Abstract
Study design
Meta-analysis.
Objective
To conduct a meta-analysis investigating the relationship between spinopelvic alignment parameters and development of adjacent level disease (ALD) following lumbar fusion for degenerative disease.
Summary of background data
ALD is a degenerative pathology that develops at mobile segments above or below fused spinal segments. Patient outcomes are worse, and the likelihood of requiring revision surgery is higher in ALD compared to patients without ALD. Spinopelvic sagittal alignment has been found to have a significant effect on outcomes post-fusion; however, studies investigating the relationship between spinopelvic sagittal alignment parameters and ALD in degenerative lumbar disease are limited.
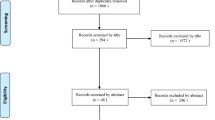
Methods
Six e-databases were searched. Predefined endpoints were extracted and meta-analyzed from the identified studies.
Results
There was a significantly larger pre-operative PT in the ALD cohort versus control (WMD 3.99, CI 1.97–6.00, p = 0.0001), a smaller pre-operative SS (WMD − 2.74; CI − 5.14 to 0.34, p = 0.03), and a smaller pre-operative LL (WMD − 4.76; CI − 7.66 to 1.86, p = 0.001). There was a significantly larger pre-operative PI-LL in the ALD cohort (WMD 8.74; CI 3.12–14.37, p = 0.002). There was a significantly larger postoperative PI in the ALD cohort (WMD 2.08; CI 0.26–3.90, p = 0.03) and a larger postoperative PT (WMD 5.23; CI 3.18–7.27, p < 0.00001).
Conclusion
The sagittal parameters: PT, SS, PI-LL, and LL may predict development of ALD in patients’ post-lumbar fusion for degenerative disease. Decision-making aimed at correcting these parameters may decrease risk of developing ALD in this cohort.
Graphical abstract
These slides can be retrieved under Electronic Supplementary Material.




Similar content being viewed by others
Change history
13 October 2021
A Correction to this paper has been published: https://doi.org/10.1007/s00586-021-07000-1
References
Lotz JC, Haughton V, Boden SD et al (2012) New treatments and imaging strategies in degenerative disease of the intervertebral disks. Radiology 264:6–19
Mobbs RJ, Phan K, Malham G et al (2015) Lumbar interbody fusion: techniques, indications and comparison of interbody fusion options including PLIF, TLIF, MI-TLIF, OLIF/ATP, LLIF and ALIF. J Spine Surg (Hong Kong) 1:2–18
Mobbs RJ, Phan K, Daly D et al (2016) Approach-related complications of anterior lumbar interbody fusion: results of a combined spine and vascular surgical team. Glob Spine J 6:147–154
Phan K, Lee NJ, Kothari P et al (2016) Risk factors for readmissions following anterior lumbar interbody fusion. Spine 43:364–369
Rao PJ, Ghent F, Phan K et al (2015) Stand-alone anterior lumbar interbody fusion for treatment of degenerative spondylolisthesis. J Clin Neurosci 22:1619–1624
Phan K, Thayaparan GK, Mobbs RJ (2015) Anterior lumbar interbody fusion versus transforaminal lumbar interbody fusion–systematic review and meta-analysis. Br J Neurosurg 29:705–711
Di Capua J, Somani S, Kim JS et al (2017) Analysis of risk factors for major complications following elective posterior lumbar fusion. Spine 42:1347–1354
Lee NJ, Kothari P, Phan K et al (2016) The incidence and risk factors for 30-day unplanned readmissions after elective posterior lumbar fusion. Spine 43:41–48
Phan K, Rao PJ, Scherman DB et al (2015) Lateral lumbar interbody fusion for sagittal balance correction and spinal deformity. J Clin Neurosci 22:1714–1721
Rajaee SS, Bae HW, Kanim LE et al (2012) Spinal fusion in the United States: analysis of trends from 1998 to 2008. Spine 37:67–76
Yelin E, Weinstein S, King T (2016) The burden of musculoskeletal diseases in the United States. Semin Arthritis Rheum 46:259–260
Davies M (2013) Where the United States Spends its Spine Dollars: expenditures on different ambulatory services for the management of back and neck conditions. Spine 37(19):1693–1701
Hilibrand AS, Robbins M (2004) Adjacent segment degeneration and adjacent segment disease: the consequences of spinal fusion? Spine J 4:190S–194S
Yang SW, Langrana NA, Lee CK (1986) Biomechanics of lumbosacral spinal fusion in combined compression-torsion loads. Spine 11:937–941
Lee CK (1988) Accelerated degeneration of the segment adjacent to a lumbar fusion. Spine 13:375–377
Bresnahan L, Ogden AT, Natarajan RN et al (2009) A biomechanical evaluation of graded posterior element removal for treatment of lumbar stenosis: comparison of a minimally invasive approach with two standard laminectomy techniques. Spine 34:17–23
Regev GJ, Lee YP, Taylor WR et al (2009) Nerve injury to the posterior rami medial branch during the insertion of pedicle screws: comparison of mini-open versus percutaneous pedicle screw insertion techniques. Spine 34:1239–1242
Battie MC, Videman T, Kaprio J et al (2009) The Twin Spine Study: contributions to a changing view of disc degeneration. Spine J 9:47–59
Kim DY, Lee SH, Chung SK et al (2005) Comparison of multifidus muscle atrophy and trunk extension muscle strength: percutaneous versus open pedicle screw fixation. Spine 30:123–129
Lee JC, Choi S-W (2015) Adjacent segment pathology after lumbar spinal fusion. Asian Spine J 9:807–817
Harrop JS, Youssef JA, Maltenfort M et al (2008) Lumbar adjacent segment degeneration and disease after arthrodesis and total disc arthroplasty. Spine 33:1701–1707
Schwab FJ, Blondel B, Bess S et al (2013) Radiographical spinopelvic parameters and disability in the setting of adult spinal deformity: a prospective multicenter analysis. Spine 38:E803–E812
Djurasovic MO, Carreon LY, Glassman SD et al (2008) Sagittal alignment as a risk factor for adjacent level degeneration: a case-control study. Orthopedics 31:546
Radcliff KE, Kepler CK, Jakoi A et al (2013) Adjacent segment disease in the lumbar spine following different treatment interventions. Spine J 13:1339–1349
Moher D, Liberati A, Tetzlaff J et al (2009) Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med 6:e1000097
Phan K, Tian DH, Cao C et al (2015) Systematic review and meta-analysis: techniques and a guide for the academic surgeon. Anna Cardiothorac Surg 4:112–122
Phan K, Mobbs RJ (2015) Systematic reviews and meta-analyses in spine surgery, neurosurgery and orthopedics: guidelines for the surgeon scientist. J Spine Surg 1:19–27
Cole T-C, Ghosh P, Hannan NJ et al (1987) The response of the canine intervertebral disc to immobilization produced by spinal arthrodesis is dependent on constitutional factors. J Orthop Res 5:337–347
Lee CK, Langrana NA (1984) Lumbosacral spinal fusion. A biomechanical study. Spine 9:574–581
Cole T-C, Burkhardt D, Ghosh P et al (1985) Effects of spinal fusion on the proteoglycans of the canine intervertebral disc. J Orthop Res 3:277–291
Cheh G, Bridwell KH, Lenke LG et al (2007) Adjacent segment disease following lumbar/thoracolumbar fusion with pedicle screw instrumentation. Spine 32:2253–2257
Mok JM, Cloyd JM, Bradford DS et al (2009) Reoperation after primary fusion for adult spinal deformity: rate, reason, and timing. Spine 34:832–839
Sears WR, Sergides IG, Kazemi N et al (2011) Incidence and prevalence of surgery at segments adjacent to a previous posterior lumbar arthrodesis. Spine J 11:11–20
Di Martino A, Quattrocchi CC, Scarciolla L et al (2014) Estimating the risk for symptomatic adjacent segment degeneration after lumbar fusion: analysis from a cohort of patients undergoing revision surgery. Eur Spine J 23(Suppl 6):693–698
Kumar MN, Baklanov A, Chopin D (2001) Correlation between sagittal plane changes and adjacent segment degeneration following lumbar spine fusion. Eur Spine J 10:314–319
Umehara S, Zindrick MR, Patwardhan AG et al (2000) The biomechanical effect of postoperative hypolordosis in instrumented lumbar fusion on instrumented and adjacent spinal segments. Spine 25:1617–1624
Oda I, Cunningham BW, Buckley RA et al (1999) Does spinal kyphotic deformity influence the biomechanical characteristics of the adjacent motion segments? An in vivo animal model. Spine 24:2139–2146
Barrey C, Roussouly P, Perrin G et al (2011) Sagittal balance disorders in severe degenerative spine. Can we identify the compensatory mechanisms? Eur Spine J 20(Suppl 5):626–633
Roussouly P, Pinheiro-Franco JL (2011) Biomechanical analysis of the spino-pelvic organization and adaptation in pathology. Eur Spine J 20(Suppl 5):609–618
Senteler M, Weisse B, Snedeker JG et al (2014) Pelvic incidence-lumbar lordosis mismatch results in increased segmental joint loads in the unfused and fused lumbar spine. Eur Spine J 23:1384–1393
Akamaru T, Kawahara N, Tim Yoon S et al (2003) Adjacent segment motion after a simulated lumbar fusion in different sagittal alignments: a biomechanical analysis. Spine 28:1560–1566
Kim KH, Lee SH, Shim CS et al (2010) Adjacent segment disease after interbody fusion and pedicle screw fixations for isolated L4-L5 spondylolisthesis: a minimum five-year follow-up. Spine 35:625–634
Hsieh PC, Koski TR, O’Shaughnessy BA et al (2007) Anterior lumbar interbody fusion in comparison with transforaminal lumbar interbody fusion: implications for the restoration of foraminal height, local disc angle, lumbar lordosis, and sagittal balance. J Neurosurg Spine 7:379–386
Pavlov PW, Meijers H, van Limbeek J et al (2004) Good outcome and restoration of lordosis after anterior lumbar interbody fusion with additional posterior fixation. Spine 29:1893–1899 (discussion 900)
Rao PJ, Maharaj MM, Phan K et al (2015) Indirect foraminal decompression after anterior lumbar interbody fusion: a prospective radiographic study using a new pedicle-to-pedicle technique. Spine J 15:817–824
Lee N, Kim KN, Yi S et al (2017) Comparison of outcomes of anterior-, posterior- and transforaminal lumbar interbody fusion surgery at a single lumbar level with degenerative spinal disease. World Neurosurg 101:216–226
Sembrano JN, Yson SC, Horazdovsky RD et al (2015) Radiographic comparison of lateral lumbar interbody fusion versus traditional fusion approaches: analysis of sagittal contour change. Int J Spine Surg 9:16
Malham GM, Parker RM, Blecher CM et al (2016) Choice of approach does not affect clinical and radiologic outcomes: a comparative cohort of patients having anterior lumbar interbody fusion and patients having lateral lumbar interbody fusion at 24 months. Glob Spine J 6:472–481
Challier V, Boissiere L, Obeid I et al (2016) One-level lumbar degenerative spondylolisthesis and posterior approach. is transforaminal lateral interbody fusion mandatory? A randomized controlled trial with two year follow-up. Spine 42(8):531–539
Levin JM, Alentado VJ, Healy AT et al (2017) Superior segment facet joint violation during instrumented lumbar fusion is associated with higher reoperation rates and diminished improvement in quality of life. Clin Spine Surg. https://doi.org/10.1097/BSD.0000000000000566
Lee CH, Kim YE, Lee HJ et al (2017) Biomechanical effects of hybrid stabilization on the risk of proximal adjacent-segment degeneration following lumbar spinal fusion using an interspinous device or a pedicle screw-based dynamic fixator. J Neurosurg Spine 22:1–7. https://doi.org/10.3171/2017.3.SPINE161169
Cecchinato R, Redaelli A, Martini C et al (2017) Long fusions to S1 with or without pelvic fixation can induce relevant acute variations in pelvic incidence: a retrospective cohort study of adult spine deformity surgery. Eur Spine J. https://doi.org/10.1007/s00586-017-5154-z
Lee JH, Na KH, Kim JH et al (2016) Is pelvic incidence a constant, as everyone knows? Changes of pelvic incidence in surgically corrected adult sagittal deformity. Eur Spine J 25(11):3707–3714
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors have no conflicts of interest to disclose.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Phan, K., Nazareth, A., Hussain, A.K. et al. Relationship between sagittal balance and adjacent segment disease in surgical treatment of degenerative lumbar spine disease: meta-analysis and implications for choice of fusion technique. Eur Spine J 27, 1981–1991 (2018). https://doi.org/10.1007/s00586-018-5629-6
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00586-018-5629-6