Abstract
Purpose
To study the value of 3.0 T magnetic resonance imaging with intravoxel incoherent motion (IVIM) in the diagnosis of the crossed cerebellar diaschisis (CCD) after the unilateral supratentorial acute ischemic stroke.
Methods
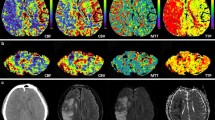
Seventy-four patients with acute ischemic stroke who underwent intravoxel incoherent motion (IVIM), arterial spin labeling (ASL), and conventional magnetic resonance imaging (MRI) scanning were enrolled. Intravoxel incoherent motion-derived perfusion-related parameters including fast diffusion coefficient (D*), slow diffusion coefficient (D), vascular volume fraction (f), and arterial spin-labeling-derived cerebral blood flow (CBF) of bilateral cerebellum were measured.
Results
In the CCD-positive group, D*, D, and CBF values of the contralateral cerebellum decreased compared with those of the ipsilesional cerebellum (P < 0.05), whereas f significantly increased (P < 0.05). A positive correlation was detected between the slow diffusion coefficient-based asymmetry index (AI-D) and the cerebral blood flow-based asymmetry index (AI-CBF) (r = 0.515, P < 0.01), whereas the vascular volume fraction-based asymmetry index (AI-f) had a negative correlation with the cerebral blood flow-based asymmetry index (AI-CBF) (r = − 0.485, P < 0.01). Furthermore, the area under the receiver operating characteristic (ROC) curve value of AI-D and AI-f was 0.81 and 0.76, respectively.
Conclusions
The IVIM is feasible for the detection of CCD. This technique might provide opportunities to further investigate the pathophysiology of CCD.




Similar content being viewed by others
Data availability
The processed data required to reproduce these findings cannot be shared at this time as the data also forms part of an ongoing study.
References
Zhang M, Cao Y, Wu F, Zhao C, Ma Q, Li K, Lu J (2020) Characteristics of cerebral perfusion and diffusion associated with crossed cerebellar diaschisis after acute ischemic stroke. Jpn J Radiol 38(2):126–134. https://doi.org/10.1007/s11604-019-00898-0
Naccarato M, Ajcevic M, Furlanis G, Lugnan C, Buoite Stella A, Scali I, Caruso P, Stragapede L, Ukmar M, Manganotti P (2020) Novel quantitative approach for crossed cerebellar diaschisis detection in acute ischemic stroke using CT perfusion. J Neurol Sci 416:117008. https://doi.org/10.1016/j.jns.2020.117008
Baron JCBM, Comar D et al (1981) Noninvasive tomographic study of cerebral blood flow and oxygen metabolism in vivo Potentials, limitations, and clinical applications in cerebral ischemic disorders. Eur Neurol 20(3):273–284
Kwon YC, Kim JH, Ahn TB (2015) Ataxia of cortical origin via crossed cerebellar diaschisis. Neurol Sci 36(1):161–163. https://doi.org/10.1007/s10072-014-1846-x
Liu X, Li J, Xu Q, Mantini D, Wang P, Xie Y, Weng Y, Ma C, Sun K, Zhang Z, Lu G (2018) Pathological factors contributing to crossed cerebellar diaschisis in cerebral gliomas: a study combining perfusion, diffusion, and structural MR imaging. Neuroradiology 60(6):643–650. https://doi.org/10.1007/s00234-018-2015-3
Reesink FE, Garcia DV, Sanchez-Catasus CA, Peretti DE, Willemsen AT, Boellaard R, Meles SK, Huitema RB, de Jong BM, Dierckx RA, De Deyn PP (2018) Crossed cerebellar diaschisis in Alzheimer’s disease. Curr Alzheimer Res 15(13):1267–1275. https://doi.org/10.2174/1567205015666180913102615
Nishioka K, Suzuki M, Satoh K, Hattori N (2018) Crossed cerebellar diaschisis in Creutzfeldt-Jakob disease evaluated through single photon emission computed tomography. J Neurol Sci 395:88–90. https://doi.org/10.1016/j.jns.2018.09.027
Joya A, Padro D, Gomez-Vallejo V, Plaza-Garcia S, Llop J, Martin A (2018) PET imaging of crossed cerebellar diaschisis after long-term cerebral ischemia in rats. Contrast Media Mol Imaging 2018:2483078. https://doi.org/10.1155/2018/2483078
Sin DS, Kim MH, Park SA, Joo MC, Kim MS (2018) Crossed cerebellar diaschisis: risk factors and correlation to functional recovery in intracerebral hemorrhage. Ann Rehabil Med 42(1):8–17. https://doi.org/10.5535/arm.2018.42.1.8
Uchino H, Kazumata K, Ito M, Nakayama N, Kuroda S, Houkin K (2020) Crossed cerebellar diaschisis as an indicator of severe cerebral hyperperfusion after direct bypass for moyamoya disease. Neurosurg Rev. https://doi.org/10.1007/s10143-020-01265-8
Lin T, Lyu Y, Qu J, Cheng X, Fan X, Zhang Y, Hou B, You H, Ma W, Feng F (2018) Crossed cerebellar diaschisis in post-treatment glioma patients: A comparative study of arterial spin labelling and dynamic susceptibility contrast. Eur J Radiol 107:70–75. https://doi.org/10.1016/j.ejrad.2018.08.001
Kang KM, Sohn CH, Kim BS, Kim YI, Choi SH, Yun TJ, Kim JH, Park SW, Cheon GJ, Han MH (2015) Correlation of asymmetry indices measured by arterial spin-labeling MR imaging and SPECT in Patients with crossed cerebellar diaschisis. AJNR Am J Neuroradiol 36(9):1662–1668. https://doi.org/10.3174/ajnr.A4366
Chen S, Guan M, Lian HJ, Ma LJ, Shang JK, He S, Ma MM, Zhang ML, Li ZY, Wang MY, Shi DP, Zhang JW (2014) Crossed cerebellar diaschisis detected by arterial spin-labeled perfusion magnetic resonance imaging in subacute ischemic stroke. J Stroke Cerebrovasc Dis 23(9):2378–2383. https://doi.org/10.1016/j.jstrokecerebrovasdis.2014.05.009
Wang J, Pan LJ, Zhou B, Zu JY, Zhao YX, Li Y, Zhu WQ, Li L, Xu JR, Chen ZA (2020) Crossed cerebellar diaschisis after stroke detected noninvasively by arterial spin-labeling MR imaging. BMC Neurosci 21(1):46. https://doi.org/10.1186/s12868-020-00595-z
Zhang CE, Wong SM, Uiterwijk R, Staals J, Backes WH, Hoff EI, Schreuder T, Jeukens CR, Jansen JF, van Oostenbrugge RJ (2017) Intravoxel incoherent motion imaging in small vessel disease: microstructural integrity and microvascular perfusion related to cognition. Stroke 48(3):658–663. https://doi.org/10.1161/STROKEAHA.116.015084
Pavilla A, Gambarota G, Arrigo A, Mejdoubi M, Duvauferrier R, Saint-Jalmes H (2017) Diffusional kurtosis imaging (DKI) incorporation into an intravoxel incoherent motion (IVIM) MR model to measure cerebral hypoperfusion induced by hyperventilation challenge in healthy subjects. MAGMA 30(6):545–554. https://doi.org/10.1007/s10334-017-0629-9
Strother MK, Buckingham C, Faraco CC, Arteaga DF, Lu P, Xu Y, Donahue MJ (2016) Crossed cerebellar diaschisis after stroke identified noninvasively with cerebral blood flow-weighted arterial spin labeling MRI. Eur J Radiol 85(1):136–142. https://doi.org/10.1016/j.ejrad.2015.11.003
Kang KM, Sohn CH, Choi SH, Jung KH, Yoo RE, Yun TJ, Kim JH, Park SW (2017) Detection of crossed cerebellar diaschisis in hyperacute ischemic stroke using arterial spin-labeled MR imaging. PLoS ONE 12(3):e0173971. https://doi.org/10.1371/journal.pone.0173971
Shinohara Y, Kato A, Kuya K, Okuda K, Sakamoto M, Kowa H, Ogawa T (2017) Perfusion MR imaging using a 3D pulsed continuous arterial spin-labeling method for acute cerebral infarction classified as branch atheromatous disease involving the lenticulostriate artery territory. AJNR Am J Neuroradiol 38(8):1550–1554. https://doi.org/10.3174/ajnr.A5247
Mozumder M, Beltrachini L, Collier Q, Pozo JM, Frangi AF (2018) Simultaneous magnetic resonance diffusion and pseudo-diffusion tensor imaging. Magn Reson Med 79(4):2367–2378. https://doi.org/10.1002/mrm.26840
Wang J, Suo S, Zu J, Zhu W, Pan L, Song S, Li Y, Li L, Chen Z, Xu J (2019) Detection of Crossed Cerebellar Diaschisis by Intravoxel Incoherent Motion MR Imaging in Subacute Ischemic Stroke. Cell Transplant 28(8):1062–1070. https://doi.org/10.1177/0963689719856290
Lin DD, Kleinman JT, Wityk RJ, Gottesman RF, Hillis AE, Lee AW, Barker PB (2009) Crossed cerebellar diaschisis in acute stroke detected by dynamic susceptibility contrast MR perfusion imaging. AJNR Am J Neuroradiol 30(4):710–715. https://doi.org/10.3174/ajnr.A1435
Wang C, Ren D, Guo Y, Xu Y, Feng Y, Zhang X, Mei Y, Chen M, Xiao X (2017) Distribution of intravoxel incoherent motion MRI-related parameters in the brain: evidence of interhemispheric asymmetry. Clin Radiol 72(1):94 e91-94 e96. https://doi.org/10.1016/j.crad.2016.09.007
Pavilla A, Arrigo A, Mejdoubi M, Duvauferrier R, Gambarota G, Saint-Jalmes H (2018) Measuring cerebral hypoperfusion induced by hyperventilation challenge with intravoxel incoherent motion magnetic resonance imaging in healthy volunteers. J Comput Assist Tomogr 42(1):85–91. https://doi.org/10.1097/RCT.0000000000000640
Wong SM, Zhang CE, van Bussel FC, Staals J, Jeukens CR, Hofman PA, van Oostenbrugge RJ, Backes WH, Jansen JF (2017) Simultaneous investigation of microvasculature and parenchyma in cerebral small vessel disease using intravoxel incoherent motion imaging. Neuroimage Clin 14:216–221. https://doi.org/10.1016/j.nicl.2017.01.017
Xu XQ, Wu CJ, Lu SS, Gao QQ, Zu QQ, Liu XL, Shi HB, Liu S (2017) Correlation between intravoxel incoherent motion magnetic resonance imaging derived metrics and serum soluble CD40 ligand level in an embolic canine stroke model. Korean J Radiol 18(5):835–843. https://doi.org/10.3348/kjr.2017.18.5.835
Federau C, Sumer S, Becce F, Maeder P, O’Brien K, Meuli R, Wintermark M (2014) Intravoxel incoherent motion perfusion imaging in acute stroke: initial clinical experience. Neuroradiology 56(8):629–635. https://doi.org/10.1007/s00234-014-1370-y
Kuai ZX, Liu WY, Zhu YM (2017) Effect of multiple perfusion components on pseudo-diffusion coefficient in intravoxel incoherent motion imaging. Phys Med Biol 62(21):8197–8209. https://doi.org/10.1088/1361-6560/aa8d0c
Wu WC, Chen YF, Tseng HM, Yang SC, My PC (2015) Caveat of measuring perfusion indexes using intravoxel incoherent motion magnetic resonance imaging in the human brain. Eur Radiol 25(8):2485–2492. https://doi.org/10.1007/s00330-015-3655-x
Suo S, Cao M, Zhu W, Li L, Li J, Shen F, Zu J, Zhou Z, Zhuang Z, Qu J, Chen Z, Xu J (2016) Stroke assessment with intravoxel incoherent motion diffusion-weighted MRI. NMR Biomed 29(3):320–328. https://doi.org/10.1002/nbm.3467
Kidani N, Hishikawa T, Hiramatsu M, Nishihiro S, Kin K, Takahashi Y, Murai S, Sugiu K, Yasuhara T, Miyazaki I, Asanuma M, Date I (2020) Cerebellar blood flow and gene expression in crossed cerebellar diaschisis after transient middle cerebral artery occlusion in rats. Int J Mol Sci 21(11). https://doi.org/10.3390/ijms21114137
Surer E, Rossi C, Becker AS, Finkenstaedt T, Wurnig MC, Valavanis A, Winklhofer S (2018) Cardiac-gated intravoxel incoherent motion diffusion-weighted magnetic resonance imaging for the investigation of intracranial cerebrospinal fluid dynamics in the lateral ventricle: a feasibility study. Neuroradiology 60(4):413–419. https://doi.org/10.1007/s00234-018-1995-3
Funding
This work was supported by the Science and Technology Innovative Development Foundation of Taian (2020NS249).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethics approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Consent to participate
Informed consent was obtained from all individual participants included in the study. Volunteers did not report discomfort during the MRI examination that lasted up to 20 min.
Consent for publication
Written informed consent for publication was obtained from all participants.
Conflicts of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Ma, J., Zhao, L., Yuan, K. et al. Crossed cerebellar diaschisis after acute ischemic stroke detected by intravoxel incoherent motion magnetic resonance imaging. Neurol Sci 43, 1135–1141 (2022). https://doi.org/10.1007/s10072-021-05425-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10072-021-05425-6