Abstract
Background
The impact of paranasal sinusitis on the clinical outcome of patients with cancer remains unknown. The aim of this study was to determine whether paranasal sinusitis at the initiation of chemotherapy (SAI) affects the development of infectious complications in children and adolescents with cancer.
Methods
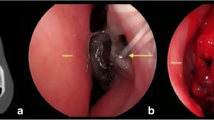
A retrospective cohort analysis of patients aged 0-20 years with cancer who received chemotherapy was performed. SAI was defined as the presence of a fluid level or mucosal swelling or total opacity on sinus computed tomography examination before the initiation of chemotherapy. The primary outcome measures were the incidence of bacteremia, septic shock, and invasive fungal disease (IFD, including proven, probable, and possible cases).
Results
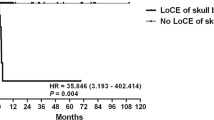
SAI was observed in 57 (44%) of 130 enrolled patients. There were no significant differences in age, sex, and disease distribution between the patients with SAI (SAI group) and those without (non-SAI group). There was no significant difference in the 1-year cumulative incidence of bacteremia or septic shock after treatment initiation between the two groups (bacteremia, SAI group 33% vs. non-SAI group 35%, P = 0.53; septic shock, SAI group 4% vs. non-SAI group 4%, P = 0.87). The 1-year cumulative incidence of IFD was higher in the SAI group than in the non-SAI group (22% vs. 6%, P = 0.012). Cumulative incidence analysis after inverse probability of treatment weighting adjustment showed that the SAI group was more likely to develop IFD (HR: 3.5, 95% CI: 1.1-11.2, P = 0.033).
Conclusions
Our findings suggest that patients with SAI may be at higher risk for IFD during chemotherapy.

Similar content being viewed by others
References
Zembower TR (2014) Epidemiology of infections in cancer patients. Cancer Treat Res:161.43–161.89
Mikulska M, Viscoli C, Orasch C, Livermore DM, Averbuch D, Cordonnier C, Akova M (2014) Aetiology and resistance in bacteraemias among adult and paediatric haematology and cancer patients. J Inf Secur 68:321–331
Montassier E, Batard E, Gastinne T, Potel G, Cochetière MF (2013) Recent changes in bacteremia in patients with cancer: A systematic review of epidemiology and antibiotic resistance. Eur J Clin Microbiol Infect Dis 32:841–850
Valentine JC, Morrissey CO, Tacey MA, Liew D, Patil S, Peleg AY, Ananda-Rajah MR (2019) A population-based analysis of invasive fungal disease in haematology-oncology patients using data linkage of state-wide registries and administrative databases: 2005-2016. BMC Infect Dis 19:274
Pana ZD, Roilides E, Warris A, Groll AH, Zaoutis T (2017) Epidemiology of invasive fungal disease in children. J Pediatric Infect Dis Soc 6:S3–S11
Thom KA, Kleinberg M, Roghmann MC (2013) Infection prevention in the cancer center. Clin Infect Dis 57:579–585
Taplitz RA, Kennedy EB, Bow EJ, Crews J, Gleason C, Hawley DK, Langston AA, Nastoupil LJ, Rajotte M, Rolston KV, Strasfeld L, Flowers CR (2018) Antimicrobial prophylaxis for adult patients with cancer-related immunosuppression: ASCO and IDSA clinical practice guideline update. J Clin Oncol 36:3043–3054
Lehrnbecher T, Robinson P, Fisher B, Alexander S, Ammann RA, Beauchemin M, Carlesse F, Groll AH, Haeusler GM, Santolaya M, Steinbach WJ, Castagnola E, Davis BL, Dupuis LL, Gaur AH, Tissing WJE, Zaoutis T, Phillips R, Sung L (2017) Guideline for the management of fever and neutropenia in children with cancer and hematopoietic stem-cell transplantation recipients: 2017 Update. J Clin Oncol 35:2082–2094
Stevens WW, Lee RJ, Schleimer RP, Cohen NA (2015) Chronic rhinosinusitis pathogenesis. J Allergy Clin Immunol 136:1442–1453
Khalmuratova R, Park JW, Shin HW. Immune cell responses and mucosal barrier disruptions in chronic rhinosinusitis. Immune Netw 2017;17:60-67.
Goytia VK, Giannoni CM, Edwards MS (2011) Intraorbital and intracranial extension of sinusitis: Comparative morbidity. J Pediatr 158:486–491
Kishimoto K, Kobayashi R, Hori D, Sano H, Suzuki D, Yasuda K, Kobayashi K (2016) Pretransplant paranasal sinus disease is associated with a high incidence of transplant-related mortality in hematopoietic stem cell transplantation for children and adolescents. Pediatr Transplant 20:1111–1116
Okuyemi KS, Tsue TT (2002) Radiologic imaging in the management of sinusitis. Am Fam Physician 66:1882–1886
De Pauw B, Walsh TJ, Donnelly JP et al (2008) Revised definitions of invasive fungal disease from the European Organization for Research and Treatment of Cancer/Invasive Fungal Infections Cooperative Group and the National Institute of Allergy and Infectious Diseases Mycoses Study Group (EORTC/MSG) Consensus Group. Clin Infect Dis 46:1813–1821
Austin PC (2011) An introduction to propensity score methods for reducing the effects of confounding in observational studies. Multivar Behav Res 46:399–424
Austin PC, Stuart EA (2015) Moving towards best practice when using inverse probability of treatment weighting (IPTW) using the propensity score to estimate causal treatment effects in observational studies. Stat Med 34:3661–3679
Neumann A, Billionnet C (2016) Covariate adjustment of cumulative incidence functions for competing risks data using inverse probability of treatment weighting. Comput Methods Prog Biomed 129:63–70
Wald ER, Guerra N, Byers C (1991) Upper respiratory tract infections in young children: duration of and frequency of complications. Pediatrics. 87:129–133
Marom T, Alvarez-Fernandez PE, Jennings K, Patel JA, McCormick DP, Chonmaitree T (2014) Acute bacterial sinusitis complicating viral upper respiratory tract infection in young children. Pediatr Infect Dis J 33:803–808
DeMuri GP, Gern JE, Moyer SC et al (2016) Clinical features, virus identification, and sinusitis as a complication of upper respiratory tract illness in children ages 4-7 years. J Pediatr 171:133–9.e1
Beule A (2015) Epidemiology of chronic rhinosinusitis, selected risk factors, comorbidities, and economic burden. GMS Curr Top Otorhinolaryngol Head Neck Surg 14:Doc11
Shi JB, Fu QL, Zhang H, Cheng L, Wang YJ, Zhu DD, Lv W, Liu SX, Li PZ, Ou CQ, Xu G (2015) Epidemiology of chronic rhinosinusitis: results from a cross-sectional survey in seven Chinese cities. Allergy. 70:533–539
Jones NS (2002) CT of the paranasal sinuses: a review of the correlation with clinical, surgical and histopathological findings. Clin Otolaryngol Allied Sci 27:11–17
Havas TE, Motbey JA, Gullane PJ (1988) Prevalence of incidental abnormalities on computed tomographic scans of the paranasal sinuses. Arch Otolaryngol Head Neck Surg 114:856–859
Tarp B, Fiirgaard B, Christensen T, Jensen JJ, Black FT (2000) The prevalence and significance of incidental paranasal sinus abnormalities on MRI. Rhinology. 38:33–38
Hansen AG, Helvik AS, Nordgard S et al (2014) Incidental findings in MRI of the paranasal sinuses in adults: A population-based study (HUNT MRI). BMC Ear Nose Throat Disord 14:13
Thompson GR, Patterson TF (2012) Fungal disease of the nose and paranasal sinuses. J Allergy Clin Immunol 129:321–326
Kim ST, Choi JH, Jeon HG, Cha HE, Hwang YJ, Chung YS (2005) Comparison between polymerase chain reaction and fungal culture for the detection of fungi in patients with chronic sinusitis and normal controls. Acta Otolaryngol 125:72–75
Murr AH, Goldberg AN, Vesper S (2006) Fungal speciation using quantitative polymerase chain reaction (QPCR) in patients with and without chronic rhinosinusitis. Laryngoscope. 116:1342–1348
Tieu DD, Kern RC, Schleimer RP (2009) Alterations in epithelial barrier function and host defense responses in chronic rhinosinusitis. J Allergy Clin Immunol 124:37–42
Ramanathan M Jr, Lee WK, Dubin MG, Lin S, Spannhake EW, Lane AP (2007) Sinonasal epithelial cell expression of toll-like receptor 9 is decreased in chronic rhinosinusitis with polyps. Am J Rhinol 21:110–116
Schleimer RP, Kato A, Kern R, Kuperman D, Avila PC (2007) Epithelium: at the interface of innate and adaptive immune responses. J Allergy Clin Immunol 120:1279–1284
Hellings PW, Hens G (2009) Rhinosinusitis and the lower airways. Immunol Allergy Clin N Am 29:733–740
Hellings PW, Prokopakis EP (2010) Global airway disease beyond allergy. Curr Allergy Asthma Rep 10:143–149
Gudis D, Zhao KQ, Cohen NA (2012) Acquired cilia dysfunction in chronic rhinosinusitis. Am J Rhinol Allergy 26:1–6
Hochhegger B, Alves GRT, Irion KL et al (2015) Computed tomographic pulmonary changes in patients with chronic rhinosinusitis. Br J Radiol 88:20150273
Kobayashi R, Kaneda M, Sato T, Ichikawa M, Suzuki D, Ariga T (2008) The clinical feature of invasive fungal infection in pediatric patients with hematologic and malignant diseases: a 10-year analysis at a single institution at Japan. J Pediatr Hematol Oncol 30:886–890
Mor M, Gilad G, Kornreich L, Fisher S, Yaniv I, Levy I (2011) Invasive fungal infections in pediatric oncology. Pediatr Blood Cancer 56:1092–1097
Groll AH, Castagnola E, Cesaro S, Dalle JH, Engelhard D, Hope W, Roilides E, Styczynski J, Warris A, Lehrnbecher T, Fourth European Conference on Infections in Leukaemia, Infectious Diseases Working Party of the European Group for Blood Marrow Transplantation (EBMT-IDWP), Infectious Diseases Group of the European Organisation for Research and Treatment of Cancer (EORTC-IDG), International Immunocompromised Host Society (ICHS), European Leukaemia Net (ELN) (2014) Fourth European conference on infections in leukaemia (ECIL-4): Guidelines for diagnosis, prevention, and treatment of invasive fungal diseases in paediatric patients with cancer or allogeneic haemopoietic stem-cell transplantation. Lancet Oncol 15:e327–e340
Kobayashi R, Hori D, Sano H, Suzuki D, Kishimoto K, Kobayashi K (2018) Risk factors for invasive fungal infection in children and adolescents with hematologic and malignant diseases: A 10-year analysis in a single institute in Japan. Pediatr Infect Dis J 37:1282–1285
Lorkiewicz-Muszynska D, Kociemba W, Rewekant A et al (2015) Development of the maxillary sinus from birth to age 18. Postnatal growth pattern. Int J Pediatr Otorhinolaryngol 79:1393–1400
Degermenci M, Ertekin T, Ulger H et al (2016) The age-related development of maxillary sinus in children. J Craniofac Surg 27:e38–e44
Gilani S, Shin JJ (2017) The burden and visit prevalence of pediatric chronic rhinosinusitis. Otolaryngol Head Neck Surg 157:1048–1052
Deshazo RD (2009) Syndromes of invasive fungal sinusitis. Med Mycol 47:S309–S314
Singh V (2019) Fungal rhinosinusitis: Unravelling the disease spectrum. J Maxillofac Oral Surg 18:164–179
Data and materials availability
The datasets analyzed during the current study available from the corresponding author on reasonable request.
Author information
Authors and Affiliations
Contributions
Kenji Kishimoto and Ryoji Kobayashi contributed to study conception and design. Kenji Kishimoto, Daiki Hori, Satoru Matsushima, Masato Yanagi, Hirozumi Sano, and Daisuke Suzuki collected the data. Kenji Kishimoto and Ryoji Kobayashi performed the analysis and interpretation of data. Kenji Kishimoto drafted the manuscript. Ryoji Kobayashi and Kunihiko Kobayashi edited and made critical revision to the manuscript. All the authors contributed to the final manuscript.
Corresponding author
Ethics declarations
Ethics approval
This study was approved by the Institutional Review Board of Sapporo Hokuyu Hospital.
Conflicts of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Supplemental Figure 1
Patient enrollment process. CT, computed tomography (PNG 10 kb)
ESM 2
(DOCX 23 kb)
Rights and permissions
About this article
Cite this article
Kishimoto, K., Kobayashi, R., Hori, D. et al. Paranasal sinusitis at the initiation of chemotherapy is a risk factor for invasive fungal disease in children and adolescents with cancer. Support Care Cancer 29, 5847–5852 (2021). https://doi.org/10.1007/s00520-021-06143-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00520-021-06143-7