Abstract
Purpose
Weight loss and poor food intake have been shown to affect several outcomes in patients undergoing surgery for gastrointestinal cancer. This review aims to examine the effect of pre-, post- or perioperative nutrition interventions focused on increasing oral energy or protein intake in patients undergoing surgery for gastrointestinal cancer. Interventions using standard oral nutrition supplements and/or dietary counselling were included. The primary outcome was weight change, and secondary outcomes were energy and protein intake. A secondary aim was to examine this effect in malnourished patients.
Methods
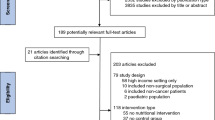
Embase, Medline, CINAHL and CENTRAL were searched from inception to September 2019 for relevant randomised controlled trials. Study quality was assessed using the revised Cochrane Collaboration risk of bias tool for randomised trials. The quality of evidence for each outcome was assessed using GRADE.
Results
Fourteen articles met the inclusion criteria. Studies assessed patients undergoing surgery for gastric, colorectal, oesophageal and pancreatic cancers. The interventions studied included oral nutrition supplements and/or dietary counselling. Five studies reported preoperative interventions; five studies reported post-operative interventions; six studies reported post-discharge interventions; and two studies reported perioperative interventions. Overall, low or very low quality evidence was found to support the use of oral nutrition supplements to positively influence weight and increase energy and protein intake in the preoperative period and immediate post-operative period. Very low quality evidence was found to support the use of oral nutrition interventions to influence weight, energy or protein intake in the post-discharge period. Very limited evidence with high risk of bias was found to support positive effects of nutrition intervention in malnourished patients.
Conclusions
This review demonstrates limited evidence for the use of oral nutrition supplements to increase intake and positively influence weight in patients undergoing surgery for gastrointestinal cancer. Overall, results were heterogeneous leading to inconsistent results. Further research into optimal nutrition support interventions and timing of interventions is required.

Similar content being viewed by others
Availability of data and material
Not applicable
References
Bray F, Ferlay J, Soerjomataram I, Siegel RL, Torre L, Jemal A (2018) Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin 68(6):394–424
Allum W, Lordick F, Alsina M, Andritsch E, Ba-Ssalamah A, Beishon M, Braga M, Caballero C, Carneiro F, Cassinello F, Dekker JW, Delgado-Bolton R, Haustermans K, Henning G, Hutter B, Lövey J, Netíková IŠ, Obermannová R, Oberst S, Rostoft S, Saarto T, Seufferlein T, Sheth S, Wynter-Blyth V, Costa A, Naredi P (2018) ECCO essential requirements for quality cancer care: oesophageal and gastric cancer. Crit Rev Oncol Hematol 122:179–193
Van Cutsem E, Arends J (2005) The causes and consequences of cancer-associated malnutrition. Eur J Oncol Nurs 9(S2):S51–S63
Arends J, Baracos V, Bertz H, Bozzetti F, Calder PC et al (2017) ESPEN guidelines on nutrition in cancer patients. Clin Nutr 36(1):11–48
Marin Caro MM, Laviano A, Pichard C (2007) Impact of nutrition on quality of life during cancer. Curr Opin Clin Nutr Metab Care 10(4):480–487
Garth AK, Newsome CM, Simmance N, Crow TC (2010) Nutritional status, nutrition practices and post-operative complications in patients with gastrointestinal cancer. J Hum Nutr Diet 23(4):393–401
Mosquera C, Koutlas NJ, Edwards KC, Strickland A, Vohra NA, Zervos EE, Fitzgerald TL (2016) Impact of malnutrition on gastrointestinal surgical patients. J Surg Res 205(1):95–101
Sungurtekin H, Sungertekin U, Balci C, Zencir M, Erdem E (2004) The influence of nutritional status on complications after major intraabdominal surgery. J Am Coll Nutr 23(3):227–232
Liu X, Xu P, Qiu H, Xu D, Li W, Zhan Y, Li Y, Chen Y, Zhou Z, Sun X (2016) Preoperative nutritional deficiency is a useful predictor of postoperative outcome in patients undergoing curative resection for gastric cancer. Transl Oncol 9(6):482–488
Hill A, Kiss N, Hodgson CTC, Walsh AD (2011) Associations between nutritional status, weight loss, radiotherapy treatment toxicity and treatment outcomes in gastrointestinal cancer patients. Clin Nutr 30(1):92–98
Lobo DN, Gianotti L, Adiamah A, Barazzoni R, Deutz DK et al (2020) Perioperative nutrition: recommendations from the ESPEN expert group. Clin Nutr. https://doi.org/10.1016/j.clnu.2020.03.038
Weimann A, Braga M, Carli F, Higashiguchi T, Hubner M et al (2017) ESPEN guideline: clinical nutrition in surgery. Clin Nutr 36(3):623–650
Barlow R, Price P, Reid TD, Hunt S, Clark GW, Havard TJ, Puntis MC, Lewis WG (2011) Prospective multicentre randomised controlled trial of early enteral nutrition for patients undergoing major upper gastrointestinal surgical resection. Clin Nutr 30(5):560–566
Jin Y, Yong C, Ren K, Li D, Yuan H (2018) Effects of post-surgical parenteral nutrition on patients with gastric cancer. Cell Physiol Biochem 49(4):1320–1328
Burden ST, Gibson DJ, Lal S, Hill J, Pilling M, Soop M, Ramesh A, Todd C (2017) Pre-operative oral nutritional supplementation with dietary advice versus dietary advice alone in weight-losing patients with colorectal cancer: single-blind randomized controlled trial. J Cachexia Sarcopenia Muscle 8(3):437–446
Kong SH, Lee HJ, Na JR, Kim WG, Han DS, Park SH, Hong H, Choi Y, Ahn HS, Suh YS, Yang HK (2018) Effect of perioperative oral nutritional supplementation in malnourished patients who undergo gastrectomy: a prospective randomized trial. Surgery 164(6):1263–1270
Carey S, Ferrie S, Ryan R, Beaton J, Young J, Allman-Farinelle M (2013) Long-term nutrition intervention following major upper gastrointestinal surgery: a prospective randomized controlled trial. Eur J Clin Nutr 67(4):324–329
Kim H, Suh EE, Lee HJ, Yang HK (2014) The effects of patient participation-based dietary intervention on nutritional and functional status for patients with gastrectomy: a randomized controlled trial. Cancer Nurs 37(2):E10–E20
van Noort HHJ, Ettema RGA, Vermeulen H, Huisman-de Waal G, Basic Care Revisited Group (2019) Outpatient preoperative oral nutritional support for undernourished surgical patients: a systematic review. J Clin Nurs 28(1–2):7–19
Burden S, Todd C, Hill J, Lal S (2012) Pre-operative nutrition support in patients undergoing gastrointestinal surgery. Cochrane Database Syst Rev 11:CD008879
Zhang B, Najarali Z, Ruo L, Alhusaini A, Solis N, Valencia M, Sanchez MIP, Serrano PE (2019) Effect of perioperative nutritional supplementation on postoperative complications-systematic review and meta-analysis. J Gastrointest Surg 23(8):1682–1693
Crickmer M, Dunne CP, O’Regan A, Coffey JC, Dunne SS (2016) Benefits of post-operative oral protein supplementation in gastrointestinal surgery patients: a systematic review of clinical trials. World J Gastrointest Surg 8(7):521–532
Lidder PG, Lewis S, Duxbury M, Thomas S (2009) Systematic review of post discharge oral nutritional supplementation in patients undergoing GI surgery. Nutr Clin Pract 24(3):388–394
Imamura H, Nishikawa K, Kishi K, Inoue K, Matsuyama J, Akamaru Y, Kimura Y, Tamura S, Kawabata R, Kawada J, Fujiwara Y, Kawase T, Fukui J, Takagi M, Takeno A, Shimokawa T (2016) Effects of an oral elemental nutritional supplement on post-gastrectomy body weight loss in gastric cancer patients: a randomized controlled clinical trial. Ann Surg Oncol 23(9):2928–2935
Zhu MW, Yang X, Xiu DR, Yang Y, Li GX et al (2019) Effect of oral nutritional supplementation on the post-discharge nutritional status and quality of life of gastrointestinal cancer patients after surgery: a multi-center study. Asia Pac J Clin Nutr 28(3):450–456
Kong SH, Park JS, Lee IK, Ryu SW, Park YK, Yang HK, Han SU, Yoon KY, Jeong SY, Jeong MR, Hwang DW, Suh YS, Yoon YS, Seo KW, Park JW, Byun CS, Hur H, Won H, Choi Y, Lee HJ (2017) Postoperative oral nutritional supplementation after major gastrointestinal surgery: a randomized controlled clinical trial. Asia Pac J Clin Nutr 26(5):811–819
Burden ST, Hill J, Shaffer JL, Todd C (2010) Nutritional status of preoperative colorectal cancer patients. J Hum Nutr Diet 23(4):402–407
Grace EM, Shaw C, Lalji A, Mohammed K, Andreyev A, Whelan K (2018) Nutritional status, the development and persistence of malnutrition and dietary intake in oesophago-gastric cancer: a longitudinal cohort study. J Hum Nutr Diet 31:785–792
Marshall KM, Loeliger J, Nolte L, Kelaart A, Kiss NK (2019) Prevalence of malnutrition and impact on clinical outcomes in cancer services: a comparison of two time points. Clin Nutr 38:644–651
Baldwin C, McGough C, Spiro A, Thomas K, Cunningham DC, Andreyev HJN (2009) Nutritional and clinical characteristics of patients with gastrointestinal tract (GI) cancers at presentation. Proc Nutr Soc 68(OCE1):E18
Baldwin C, Spiro A, Ahern R, Emery PW (2012) Oral nutritional interventions in malnourished patients with cancer: a systematic review and meta-analysis. J Natl Cancer Inst 104(5):371–385
Moher D, Liberati A, Tetzlaff J, Altman DG, Prisma Group (2010) Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Int J Surg 8(5):336–341
Silvers MA, Savva J, Huggins CE, Truby H, Haines T (2014) Potential benefits of early nutritional intervention in adults with upper gastrointestinal cancer: a pilot randomised trial. Support Care Cancer 22(11):3035–3044
Sterne JAC, Savović PMJ, Elbers RG, Blencowe NS et al (2019) RoB 2: a revised tool for assessing risk of bias in randomised trials. BMJ 366:l4898
Murad MH, Mustafa RA, Schunemann HJ, Sultan S, Santesso N (2017) Rating certainty in evidence in the absence of a single estimate of effect. Evid Based Med 22:85–87
Balshem H, Helfand M, Shunemann HJ, Ozam AD, Kunz R, Brozek J (2011) GRADE guidelines: 3. Rating the quality of evidence. J Clin Epidemiol 64(4):401–406
Burden ST, Hill J, Shaffer JL, Campbell M, Todd C (2011) An unblinded randomised controlled trial of preoperative oral supplements in colorectal cancer patients. J Hum Nutr Diet 24(5):441–448
Kabata P, Jastrzebski T, Kakol M, Krol K, Bobowicz M, Kosowska A, Jaskiewicz J (2015) Preoperative nutritional support in cancer patients with no clinical signs of malnutrition-prospective randomized controlled trial. Support Care Cancer 23(2):365–370
Beattie AH, Prach AT, Baxter JP, Pennington CR (2000) A randomised controlled trial evaluating the use of enteral nutritional supplements postoperatively in malnourished surgical patients. Gut 46(6):813–818
Rana SK, Bray J, Menzies-Gow N, Jameson J, Payne James JJ, Frost P, Silk DB (1992) Short term benefits of post-operative oral dietary supplements in surgical patients. Clin Nutr 11(6):337–344
Xie FL, Wang YQ, Peng LF, Lin FY, He YL, Jiang ZQ (2017) Beneficial effect of educational and nutritional intervention on the nutritional status and compliance of gastric cancer patients undergoing chemotherapy: a randomized trial. Nutr Cancer 69(5):762–771
MacFie J, Woodcock NP, Palmer MD, Walker A, Townsend S, Mitchell CJ (2000) Oral dietary supplements in pre- and postoperative surgical patients: a prospective and randomized clinical trial. Nutrition 16(9):723–728
Keele AM, Bray MJ, Emery PW, Duncan HD, Silk DB (1997) Two phase randomised controlled clinical trial of postoperative oral dietary supplements in surgical patients. Gut 40(3):393–399
Gavazzi C, Colatruglio S, Valoriani F, Mazzaferro V, Sabbatini A, Biffi R, Mariani L, Miceli R (2016) Impact of home enteral nutrition in malnourished patients with upper gastrointestinal cancer: a multicenter randomized clinical trial. Eur J Cancer 64:107–112
Lahoud J, Bazzi K, Yeo D, Carey S (2018) Survey of nutritional practices in total gastrectomy and oesophagectomy procedures. Nutr Diet 76(2):135–140
Carey S, He L, Ferrie S (2010) Nutritional management of patients undergoing major upper gastrointestinal surgery: a survey of current practice in Australia. Nutr Diet 67(4):219–223
Cawood AL, Elia M, Stratton RJ (2012) Systematic review and meta-analysis of the effects of high protein oral nutritional supplements. Ageing Res Rev 11(2):278–296
Naska A, Lagiou A, Lagiou P (2017) Dietary assessment methods in epidemiological research: current state of the art and future prospects. F1000Res 6:926
Ottery FD (1996) Definition of standardized nutritional assessment and interventional pathways in oncology. Nutrition 12(1 Suppl):S15–S19
Lawal AK, Rotter T, Kinsman L, Machotta A, Ronellenfitsch U, Scott SD, Goodridge D, Plishka C, Groot G (2016) What is a clinical pathway? Refinement of an operational definition to identify clinical pathway studies for a Cochrane systematic review. BMC Med 14(1):35–40
Muscaritoli M, Arends J, Aapro M (2019) From guidelines to clinical practice: a roadmap for oncologists for nutrition therapy for cancer patients. Ther Adv Med Oncol 11:1–14
Biondi A, Lirosi MC, D’Ugo D, Fico V, Riccu R et al (2015) Neo-adjuvant chemo(radio)therapy in gastric cancer: current status and future perspectives. World J Gastrointest Oncol 7(12):389–400
Author information
Authors and Affiliations
Contributions
All authors have contributed to the paper. LR designed the research, completed the literature search, extracted data, completed the study quality assessment, analysed the results and prepared the manuscript. SH was involved in the study quality assessment, analysis and interpretation of results and manuscript preparation. MA-F was involved in the design of the research, interpretation of the results and manuscript preparation. SC was involved in the research design, identification of relevant studies, data extraction, analysis and interpretation of the results, and manuscript preparation.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflicts of interest.
Ethics approval
Ethical approval was not required for this review.
Consent to participate
Consent was not required for this review.
Consent for publication
Consent was not required for this review.
Code availability
Not applicable.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
ESM 1
(DOCX 25 kb).
Rights and permissions
About this article
Cite this article
Reece, L., Hogan, S., Allman-Farinelli, M. et al. Oral nutrition interventions in patients undergoing gastrointestinal surgery for cancer: A systematic literature review. Support Care Cancer 28, 5673–5691 (2020). https://doi.org/10.1007/s00520-020-05673-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00520-020-05673-w