Abstract
Purpose
Understanding how the information needs of cancer patients (CaPts) vary is important because met information needs affect health outcomes and CaPts’ satisfaction. The goals of the study were to identify subgroups of CaPts based on self-reported cancer- and treatment-related information needs and to determine whether subgroups could be predicted on the basis of selected sociodemographic, clinical and clinician–patient relationship variables.
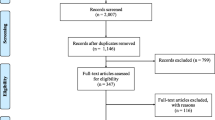
Methods
Three hundred twenty-three CaPts participated in a survey using the “Cancer Patients Information Needs” scale, which is a new tool for measuring cancer-related information needs. The number of information need subgroups and need profiles within each subgroup was identified using latent class analysis (LCA). Multinomial logistic regression was applied to predict class membership.
Results
LCA identified a model of five subgroups exhibiting differences in type and extent of CaPts’ unmet information needs: a subgroup with “no unmet needs” (31.4% of the sample), two subgroups with “high level of psychosocial unmet information needs” (27.0% and 12.0%), a subgroup with “high level of purely medical unmet information needs” (16.0%) and a subgroup with “high level of medical and psychosocial unmet information needs” (13.6%). An assessment of sociodemographic and clinical characteristics revealed that younger CaPts and CaPts’ requiring psychological support seem to belong to subgroups with a higher level of unmet information needs. However, the most significant predictor for the subgroups with unmet information needs is a good clinician–patient relationship, i.e. subjective perception of high level of trust in and caring attention from nurses together with high degree of physician empathy seems to be predictive for inclusion in the subgroup with no unmet information needs.
Conclusions
The results of our study can be used by oncology nurses and physicians to increase their awareness of the complexity and heterogeneity of information needs among CaPts and of clinically significant subgroups of CaPts. Moreover, regression analyses indicate the following association: Nurses and physicians seem to be able to reduce CaPts’ unmet information needs by establishing a relationship with the patient, which is trusting, caring and empathic.


Similar content being viewed by others
References
ASCO (2006) ASCO-ESMO consensus statement on quality cancer care. Am J Clin Oncol 24:3498–3499
Epstein RM, Street RL (2007) Patient-centred communication in cancer care. Promoting healing and reducing suffering. National Cancer Institute. NIH Publication No. 07-6225. Bethesda, MD
Sheer V, Cline R (1995) Testing a model of perceived information adequacy and uncertainty reduction in physician–patient interactions. J Appl Commun Res 23:44–59
Street R (1991) Information-giving in medical consultations: the influence of patients’ communicative styles and personal characteristics. Soc Sci Med 32:541–548
Fallowfield L, Jenkins V (1999) Effective communication skills are the key to good cancer care. Eur J Cancer Care 35:1592–1597
Kim SS, Kaplowitz S, Johnston MV (2004) The effects of physician empathy on patient satisfaction and compliance. Eval Health Prof 27:237–251
Neumann M, Wirtz M, Bollschweiler E et al (2007) Determinants and patient-reported long-term outcomes of physician empathy in oncology: a structural equation modelling approach. Patient Educ Couns 69:63–75
Arora N, Johnson P, Gustafson D, McTavish F, Hawkins R, Pingree S (2002) Barriers to information access, perceived health competence, and psychosocial health outcomes: test of a mediation model in a breast cancer sample. Patient Educ Couns 47:37–46
Thorne SE, Bultz BD, Baile W (2005) Is there a cost to poor communication in cancer care? A critical review of the literature. Psychooncology 14:875–884
Chaitchik S, Kreitler S, Shaked S, Schwart I, Rosin R (1992) Doctor–patient communication in a cancer ward. J Cancer Educ 7:41–54
Gattellari M, Butow PN, Tattersall MH (2001) Sharing decisions in cancer care. Soc Sci Med 52:1865–1878
Chan A, Woddruff R (1997) Communication with patients with advanced cancer. J Palliat Care 13:29–33
Quirt C, Macillop W, Ginsburg A et al (1997) Do doctors know when their patients don’t? A survey of doctor–patient communication in lung cancer. Lung Cancer 18:1–10
Arora NK (2003) Interacting with cancer patients: the significance of physicians’ communication behavior. Soc Sci Med 57:791–806
Hain T (2000) The role of health professionals in informing cancer patients: findings from The Teamwork Project (phase one). Health Expect 3:217–219
Mesters I, van den Borne B, De Boer M, Pruyn J (2001) Measuring information among cancer patients. Patient Educ Couns 43:253–262
Dillman DA (1978) Mail and telephone surveys. The total design method. Wiley, New York
Dillman DA (2000) Mail and internet surveys. Wiley, New York
Ommen O, Janssen C, Neugebauer E, Bouillon B, Rehm K, Rangger C, Erli H, Pfaff H (2008) Trust, social support and patient type—associations between patients perceived trust, supportive communication and patients preferences in regard to paternalism, clarification and participation of severely injured patients. Patient Educ Couns 73:196–204
Pfaff H (2003) Der Kölner Patientenfragebogen: Theoretischer Rahmen, Konstrukte und Messinstrumente./The Cologne Patient Questionnaire: theory, constructs and measures. In: Pfaff H, Freise D, Mager G, Schrappe M (eds) Der Kölner Patientenfragebogen (KPF): Entwicklung und Validierung eines Fragebogens zur Erfassung der Einbindung des Patienten als Kotherapeuten./The Cologne Patient Questionnaire (CPQ): development and validation of a questionnaire to assess the patient as a co-therapist. Asgard, Sankt Augustin, pp 7–27
Pfaff H, Steffen P, Brinkmann A, Lütticke J, Nitzsche A (2004) Der Kölner Patientenfragebogen (KPF). Kennzahlenhandbuch./The Cologne Patient Questionnaire (CPQ). Handbook of indices. Veröffentlichungsreihe der Abteilung Medizinische Soziologie des Instituts für Arbeitsmedizin, Sozialmedizin und Sozialhygiene der Universität zu Köln: ISSN 1618-7067
Neumann M, Wirtz M, Bollschweiler E, Warm M, Wolf J, Pfaff H (2008) Psychometrische Evaluation der deutschen Version des Messinstruments “Consultation and Relational Empathy” (CARE) am Beispiel von Krebspatienten./Psychometric evaluation of the German version of the “Consultation and Relational Empathy” (CARE) at the example of cancer patients. Psychother Psychosom Med Psychol 58:5–15
Mercer SW, Maxwell M, Heaney D, Watt GC (2004) The Consultation and Relational Empathy (CARE) measure: development and preliminary validation and reliability of an empathy-based consultation process measure. Fam Prac 21:1–6
Mercer SW, McConnachie A, Maxwell M, Heaney D, Watt GC (2005) Relevance and practical use of the Consultation and Relational Empathy (CARE) measure in general practice. Fam Prac 22:328–334
Mercer SW, Neumann M, Wirtz M, Fitzpatrick B, Vojt G (2008) General practitioner empathy, patient enablement, and patient-reported outcomes in primary care in an area of high socio-economic deprivation in Scotland: a pilot prospective study using structural equation modelling. Patient Educ Couns 73:240–245
Allison PD (2001) Missing data. Sage, Thousand Oaks
Schafer JL, Graham JW (2002) Missing data: our view of the state of the art. Psychol Meth 7:147–177
Graham JW, Cumsille PE, Elek-Fisk E (2003) Methods for handling missing data. In: Schinka JA, Velicer WF (eds) Research methods in psychology. Wiley, New York, pp 87–114
Clogg CC (1995) Latent class models. In: Arminger G, Clogg CC, Sobel ME (eds) Handbook of statistical modeling for the social and behavioural sciences. Plenum, New York, pp 311–359
Hagenaars JA, McCutcheon AL (2002) Applied latent class analysis. Cambridge University Press, Cambridge
Lazarsfeld PF (1950) The logical and mathematical foundation of latent structure analysis. In: Stouffer S (ed) Measurement and prediction. Princeton University Press, Princeton, pp 362–412
McCutcheon AL (1987) Latent class analysis. Sage, Newbury Park
Muthen B, Muthen LK (2000) Integrating person-centered and variable-centered analyses: growth mixture modeling with latent trajectory classes. Alcohol Clin Exp Res 24:882–891
Hambleton R, Swaminathan H, Rogers HJ (1991) Fundamentals of item response theory. Sage, Newbury Park
Vermunt JK, Magidson J (2005) Latent Gold 4.0 user’s guide. Statistical Innovations, Belmont
Vermunt JK, Magidson J (2002) Latent class cluster analysis. In: Hagenaars JA, McCutcheon AL (eds) Applied latent class analysis. Cambridge University Press, Cambridge, pp 89–107
Neumann M, Galushko M, Goldblatt H, Visser A, Wirtz M, Karbach U, Ernstmann N, Ommen O, Pfaff H (2009) Barriers to use psycho-oncological services an exploration of perspectives by users, their relatives, non-users, physicians, and nurses. Support Care Cancer. doi:10.1007/s00520-009-0731-2
Hair JF, Anderson RE, Tatham RL, Black WC (2006) Multivariate data analysis. Upper Prentice Hall, Saddle River
Mittag O, Böhmer S, Deck R et al (2003) Fragen über Fragen: cognitive survey in der Fragebogenentwicklung./One question after the other: cognitive survey in the development of questionnaires. Soz Praventivmed 48:55–64
Longo DR (2005) Understanding health information, communication, and information seeking of patients and consumers: a comprehensive and integrated model. Health Expect 8:189–194
Schofield NG, Green C, Creed F (2008) Communication skills of health-care professionals working in oncology—can they be improved? Eur J Oncol Nurs 12:4–13
Brown R, Butow PN, Boyer MJ, Tattersall MHN (1999) Promoting patient participation in the cancer consultation: evaluation of a prompt sheet and coaching in question asking. Br J Cancer 80:242–248
Clayton J, Butow PN, Tattersall MHN, Devine RJ, Simpson JM, Aggarwal G, Clark KJ, Currow DC, Elliott LM, Lacey J, Lee PG, Noel MA (2007) Randomized controlled trial of a prompt list to help advanced cancer patients and their caregivers to ask questions about prognosis and end-of-life care. J Clin Oncol 25:715–723
Kruijver IPM, Garssen B, Visser AP, Kuiper AJ (2006) Signalising psychosocial problems in cancer care. The structural use of a short psychosocial checklist during medical or nursing visits. Patient Educ Couns 62:163–177
Parker PA, Davison BJ, Tishelman C, Brundage MD (2005) What do we know about facilitating patient communication in the cancer care setting? Psycho-Oncol 14:848–858
Sepucha KR, Belkora JK, Mutchnik S, Esserman LJ (2002) Consultation planning to help breast cancer patients prepare for medical consultations: effect on communication and satisfaction for patients and physicians. J Clin Oncol 20:2695–2700
van Wersch A, de Boer MF, van der Does E, de Jong P, Knegt P, Meeuwis CA, Stringer P, Pruyn JFA (1997) Continuity of information in cancer care: evaluation of a logbook. Patient Educ Couns 31:223–236
Acknowledgements
We are grateful to the Else Kröner-Fresenius Foundation for providing financial support during the course of this study (grant number P43/05//A33/05/F0). Melanie Neumann is supported by a grant from the Software AG Foundation, Germany. We would also like to thank Sarah Frances for her qualified support concerning our application of the English language.
We confirm all patient/personal identifiers have been removed or disguised so the patients/persons described are not identifiable and cannot be identified through the details of the article.
Conflict of interest
The authors indicated no potential conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Appendix
Appendix
Translation of the German measures
Measure | English translation |
Trust in nurses | The nurses were open and honest with me. |
I completely trusted my nurses. | |
The nurses did not interrupt me while I was talking. | |
I had the impression that the nurses are very competent. | |
With the nurses in this hospital, one is in good hands. | |
Caring attention from nurses | The nurses showed feeling in their discussion with me. |
The nurses conducted regular discussions with me. | |
I had a dedicated contact person assigned to me from the nursing staff. | |
One could personally confide in the nurses. | |
The nurses gave me time to think when important decisions had to me made. |
Rights and permissions
About this article
Cite this article
Neumann, M., Wirtz, M., Ernstmann, N. et al. Identifying and predicting subgroups of information needs among cancer patients: an initial study using latent class analysis. Support Care Cancer 19, 1197–1209 (2011). https://doi.org/10.1007/s00520-010-0939-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00520-010-0939-1