Abstract
Introduction
Systemic lupus erythematosus (SLE) is a common autoimmune disease with significant gender bias in women, and sex hormones are considered to play an important role in the regulation of immune activity. The CD45 isoforms generated through alternative splicing of mRNA identify different functional status of lymphocytes and also are suggested as a biomarker for assessing the progression of SLE, while the modulation of CD45 expression in SLE patients is not clear.
Methods
In this study, the peripheral blood sera of 46 SLE patients and 15 health individuals were collected for detecting the levels of sex hormones and immune associated factors. The expression of CD45 isoforms and the status of CD45 DNA methylation of the peripheral mononuclear blood cells were detected by flow cytometry and bisulfite sequencing PCR, respectively.
Results
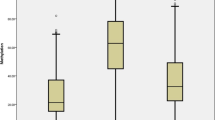
The levels of complement C3 and IgA decreased, especially decline of the serum IgA to the level of selective immunoglobulin A deficiency, and the C-reactive protein increased in SLE patients when compared with healthy controls, which manifested the abnormal immune activity of the SLE patients. Sex hormones detection showed a decreased testosterone and increased prolactin in SLE. An accelerated expression of CD45RO, reduced CD45RA and CD45RB, and a relative hypermethylation of CD45 DNA in SLE were also identified that provided a clue to explain the possible regulatory mechanism for the immune function in SLE.
Conclusion
The results indicated that the aberrant CD45 isoforms, DNA methylation and hormone levels might be correlated with the imbalanced immune activity of SLE patients.
Key Points • Selective immunoglobulin A deficiency was significantly higher in SLE than in healthy individuals. • SLE patients had decreased testosterone and increased prolactin in the sera. • An aberrant expression of CD45 isoforms and CD45 DNA methylation were identified in SLE. |


Similar content being viewed by others
Data availability
Data are available to the author group.
References
Yu C, Gershwin ME, Chang C (2014) Diagnostic criteria for systemic lupus erythematosus: a critical review. J Autoimmun 48–49:10–13. https://doi.org/10.1016/j.jaut.2014.01.004
Bengtsson AA, Rönnblom L (2017) Systemic lupus erythematosus: still a challenge for physicians. J Intern Med 281(1):52–64. https://doi.org/10.1111/joim.12529
Costa-Reis P, Sullivan KE (2013) Genetics and epigenetics of systemic lupus erythematosus. Curr Rheumatol Rep 15(9):369. https://doi.org/10.1007/s11926-013-0369-4
Deng Y, Tsao BP (2014) Advances in lupus genetics and epigenetics. Curr Opin Rheumatol 26(5):482–492. https://doi.org/10.1097/BOR.0000000000000086
Mak A, Tay SH (2014) Environmental factors, toxicants and systemic lupus erythematosus. Int J Mol Sci 15(9):16043–16056. https://doi.org/10.3390/ijms150916043
Tedeschi SK, Bermas B, Costenbader KH (2013) Sexual disparities in the incidence and course of SLE and RA. Clin Immunol 149(2):211–218. https://doi.org/10.1016/j.clim.2013.03.003
Rider V, Abdou NI, Kimler BF et al (2018) Gender bias in human systemic lupus erythematosus: a problem of steroid receptor action? Front Immunol 9:611. https://doi.org/10.3389/fimmu.2018.00611
Lahita RG (1999) The role of sex hormones in systemic lupus erythematosus. Curr Opin Rheumatol 11(5):352–356. https://doi.org/10.1097/00002281-199909000-00005
Grimaldi CM (2006) Sex and systemic lupus erythematosus: the role of the sex hormones estrogen and prolactin on the regulation of autoreactive B cells. Curr Opin Rheumatol 18(5):456–461. https://doi.org/10.1097/01.bor.0000240354.37927.dd
Moulton VR (2018) Sex hormones in acquired immunity and autoimmune disease. Front Immunol 9:2279. https://doi.org/10.3389/fimmu.2018.02279
McMurray RW (2001) Prolactin in murine systemic lupus erythematosus. Lupus 10(10):742–747. https://doi.org/10.1191/096120301717164985
Recalde G, Moreno-Sosa T, Yudica F et al (2018) Contribution of sex steroids and prolactin to the modulation of T and B cells during autoimmunity. Autoimmun Rev 17(5):504–512. https://doi.org/10.1016/j.autrev.2018.03.006
Saunders AE, Johnson P (2010) Modulation of immune cell signalling by the leukocyte common tyrosine phosphatase, CD45. Cell signal 22(3):339–348. https://doi.org/10.1016/j.cellsig.2009.10.003
Courtney AH, Shvets AA, Lu W, et al (2019) CD45 functions as a signaling gatekeeper in T cells. Sci Signal 12(604). https://doi.org/10.1126/scisignal.aaw8151
Zikherman J, Weiss A (2008) Alternative splicing of CD45: the tip of the iceberg. Immunity 2008:839–841. https://doi.org/10.1016/j.immuni.2008.12.005
Merkenschlager M, Terry L, Edwards R et al (1988) Limiting dilution analysis of proliferative responses in human lymphocyte populations defined by the monoclonal antibody UCHL1: implications for differential CD45 expression in T cell memory formation. Eur J Immunol 18(11):1653–1661. https://doi.org/10.1002/eji.1830181102
Beverley PC, Daser A, Michie CA et al (1992) Functional subsets of T cells defined by isoforms of CD45. Biochem Soc Trans 20(1):184–187. https://doi.org/10.1042/bst0200184
Hermiston ML, Xu Z, Weiss A (2003) CD45: a critical regulator of signaling thresholds in immune cells. Annu Rev Immunol 21:107–137. https://doi.org/10.1146/annurev.immunol.21.120601.140946
Silva-Neta HL, Brelaz-de-Castro MCA, Chagas MBO et al (2018) CD4(+)CD45RA(-)FOXP3(low) Regulatory T cells as potential biomarkers of disease activity in systemic lupus erythematosus Brazilian patients. Biomed Res Int 2018:3419565. https://doi.org/10.1155/2018/3419565
Rheinlander A, Schraven B, Bommhardt U (2018) CD45 in human physiology and clinical medicine. Immunol Lett 196:22–32. https://doi.org/10.1016/j.imlet.2018.01.009
Taneja V (2018) Sex hormones determine immune response. Front Immunol 9:1931. https://doi.org/10.3389/fimmu.2018.01931
Zhang T, Dong Z, Cai H et al (2020) Estradiol regulates the expression of CD45 splicing isoforms in lymphocytes. Mol Biol Rep 47(4):3025–3030. https://doi.org/10.1007/s11033-020-05373-y
Shukla S, Kavak E, Gregory M et al (2011) CTCF-promoted RNA polymerase II pausing links DNA methylation to splicing. Nature 479(7371):74–79. https://doi.org/10.1038/nature10442
Marina RJ, Sturgill D, Bailly MA et al (2016) TET-catalyzed oxidation of intragenic 5-methylcytosine regulates CTCF-dependent alternative splicing. The EMBO J 35(3):335–355. https://doi.org/10.15252/embj.201593235
Hochberg MC (1997) Updating the American College of Rheumatology revised criteria for the classification of systemic lupus erythematosus. Arthritis Rheum 40(9):1725. https://doi.org/10.1002/art.1780400928
Yel L (2010) Selective IgA deficiency. J Clin Immunol 30(1):10–16. https://doi.org/10.1007/s10875-009-9357-x
Odineal DD, Gershwin ME (2020) The epidemiology and clinical manifestations of autoimmunity in selective IgA deficiency. Clin Rev Allergy Immunol 58:107–133. https://doi.org/10.1136/ard.39.1.50
Becker GJ, Waldburger M, Hughes GR et al (1980) Value of serum C-reactive protein measurement in the investigation of fever in systemic lupus erythematosus. Ann Rheum Dis 39(1):50–52. https://doi.org/10.1136/ard.39.1.50
Hind CR, Ng SC, Feng PH et al (1985) Serum C-reactive protein measurement in the detection of intercurrent infection in Oriental patients with systemic lupus erythematosus. Ann Rheum Dis 44(4):260–261. https://doi.org/10.1136/ard.44.4.260
Feng M, Zhang SL, Liang ZJ et al (2019) Peripheral neutrophil CD64 index combined with complement, CRP, WBC count and B cells improves the ability of diagnosing bacterial infection in SLE. Lupus 28(3):304–316. https://doi.org/10.1177/0961203319827646
Ferreira RC, Pan-Hammarstrom Q, Graham RR et al (2010) Association of IFIH1 and other autoimmunity risk alleles with selective IgA deficiency. Nat Genet 42(9):777–780. https://doi.org/10.1038/ng.644
Erkocoglu M, Metin A, Kaya A et al (2017) Allergic and autoimmune disorders in families with selective IgA deficiency. Turk J Med Sci 47(2):592–598. https://doi.org/10.3906/sag-1605-50
Shkalim V, Monselize Y, Segal N et al (2010) Selective IgA deficiency in children in Israel. J Clin Immunol 30(5):761–765. https://doi.org/10.1007/s10875-010-9438-x
Zhang J, Kong W, Ni J et al (2020) The epidemiology and clinical feature of selective immunoglobulin a deficiency of Zhejiang Province in China. J Clin Lab Anal 34(10):e23440. https://doi.org/10.1002/jcla.23440
Wang W, Yao T, Zhang T et al (2020) Selective immunoglobulin A deficiency (SIgAD) primarily leads to recurrent infections and autoimmune diseases: a retrospective study of Chinese patients in the past 40 years. Genes Dis 7(1):115–121. https://doi.org/10.1016/j.gendis.2019.10.014
Klein SL, Flanagan KL (2016) Sex differences in immune responses. Nat Rev Immunol 16(10):626–638. https://doi.org/10.1038/nri.2016.90
Takahashi T, Iwasaki A (2021) Sex differences in immune responses. Science 371(6527):347–348. https://doi.org/10.1126/science.abe7199
Song GG, Lee YH (2017) Circulating prolactin level in systemic lupus erythematosus and its correlation with disease activity: a meta-analysis. Lupus 26(12):1260–1268. https://doi.org/10.1177/0961203317693094
Jara LJ, Medina G, Saavedra MA et al (2017) Prolactin has a pathogenic role in systemic lupus erythematosus. Immunol Res 65(2):512–523. https://doi.org/10.1007/s12026-016-8891-x
Lahita RG, Kunkel HG et al (1983) Increased oxidation of testosterone in systemic lupus erythematosus. Arthritis Rheum 26(12):1517–1521. https://doi.org/10.1002/art.1780261215
Robeva R, Tanev D, Andonova S et al (2013) Androgen receptor (CAG)n polymorphism and androgen levels in women with systemic lupus erythematosus and healthy controls. Rheumatol Int 33(8):2031–2038. https://doi.org/10.1007/s00296-013-2687-2
Mohr A, Atif M, Balderas R et al (2019) The role of FOXP3(+) regulatory T cells in human autoimmune and inflammatory diseases. Clin Exp Immunol 197(1):24–35. https://doi.org/10.1111/cei.13288
Singh RP, Bischoff DS (2021) Sex hormones and gender influence the expression of markers of regulatory T cells in SLE patients. Front Immunol 12:619268. https://doi.org/10.3389/fimmu.2021.619268
Chang VT, Fernandes RA, Ganzinger KA et al (2016) Initiation of T cell signaling by CD45 segregation at “close contacts.” Nat Immunol 17(5):574–582. https://doi.org/10.1038/ni.3392
Javierre BM, Fernandez AF, Richter J et al (2010) Changes in the pattern of DNA methylation associate with twin discordance in systemic lupus erythematosus. Genome Res 20(2):170–179. https://doi.org/10.1101/gr.100289.109
Imgenberg-Kreuz J, Carlsson Almlof J, Leonard D et al (2018) DNA methylation mapping identifies gene regulatory effects in patients with systemic lupus erythematosus. Ann Rheum Dis 77(5):736–743. https://doi.org/10.1136/annrheumdis-2017-212379
Su Z, Liu G, Zhang B, et al (2021) Natural antisense transcript PEBP1P3 regulates the RNA expression, DNA methylation and histone modification of CD45 gene. Genes 12(5). https://doi.org/10.3390/genes12050759
Funding
This work was supported by the grants from National Natural Science Foundation of China (No. 31870745) and Natural Science Foundation of Guangdong Province, China (No. 2018A0303130153).
Author information
Authors and Affiliations
Contributions
All authors made substantial contributions to the conception of the work or the acquisition, analysis, or interpretation of data. All authors approved the submitted version of the manuscript.
Corresponding authors
Ethics declarations
Consent to participate
Informed consent was obtained from all subjects enrolled in the study.
Consent for publication
Informed consent was obtained from all subjects enrolled in the study.
Disclosures
None.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Zhaoxia Dong and Bin Zhang contributed equally to this work.
Rights and permissions
About this article
Cite this article
Dong, Z., Zhang, B., Rong, J. et al. The aberrant expression of CD45 isoforms and levels of sex hormones in systemic lupus erythematosus. Clin Rheumatol 41, 1087–1093 (2022). https://doi.org/10.1007/s10067-021-05934-x
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10067-021-05934-x