Abstract
Purpose
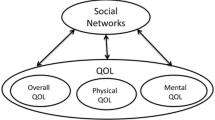
Rural women, compared to urban, experience worse survivorship outcomes, including poorer health-related quality of life (QOL). There is a need to characterize the role of multilevel social factors that contribute to QOL, including context, networks, and functioning. Our objectives were to (1) use latent class analysis to identify distinct classes of social context and social networks and (2) examine how multilevel social factors (context, networks, and functioning) are associated with health-related QOL.
Methods
We recruited self-identified rural survivors to the Illinois Rural Cancer Assessment (2017–2018), via community-based sampling methods, and participants completed the survey online, by phone, or on paper. We used latent class analysis to generate multidimensional variables for contextual and network factors. We next modeled each social factor sas a predictor in separate, bivariable linear regressions for the QOL outcomes, followed by multivariable, adjusted regressions.
Results
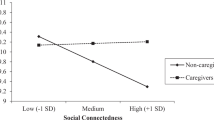
For our first objective, there were three classes each of county-level contexts (1, highly rural, socioeconomically disadvantaged, and mostly lacking in cancer-related services; 2, mostly rural, moderately disadvantaged, and underserved; 3, mostly metropolitan, less disadvantaged, and most-resourced) and social networks (1, no caregivers; 2, only spousal caregivers with whom they communicated daily; 3, multiple caregivers with varying daily communication). For our second objective, among all social factors, only functioning was associated with better mental health-related QOL. No factors were associated with physical health-related QOL.
Conclusions
Our findings suggest a rich diversity of social context and networks among rural female cancer survivors, and social functioning is particularly important for mental health-related QOL.

Similar content being viewed by others
References
Singh GK, Williams SD, Siahpush M, Mulhollen A (2011) Socioeconomic, rural-urban, and racial inequalities in US cancer mortality: part I—all cancers and lung cancer and part II—colorectal, prostate, breast, and cervical cancers. J Cancer Epidemiol 2011:1–27
Zahnd WE, James AS, Jenkins WD, et al. (2017) Rural-urban differences in cancer incidence and trends in the United States. Cancer Epidemiol Prev Biomarkers. cebp-0430
Henley SJ (2017) Invasive cancer incidence, 2004–2013, and deaths, 2006–2015, in nonmetropolitan and metropolitan counties—United States. MMWR Surveill Summ 66
Harrop JP, Dean JA, Paskett ED (2011) Cancer survivorship research: a review of the literature and summary of current NCI-designated cancer center projects. Cancer Epidemiol Biomark Prev 20(10):2042 LP–2042047. https://doi.org/10.1158/1055-9965.EPI-11-0673
Blake KD, Moss JL, Gaysynsky A, Srinivasan S, Croyle RT (2017) Making the case for investment in rural cancer control: an analysis of rural cancer incidence, mortality, and funding trends. Cancer Epidemiol Prev Biomark 26(7):992–997
National Cancer Institute. Rural Cancer Control Meeting. In: Rural Definitions—Overview and Rural Demographic Patterns. Bethesda, MD; 2018. https://cancercontrol.cancer.gov/research-emphasis/meetings/arcc-meeting.html
Soini K, Vaarala H, Pouta E (2012) Residents’ sense of place and landscape perceptions at the rural–urban interface. Landsc Urban Plan 104(1):124–134. https://doi.org/10.1016/j.landurbplan.2011.10.002
Reid-Arndt SA, Cox CR (2010) Does rurality affect quality of life following treatment for breast cancer? J Rural Health 26(4):402–405
Weaver KE, Geiger AM, Lu L, Case LD (2013) Rural-urban disparities in health status among US cancer survivors. Cancer. 119(5):1050–1057
Butow PN, Phillips F, Schweder J et al (2012) Psychosocial well-being and supportive care needs of cancer patients living in urban and rural/regional areas: a systematic review. Support Care Cancer 20(1):1–22. https://doi.org/10.1007/s00520-011-1270-1
Beck SL, Towsley GL, Caserta MS, Lindau K, Dudley WN (2009) Symptom experiences and quality of life of rural and urban older adult cancer survivors. Cancer Nurs 32(5):359–369
Luckett T, Goldstein D, Butow PN, Gebski V, Aldridge LJ, McGrane J, Ng W, King MT (2011) Psychological morbidity and quality of life of ethnic minority patients with cancer: a systematic review and meta-analysis. Lancet Oncol 12(13):1240–1248. https://doi.org/10.1016/S1470-2045(11)70212-1
Jansen L, Koch L, Brenner H, Arndt V (2010) Quality of life among long-term (⩾5years) colorectal cancer survivors – systematic review. Eur J Cancer 46(16):2879–2888. https://doi.org/10.1016/j.ejca.2010.06.010
Lyons P, Shelton MM (2012) Psychosocial impact of cancer in low-income rural/urban women: phase II. Online J Rural Nurs Health Care 4(2):6–24
Dasgupta P, Baade PD, Aitken JF, Turrell G (2012) Multilevel determinants of breast cancer survival: association with geographic remoteness and area-level socioeconomic disadvantage. Breast Cancer Res Treat 132(2):701–710
Murray CJ, Kulkarni SC, Michaud C et al (2006) Eight Americas: investigating mortality disparities across races, counties, and race-counties in the United States. PLoS Med 3(9):e260
Kroenke CH, Kwan ML, Neugut AI, Ergas IJ, Wright JD, Caan BJ, Hershman D, Kushi LH (2013) Social networks, social support mechanisms, and quality of life after breast cancer diagnosis. Breast Cancer Res Treat 139(2):515–527. https://doi.org/10.1007/s10549-013-2477-2
Cella DF, Tulsky DS, Gray G, Sarafian B, Linn E, Bonomi A, Silberman M, Yellen SB, Winicour P, Brannon J (1993) The functional assessment of cancer therapy scale: development and validation of the general measure. J Clin Oncol 11(3):570–579. https://doi.org/10.1200/JCO.1993.11.3.570
Chou AF, Stewart SL, Wild RC, Bloom JR (2010) Social support and survival in young women with breast carcinoma. Psychooncology. 21(2):125–133. https://doi.org/10.1002/pon.1863
Pedro LW, Schmiege SJ (2014) Rural living as context: a study of disparities in long-term cancer survivors. In: Oncol Nurs Forum. Vol 41
Bishaw A, Posey KG (2016) A comparison of rural and urban America: household income and poverty. United States Census Bur
Barnidge EK, Hipp PR, Estlund A, Duggan K, Barnhart KJ, Brownson RC (2013) Association between community garden participation and fruit and vegetable consumption in rural Missouri. Int J Behav Nutr Phys Act 10:128. https://doi.org/10.1186/1479-5868-10-128
Garrard ED, Fennell KM, Wilson C (2017) ‘We’re completely back to normal, but I’d say it’sa new normal’: a qualitative exploration of adaptive functioning in rural families following a parental cancer diagnosis. Support Care Cancer 25(11):3561–3568
Rogers-Clark C (2002) Living with breast cancer: the influence of rurality on women’s suffering and resilience. A postmodern feminist inquiry. Aust J Adv Nurs 20(2):34
Baernholdt M, Yan G, Hinton I, Rose K, Mattos M (2012) Quality of life in rural and urban adults 65 years and older: findings from the national health and nutrition examination survey. J Rural Health 28(4):339–347. https://doi.org/10.1111/j.1748-0361.2011.00403.x
Lichter DT, Brown DL (2011) Rural America in an Urban Society: changing spatial and social boundaries. Annu Rev Sociol 37(1):565–592. https://doi.org/10.1146/annurev-soc-081309-150208
Strayhorn S, Carnahan LR, Zimmermann K et al (2019) Co-morbidities, treatment-related consequences and health-related quality of life among rural cancer survivors. Support Care Cancer:1–10
Ware JE Jr, Kosinski M, Keller SD (1996) A 12-item short-form health survey: construction of scales and preliminary tests of reliability and validity. Med Care 34(3):220–233
United States Department of Agriculture. Rural Urban Continuum Codes. https://www.ers.usda.gov/data-products/rural-urban-continuum-codes/. Published 2013
Yaghjyan L, Cogle CR, Deng G, Yang J, Jackson P, Hardt N, Hall J, Mao L (2019) Continuous rural-urban coding for cancer disparity studies: is it appropriate for statistical analysis? Int J Environ Res Public Health 16(6):1076
U.S. Census Bureau. American Community Survey. 2013–2017 American Community Survey 5-Year Estimates, Table ACS_17_5YR_DP03; generated by Leslie Carnahan; using American FactFinder. http://factfinder.census.gov. Published 2017
Butler DC, Petterson S, Phillips RL, Bazemore AW (2013) Measures of social deprivation that predict health care access and need within a rational area of primary care service delivery. Health Serv Res 48(2pt1):539–559
Smith T, Davern M, Reese J, Hout M (2018) General social surveys, 1972–2016. Chicago: NORC at the University of Chicago
Victorson D, Barocas J, Song J, Cella D (2008) Reliability across studies from the functional assessment of cancer therapy-general (FACT-G) and its subscales: a reliability generalization. Qual Life Res 17(9):1137–1146. https://doi.org/10.1007/s11136-008-9398-2
Westmaas JL, Fallon E, McDonald BR et al (2019) Investigating relationships among cancer survivors’ engagement in an online support community, social support perceptions, well-being, and moderating effects of existing (offline) social support. Support Care Cancer:1–9
Neumann M, Wirtz M, Ernstmann N, Ommen O, Längler A, Edelhäuser F, Scheffer C, Tauschel D, Pfaff H (2011) Identifying and predicting subgroups of information needs among cancer patients: an initial study using latent class analysis. Support Care Cancer 19(8):1197–1209
Leung J, Smith A, Atherton I, McLaughlin D (2016) “Everybody knows everybody else’s business”—privacy in rural communities. J Cancer Educ 31(4):811–812
Fortin M, Bravo G, Hudon C, Lapointe L, Almirall J, Dubois MF, Vanasse A (2006) Relationship between multimorbidity and health-related quality of life of patients in primary care. Qual Life Res 15(1):83–91
Olatunji BO, Cisler JM, Tolin DF (2007) Quality of life in the anxiety disorders: a meta-analytic review. Clin Psychol Rev 27(5):572–581
Bigbee JL, Lind B (2007) Methodological challenges in rural and frontier nursing research. Appl Nurs Res 20(2):104–106. https://doi.org/10.1016/j.apnr.2007.01.001
Zahnd WE, Mueller GS, Fogleman AJ, Jenkins WD (2016) Intrastate variations in rural cancer risk and incidence: an Illinois case study. J Public Health Manag Pract 22(5):472–478. https://doi.org/10.1097/PHH.0000000000000310
Zahnd WE, Jenkins WD, Mueller-Luckey GS (2017) Cancer mortality in the Mississippi Delta region: descriptive epidemiology and needed future research and interventions. J Health Care Poor Underserved 28(1):315–328
Symens Smith A, Trevelyan E. Older populations in rural America. In some states, more than half of older residents live in rural areas. https://www.census.gov/library/stories/2019/10/older-population-in-rural-america.html. Published 2019. Accessed 19 Feb 2020
Kirby JB, Muhuri P (2018) Insurance and access to care in urban and rural areas, 2014–2015. In: Statistical Brief (Medical Expenditure Panel Survey (US))[Internet]. Agency for Healthcare Research and Quality (US)
Semega JL, Fontenot KR, Kollar MA (2016) US Census Bureau, Current Population Reports, P60–259, Income and Poverty in the United States. US Gov print off Washington, DC. 2017:10–11
Acknowledgments
We thank the cancer survivors who graciously provided their time and information, thereby making this research possible. We would also like to thank the following individuals who contributed their efforts to the study: Martasia Carter, Emily Hallgren, Jocelyne Lemus, Patricia Newton, Lillian Oluchi Nwigwe, Kryztal Peña, Lillian San Miguel, Mona Strahan, and Nidhi Suthar. Lastly, this manuscript is a component of Leslie Carnahan’s working dissertation and will be included in as a chapter in the thesis.
Funding
The Illinois Rural Cancer Assessments study was an intramurally funded project supported by the University of Illinois at Chicago’s Center for Research on Women and Gender and University of Illinois Cancer Center.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Ms. Carnahan, Dr. Rauscher, Dr. Watson, Dr. Altfeld, Dr. Zimmermann, Dr. Ferrans, and Dr. Molina have no financial relationships to disclose. Ms. Carnahan reports this manuscript is a component of their working dissertation and will be included in as a chapter in the thesis. The authors have full control of all primary data and will all the journal to review the data if requested.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
ESM 1
(DOCX 19 kb)
Rights and permissions
About this article
Cite this article
Carnahan, L.R., Rauscher, G.H., Watson, K.S. et al. Comparing the roles of social context, networks, and perceived social functioning with health-related quality of life among self-reported rural female cancer survivors. Support Care Cancer 29, 331–340 (2021). https://doi.org/10.1007/s00520-020-05497-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00520-020-05497-8