Summary
Objectives
To investigate the correlations between physical activity (PA) and metabolic associated fatty liver disease (MAFLD) or metabolic dysfunction-associated steatotic liver disease (MASLD) within a substantial population-based survey, and to examine the association between PA and liver fibrosis (LF).
Methods
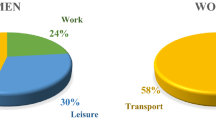
Data from the 2017–2020 NHANES cycle were utilized in this study. PA was divided into four types: leisure-time PA (LTPA), transportation-related PA (TPA), occupational PA (OPA) and total time PA (total PA, which is composed of OPA, TPA and LTPA). Weighted logistic regression models were performed to analyze the associations between PA and MAFLD/MASLD and LF. Mediation analysis was used to explore whether LTPA completely mediated the statistically significant relationship between total PA and MAFLD/MASLD or LF.
Results
The study encompassed a sample size of 5897 participants aged 20 years and above, among the total participants, 2568 individuals with MAFLD and 2588 individuals with MASLD. There was no statistically significant correlation observed between OPA/TPA and MAFLD/MASLD and LF; however, active LTPA demonstrated an inverse association with MAFLD/MASLD (OR: 0.548; 95% CI: 0.458, 0.656/OR: 0.543; 95% CI: 0.453, 0.650), as well as a negative correlation with significant/advanced LF (OR: 0.457; 95% CI: 0.334,0.625/OR: 0.427; 95% CI: 0.295,0.619). There was also a significant inverse association between total PA and MAFLD/MASLD or LF, but this association was carried by the difference in LTPA.
Conclusion
Participation in active LTPA is associated with a reduced likelihood of MAFLD/MASLD and LF, while neither OPA nor TPA can replace these effects of LTPA.

Similar content being viewed by others
Availability of data and material
Publicly available datasets were analyzed in this study. The data can be found at: https://www.cdc.gov/nchs/nhanes/index.htm.
Abbreviations
- BMI:
-
Body mass index
- CAP:
-
Controlled attenuation parameters
- CDC:
-
Disease control and prevention
- CI:
-
Confidence interval
- HBV:
-
Hepatitis B virus
- HCV:
-
Hepatitis C virus
- LF:
-
Liver fibrosis
- LSM:
-
Liver stiffness measurement
- LTPA:
-
Leisure-time physical activity
- MAFLD:
-
Metabolic associated fatty liver disease
- MASLD:
-
Metabolic dysfunction-associated steatotic liver disease
- NAFLD:
-
Non-alcoholic fatty liver disease
- NCHS:
-
National Center for Health Statistics
- NHANES:
-
National Health and Nutrition Examination Survey
- OPA:
-
Occupational physical activity
- OR:
-
Odds ratios
- SD:
-
Standard deviation
- Total PA:
-
Total-time physical activity
- TPA:
-
Transportation-related physical activity
- VCTE:
-
Vibration-controlled transient elastography
References
Li J, Zou B, Yeo YH, Feng Y, Xie X, Lee DH, et al. Prevalence, incidence, and outcome of non-alcoholic fatty liver disease in Asia, 1999–2019: a systematic review and meta-analysis. Lancet Gastroenterol Hepatol. 2019;4(5):389–98. May.
Nan Y, An J, Bao J, Chen H, Chen Y, Ding H, et al. The Chinese Society of Hepatology position statement on the redefinition of fatty liver disease. J Hepatol. 2021;75:454–61.
Tapper EB, Parikh ND. Mortality due to cirrhosis and liver cancer in the United States, 1999–2016: observational study. BMJ. 2018;18;362:k2817. Jul.
Asrani SK, Devarbhavi H, Eaton J, Kamath PS. Burden of liver diseases in the world. J Hepatol. 2019;70(1):151–71. https://doi.org/10.1016/j.jhep.2018.09.014.
Marchesini G, Brizi M, Bianchi G, Tomassetti S, Bugianesi E, Lenzi M, et al. Nonalcoholic fatty liver disease: a feature of the metabolic syndrome. Diabetes. 2001;50(8:1844–50.
Marchesini G, Brizi M, Morselli-Labate AM, Bianchi G, Bugianesi E, McCullough AJ, et al. Association of nonalcoholic fatty liver disease with insulin resistance. Am J Med. 1999;107(5):450–5.
Radaelli MG, Martucci F, Perra S, Accornero S, Castoldi G, Lattuada G, Manzoni G, et al. NAFLD/NASH in patients with type 2 diabetes and related treatment options. J Endocrinol Invest. 2018;41(5):509–21.
Eslam M , Newsome PN , Sarin SK , Anstee QM, Targher G, Romero-Gomez M, et al. A new definition for metabolic dysfunction-associated fatty liver disease: an international expert consensus statement[J]. J Hepatol, 2020, 73(1): 202–209. https://doi.org/10.1016/j.jhep.2020.03.039 .
Eslam M, Sarin SK, Wong VWS, Fan JG, Kawaguchi T, Ahn SH, et al. The Asian Pacific Association for the Study of the Liver clinical practice guidelines for the diagnosis and management of metabolic associated fatty liver disease. Hepatol Int. 2020;14:889–919.
Younossi ZM, Rinella ME, Sanyal AJ, Harrison SA, Brunt EM, Goodman Z, et al. From NAFLD to MAFLD: Implications of a Premature Change in Terminology. Hepatology. 2021;73:1194–8.
Ratziu V, Rinella M, Beuers U, Loomba R, Anstee QM, Harrison S, et al. The times they are a‑changin’ (for NAFLD as well). J Hepatol. 2020;73:1307–9.
Rinella ME, Lazarus JV, Ratziu V, Francque SM, Sanyal AJ, Kanwal F, et al. A multi-society Delphi consensus statement on new fatty liver disease nomenclature. J Hepatol. 2023 Jun 20:S0168–8278(23)00418‑X. .
Ciardullo S, Carbone M, Invernizzi P, Perseghin G. Exploring the landscape of steatotic liver disease in the general US population. Liver Int. 2023;17.
Riazi K, Azhari H, Charette JH, Underwood FE, King JA, Afshar EE, et al. The prevalence and incidence of NAFLD worldwide: a systematic review and meta-analysis. Lancet Gastroenterol Hepatol. 2022;7(9):851–61. Sep.
Friedman SL, Neuschwander-Tetri BA, Rinella M, Sanyal AJ. Mechanisms of NAFLD development and therapeutic strategies. Nat Med. 2018;24(7):908–22. Jul.
Jakicic JM, Rogers RJ, Davis KK, Collins KA. Role of Physical Activity and Exercise in Treating Patients with Overweight and Obesity. Clin Chem. 2018;64(1):99–107. Jan.
Kanaley JA, Colberg SR, Corcoran MH, Malin SK, Rodriguez NR, Crespo CJ, et al. Exercise/Physical Activity in Individuals with Type 2 Diabetes: A Consensus Statement from the American College of Sports Medicine. Med Sci Sports Exerc. 2022;1;54(2):353–68. Feb.
Tucker WJ, Fegers-Wustrow I, Halle M, Haykowsky MJ, Chung EH, Kovacic JC. Exercise for Primary and Secondary Prevention of Cardiovascular Disease: JACC Focus Seminar 1/4. J Am Coll Cardiol. 2022 Sep 13;80(11):1091–1106.
Smith PJ, Merwin RM. The Role of Exercise in Management of Mental Health Disorders: An Integrative Review. Annu Rev Med. 2021;27;72:45–62. Jan.
Rinella ME. Nonalcoholic fatty liver disease: a systematic review. JAMA. 2015;9;313(22):2263–73. Jun.
Wang X, Wang A, Zhang R, Cheng S, Pang Y. Associations between Healthy Lifestyle and All-Cause Mortality in Individuals with Metabolic Associated Fatty Liver Disease. Nutrients. 2022;11;14(20):4222. Oct.
Chun HS, Lee M, Lee HA, Oh SY, Baek HJ, Moon JW, et al. Association of Physical Activity With Risk of LF, Sarcopenia, and Cardiovascular Disease in Nonalcoholic Fatty Liver Disease. Clin Gastroenterol Hepatol. 2023;21(2):358–369.e1. 2.
Castera L, Friedrich-Rust M, Loomba R. Noninvasive Assessment of Liver Disease in Patients With Nonalcoholic Fatty Liver Disease. Gastroenterology. 2019;156(5):1264–1281.e4.
Bull FC, Maslin TS, Armstrong T. Global physical activity questionnaire (GPAQ): nine country reliability and validity study. J Phys Act Health. 2009;6(6):790–804. Nov.
Divney AA, Murillo R, Rodriguez F, Mirzayi CA, Tsui EK, Echeverria SE. Diabetes Prevalence by Leisure‑, Transportation-, and Occupation-Based Physical Activity Among Racially/Ethnically Diverse U.S. Adults. Diabetes Care. 2019;42(7):1241–7. Jul.
Chu NM, Hong J, Harasemiw O, Chen X, Fowler KJ, al Dasgupta I. Global Renal Exercise Network. Chronic kidney disease, physical activity and cognitive function in older adults-results from the National Health and Nutrition Examination Survey (2011–2014). Nephrol Dial Transplant. 2022;19;37(11):2180–9. Oct.
US Department of Health and Human Services . Physical Activity Guidelines for Americans. https://health.gov/sites/default/files/2019-09/paguide.pdf (August 2020, date last accessed).
American Diabetes Association. 2. Classification and Diagnosis of Diabetes: Standards of Medical Care in Diabetes-2020. Diabetes Care. 2020;43(Suppl 1):14–S31.
Eddowes PJ, Sasso M, Allison M, Tsochatzis E, Anstee QM, Sheridan D, et al. Accuracy of FibroScan controlled attenuation parameter and liver stiffness measurement in assessing steatosis and fibrosis in patients with nonalcoholic fatty liver disease. Gastroenterology. 2019;156(6):1717–30.
Chalasani N, Younossi Z, Lavine JE, Charlton M, Cusi K, Rinella M, et al. The diagnosis and management of nonalcoholic fatty liver disease: practice guidance from the American Association for the Study of Liver Diseases. Hepatology. 2018;67(1):328–57.
Centers for Disease Control. Prevention . Testing for HCV infection: an update of guidance for clinicians and laboratorians. Mmwr Morb Mortal Wkly Rep. 2013;62:362–5.
Coffin CS, Zhou K, Terrault NA. New and old biomarkers for diagnosis and management of chronic hepatitis B virus infection. Gastroenterology. 2019;156(e3):355–68.
Roulot D, Czernichow S, Le Clésiau H, Costes JL, Vergnaud AC, Beaugrand M. Liver stiffness values in apparently healthy subjects: influence of gender and metabolic syndrome. J Hepatol. 2008;48(4):606–13. Apr.
Yang C, Jia X, Wang Y, Fan J, Zhao C, Yang Y, et al. Trends and influence factors in the prevalence, intervention, and control of metabolic syndrome among US adults, 1999–2018. BMC Geriatr. 2022;19;22(1):979. Dec.
Guerra JVS, Dias MMG, Brilhante AJVC, Terra MF, García-Arévalo M, Figueira ACM. Multifactorial Basis and Therapeutic Strategies in Metabolism-Related Diseases. Nutrients. 2021;18;13(8):2830. Aug.
El-Agroudy NN, Kurzbach A, Rodionov RN, O’Sullivan J, Roden M, Birkenfeld AL. Are Lifestyle Therapies Effective for NAFLD Treatment? Trends Endocrinol Metab. 2019;30(10):701–9. Oct.
Shojaee-Moradie F, Cuthbertson DJ, Barrett M, Jackson NC, Herring R, Thomas EL, et al. Exercise training reduces liver fat and increases rates of VLDL clearance but not VLDL production in NAFLD. J Clin Endocrinol Metab. 2016;101(11):4219–28.
Martins C, Morgan L, Truby H. A review of the effects of exercise on appetite regulation: an obesity perspective. Int J Obes (2005). 2008;32(9):1337–1347.
Lee YH, Jung KS, Kim SU, Yoon HJ, Yun YJ, Lee BW, et al. Sarcopaenia is associated with NAFLD independently of obesity and insulin resistance: nationwide surveys (KNHANES 2008–2011). J Hepatol. 2015;63(2):486–93.
Koo BK, Kim D, Joo SK, Kim JH, Chang MS, Kim BG, et al. Sarcopenia is an independent risk factor for non-alcoholic steatohepatitis and significant fibrosis. J Hepatol. 2017;66(1):123–31.
Longo M, Meroni M, Paolini E, Macchi C, Dongiovanni P. Mitochondrial dynamics and nonalcoholic fatty liver disease (NAFLD): new perspectives for a fairy-tale ending? Metabolism. 2021;117:154708.
Guarino M, Kumar P, Felser A, Terracciano LM, Guixé-Muntet S, Humar B, et al. Exercise Attenuates the Transition from Fatty Liver to Steatohepatitis and Reduces Tumor Formation in Mice. Cancers (basel). 2020;29;12(6):1407. May.
Saran U, Guarino M, Rodríguez S, Simillion C, Montani M, Foti M, et al. Anti-tumoral effects of exercise on hepatocellular carcinoma growth. Hepatol Commun. 2018;22;2(5):607–20. Mar.
Hamer M, Sabia S, Batty GD, Shipley MJ, Tabák AG, Singh-Manoux A, et al. Physical activity and inflammatory markers over 10 years: follow-up in men and women from the Whitehall II cohort study. Circulation. 2012;21;126(8):928–33. Aug.
Li H, Wu X, Bai Y, Wei W, Li G, Fu M, et al. Physical activity attenuates the associations of systemic immune-inflammation index with total and cause-specific mortality among middle-aged and older populations. Sci Rep. 2021;15;11(1):12532. Jun.
Lee IM, Shiroma EJ, Lobelo F, Puska P, Blair SN, Katzmarzyk PT, Lancet Physical Activity Series Working Group. Effect of physical inactivity on major non-communicable diseases worldwide: an analysis of burden of disease and life expectancy. Lancet. 2012;21;380(9838):219–29. Jul.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
M. Li declares that he/she has no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Li, M. Association of physical activity with MAFLD/MASLD and LF among adults in NHANES, 2017–2020. Wien Klin Wochenschr 136, 258–266 (2024). https://doi.org/10.1007/s00508-023-02314-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00508-023-02314-0