Abstract
Background
Studies in critically ill adults demonstrate associations between serum renin concentrations (a proposed surrogate for renin–angiotensin–aldosterone system dysregulation) and poor outcomes, but data in critically ill children are lacking. We assessed serum renin + prorenin concentrations in children with septic shock to determine their predictive ability for acute kidney injury (AKI) and mortality.
Methods
We conducted a secondary analysis of a multicenter observational study of children aged 1 week to 18 years admitted to 14 pediatric intensive care units (PICUs) with septic shock and residual serum available for renin + prorenin measurement. Primary outcomes were development of severe persistent AKI (≥ KDIGO stage 2 for ≥ 48 h) in the first week and 28-day mortality.
Results
Among 233 patients, day 1 median renin + prorenin concentration was 3436 pg/ml (IQR 1452–6567). Forty-two (18%) developed severe persistent AKI and 32 (14%) died. Day 1 serum renin + prorenin predicted severe persistent AKI with an AUROC of 0.75 (95% CI 0.66–0.84, p < 0.0001; optimal cutoff 6769 pg/ml) and mortality with an AUROC of 0.79 (95% CI 0.69–0.89, p < 0.0001; optimal cutoff 6521 pg/ml). Day 3/day 1 (D3:D1) renin + prorenin ratio had an AUROC of 0.73 (95% CI 0.63–0.84, p < 0.001) for mortality. On multivariable regression, day 1 renin + prorenin > optimal cutoff retained associations with severe persistent AKI (aOR 6.8, 95% CI 3.0–15.8, p < 0.001) and mortality (aOR 6.9, 95% CI 2.2–20.9, p < 0.001). Similarly, D3:D1 renin + prorenin > optimal cutoff was associated with mortality (aOR 7.6, 95% CI 2.5–23.4, p < 0.001).
Conclusions
Children with septic shock have very elevated serum renin + prorenin concentrations on PICU admission, and these concentrations, as well as their trend over the first 72 h, predict severe persistent AKI and mortality.
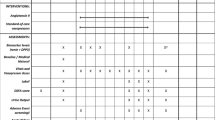
Graphical abstract

A higher resolution version of the Graphical abstract is available as Supplementary information

Similar content being viewed by others
Data availability
The datasets generated during and/or analysed during the current study are available from the corresponding author on reasonable request.
Change history
23 April 2023
The name Naomi Pode Shakked has been tagged correctly.
References
Weiss SL, Fitzgerald JC, Pappachan J, Wheeler D, Jaramillo-Bustamante JC, Salloo A, Singhi SC, Erickson S, Roy JA, Bush JL, Nadkarni VM, Thomas NJ, Sepsis Prevalence, Outcomes, and Therapies (SPROUT) Study Investigators and Pediatric Acute Lung Injury and Sepsis Investigators (PALISI) Network (2015) Global epidemiology of pediatric severe sepsis: the sepsis prevalence, outcomes, and therapies study. Am J Respir Crit Care Med 191:1147–1157. https://doi.org/10.1164/rccm.201412-2323OC
Balamuth F, Weiss SL, Neuman MI, Scott H, Brady PW, Paul R, Farris RWD, McClead R, Hayes K, Gaieski D, Hall M, Shah SS, Alpern ER (2014) Pediatric severe sepsis in US Children’s Hospitals. Pediatr Crit Care Med 15:798–805. https://doi.org/10.1097/PCC.0000000000000225
Watson RS, Carcillo JA, Linde-Zwirble WT, Clermont G, Lidicker J, Angus DC (2003) The epidemiology of severe sepsis in children in the United States. Am J Respir Crit Care Med 167:695–701. https://doi.org/10.1164/rccm.200207-682OC
Zimmerman JJ, Banks R, Berg RA, Zuppa A, Newth CJ, Wessel D, Pollack MM, Meert KL, Hall MW, Quasney M, Sapru A, Carcillo JA, McQuillen PS, Mourani PM, Wong H, Chima RS, Holubkov R, Coleman W, Sorenson S, Varni JW, McGalliard J, Haaland W, Whitlock K, Dean JM, Reeder RW, Life After Pediatric Sepsis Evaluation (LAPSE) Investigators (2020) Trajectory of mortality and health-related quality of life morbidity following community-acquired pediatric septic shock. Crit Care Med 48:329–337. https://doi.org/10.1097/CCM.0000000000004123
Stanski NL, Cvijanovich NZ, Fitzgerald JC, Bigham MT, Wong HR, Genomics of Pediatric Septic Shock Investigators (2020) Severe acute kidney injury is independently associated with mortality in children with septic shock. Intensive Care Med 46:1050–1051. https://doi.org/10.1007/s00134-020-05940-8
Fitzgerald JC, Basu RK, Akcan-Arikan A, Izquierdo LM, PiñeresOlave BE, Hassinger AB, Szczepanska M, Deep A, Williams D, Sapru A, Roy JA, Nadkarni VM, Thomas NJ, Weiss SL, Furth S, Sepsis PRevalence, OUtcomes, and Therapies Study Investigators and Pediatric Acute Lung Injury and Sepsis Investigators Network (2016) Acute kidney injury in pediatric severe sepsis: an independent risk factor for death and new disability. Crit Care Med 44:2241–2250. https://doi.org/10.1097/CCM.0000000000002007
Starr MC, Banks R, Reeder RW, Fitzgerald JC, Pollack MM, Meert KL, McQuillen PS, Mourani PM, Chima RS, Sorenson S, Varni JW, Hingorani S, Zimmerman JJ (2020) Severe acute kidney injury is associated with increased risk of death and new morbidity after pediatric septic shock. Pediatr Crit Care Med 21:e686–e695. https://doi.org/10.1097/PCC.0000000000002418
Weiss SL, Peters MJ, Alhazzani W, Agus MSD, Flori HR, Inwald DP, Nadel S, Schlapbach LJ, Tasker RC, Argent AC, Brierley J, Carcillo J, Carrol ED, Carroll CL, Cheifetz IM, Choong K, Cies JJ, Cruz AT, De Luca D, Deep A, Faust SN, De Oliveira CF, Hall MW, Ishimine P, Javouhey E, Joosten KFM, Joshi P, Karam O, Kneyber MCJ, Lemson J, MacLaren G, Mehta NM, Møller MH, Newth CJL, Nguyen TC, Nishisaki A, Nunnally ME, Parker MM, Paul RM, Randolph AG, Ranjit S, Romer LH, Scott HF, Tume LN, Verger JT, Williams EA, Wolf J, Wong HR, Zimmerman JJ, Kissoon N, Tissieres P (2020) Surviving sepsis campaign international guidelines for the management of septic shock and sepsis-associated organ dysfunction in children. Intensive Care Med 46:10–67. https://doi.org/10.1007/s00134-019-05878-6
Stanski NL, Wong HR, Basu RK, Cvijanovich NZ, Fitzgerald JC, Weiss SL, Bigham MT, Jain PN, Schwarz A, Lutfi R, Nowak J, Allen GL, Thomas NJ, Grunwell JR, Quasney M, Haileselassie B, Chawla LS, Goldstein SL (2021) Recalibration of the Renal Angina Index for Pediatric Septic Shock. Kidney Int Rep. https://doi.org/10.1016/j.ekir.2021.04.022
Stanski NL, Stenson EK, Cvijanovich NZ, Weiss SL, Fitzgerald JC, Bigham MT, Jain PN, Schwarz A, Lutfi R, Nowak J, Allen GL, Thomas NJ, Grunwell JR, Baines T, Quasney M, Haileselassie B, Wong HR (2020) PERSEVERE biomarkers predict severe acute kidney injury and renal recovery in pediatric septic shock. Am J Respir Crit Care Med 201:848–855. https://doi.org/10.1164/rccm.201911-2187OC
Basu RK, Standage SW, Cvijanovich NZ, Allen GL, Thomas NJ, Freishtat RJ, Anas N, Meyer K, Checchia PA, Lin R, Shanley TP, Bigham MT, Wheeler DS, Devarajan P, Goldstein SL, Wong HR (2011) Identification of candidate serum biomarkers for severe septic shock-associated kidney injury via microarray. Crit Care 15:R273. https://doi.org/10.1186/cc10554
Goldstein SL, Akcan-Arikan A, Alobaidi R, Askenazi DJ, Bagshaw SM, Barhight M, Barreto E, Bayrakci B, Bignall ONR, Bjornstad E, Brophy PD, Chanchlani R, Charlton JR, Conroy AL, Deep A, Devarajan P, Dolan K, Fuhrman DY, Gist KM, Gorga SM, Greenberg JH, Hasson D, Ulrich EH, Iyengar A, Jetton JG, Krawczeski C, Meigs L, Menon S, Morgan J, Morgan CJ, Mottes T, Neumayr TM, Ricci Z, Selewski D, Soranno DE, Starr M, Stanski NL, Sutherland SM, Symons J, Tavares MS, Vega MW, Zappitelli M, Ronco C, Mehta RL, Kellum J, Ostermann M, Basu RK, Pediatric ADQI Collaborative (2022) Consensus-based recommendations on priority activities to address acute kidney injury in children: a modified Delphi consensus statement. JAMA Netw Open 5:e2229442. https://doi.org/10.1001/jamanetworkopen.2022.29442
Fitzgerald JC, Basu RK, Fuhrman DY, Gorga SM, Hassinger AB, Sanchez-Pinto LN, Selewski DT, Sutherland SM, Akcan-Arikan A, Pediatric Organ Dysfunction Information Update Mandate (PODIUM) Collaborative (2022) Renal dysfunction criteria in critically ill children: The PODIUM Consensus Conference. Pediatrics 149:S66–S73. https://doi.org/10.1542/peds.2021-052888J
Bembea MM, Agus M, Akcan-Arikan A, Alexander P, Basu R, Bennett TD, Bohn D, Brandão LR, Brown A-M, Carcillo JA, Checchia P, Cholette J, Cheifetz IM, Cornell T, Doctor A, Eckerle M, Erickson S, Farris RWD, Faustino EVS, Fitzgerald JC, Fuhrman DY, Giuliano JS, Guilliams K, Gaies M, Gorga SM, Hall M, Hanson SJ, Hartman M, Hassinger AB, Irving SY, Jeffries H, Jouvet P, Kannan S, Karam O, Khemani RG, Niranjan K, Lacroix J, Laussen P, Leclerc F, Lee JH, Leteurtre S, Lobner K, McKiernan PJ, Menon K, Monagle P, Muszynski JA, Odetola F, Parker R, Pathan N, Pierce RW, Pineda J, Prince JM, Robinson KA, Rowan CM, Ryerson LM, Sanchez-Pinto LN, Schlapbach LJ, Selewski DT, Shekerdemian LS, Simon D, Smith LS, Squires JE, Squires RH, Sutherland SM, Ouellette Y, Spaeder MC, Srinivasan V, Steiner ME, Tasker RC, Thiagarajan R, Thomas N, Tissieres P, Traube C, Tucci M, Typpo KV, Wainwright MS, Ward SL, Watson RS, Weiss S, Whitney J, Willson D, Wynn JL, Yeyha N, Zimmerman JJ (2022) Pediatric Organ Dysfunction Information Update Mandate (PODIUM) Contemporary Organ Dysfunction Criteria: Executive Summary. Pediatrics 149:S1–S12. https://doi.org/10.1542/peds.2021-052888B
Chappell MC (2016) Biochemical evaluation of the renin-angiotensin system: the good, bad, and absolute? Am J Physiol Heart Circ Physiol 310:H137–H152. https://doi.org/10.1152/ajpheart.00618.2015
Flannery AH, Ortiz-Soriano V, Li X, Gianella FG, Toto RD, Moe OW, Devarajan P, Goldstein SL, Neyra JA (2021) Serum renin and major adverse kidney events in critically ill patients: a multicenter prospective study. Crit Care 25:294. https://doi.org/10.1186/s13054-021-03725-z
Bellomo R, Forni LG, Busse LW, McCurdy MT, Ham KR, Boldt DW, Hästbacka J, Khanna AK, Albertson TE, Tumlin J, Storey K, Handisides D, Tidmarsh GF, Chawla LS, Ostermann M (2020) Renin and survival in patients given angiotensin II for catecholamine-resistant vasodilatory shock. Am J Respir Crit Care Med. https://doi.org/10.1164/rccm.201911-2172OC
Gleeson PJ, Crippa IA, Mongkolpun W, Cavicchi FZ, Van Meerhaeghe T, Brimioulle S, Taccone FS, Vincent J-L, Creteur J (2019) Renin as a marker of tissue-perfusion and prognosis in critically ill patients. Crit Care Med 47:152–158. https://doi.org/10.1097/CCM.0000000000003544
Nguyen M, Denimal D, Dargent A, Guinot P-G, Duvillard L, Quenot J-P, Bouhemad B (2019) Plasma renin concentration is associated with hemodynamic deficiency and adverse renal outcome in septic shock. Shock 52:e22–e30. https://doi.org/10.1097/SHK.0000000000001285
Wong HR, Caldwell JT, Cvijanovich NZ, Weiss SL, Fitzgerald JC, Bigham MT, Jain PN, Schwarz A, Lutfi R, Nowak J, Allen GL, Thomas NJ, Grunwell JR, Baines T, Quasney M, Haileselassie B, Lindsell CJ (2019) Prospective clinical testing and experimental validation of the Pediatric Sepsis Biomarker Risk Model. Sci Transl Med 11:eaax9000. https://doi.org/10.1126/scitranslmed.aax9000
Schroten NF, Gaillard CAJM, van Veldhuisen DJ, Szymanski MK, Hillege HL, de Boer RA (2012) New roles for renin and prorenin in heart failure and cardiorenal crosstalk. Heart Fail Rev 17:191–201. https://doi.org/10.1007/s10741-011-9262-2
Danser AHJ, Deinum J (2005) Renin, prorenin and the putative (pro)renin receptor. Hypertension 46:1069–1076. https://doi.org/10.1161/01.HYP.0000186329.92187.2e
Wong HR, Cvijanovich NZ, Anas N, Allen GL, Thomas NJ, Bigham MT, Weiss SL, Fitzgerald J, Checchia PA, Meyer K, Quasney M, Hall M, Gedeit R, Freishtat RJ, Nowak J, Raj SS, Gertz S, Howard K, Harmon K, Lahni P, Frank E, Hart KW, Nguyen TC, Lindsell CJ (2016) Pediatric Sepsis Biomarker Risk Model-II: redefining the pediatric sepsis biomarker risk model with septic shock phenotype. Crit Care Med 44:2010–2017. https://doi.org/10.1097/CCM.0000000000001852
Chawla LS, Bellomo R, Bihorac A, Goldstein SL, Siew ED, Bagshaw SM, Bittleman D, Cruz D, Endre Z, Fitzgerald RL, Forni L, Kane-Gill SL, Hoste E, Koyner J, Liu KD, Macedo E, Mehta R, Murray P, Nadim M, Ostermann M, Palevsky PM, Pannu N, Rosner M, Wald R, Zarbock A, Ronco C, Kellum JA, Acute Disease Quality Initiative Workgroup 16 (2017) Acute kidney disease and renal recovery: consensus report of the Acute Disease Quality Initiative (ADQI) 16 Workgroup. Nat Rev Nephrol 13:241
Kellum JA, Lameire N, Aspelin P, Barsoum RS, Burdmann EA, Goldstein SL, Herzog CA, Joannidis M, Kribben A, Levey AS, MacLeod AM, Mehta RL, Murray PT, Naicker S, Opal SM, Schaefer F, Schetz M, Uchino S (2012) Kidney Disease: Improving Global Outcomes (KDIGO) acute kidney injury work group. KDIGO clinical practice guideline for acute kidney injury. Kidney Int Suppl 2:1–138. https://doi.org/10.1038/kisup.2012.1
Basu RK, Hackbarth R, Gillespie S, Akcan-Arikan A, Brophy P, Bagshaw S, Alobaidi R, Goldstein SL (2021) Clinical phenotypes of acute kidney injury are associated with unique outcomes in critically ill septic children. Pediatr Res 90:1031–1038. https://doi.org/10.1038/s41390-021-01363-3
Zappitelli M, Parikh CR, Akcan-Arikan A, Washburn KK, Moffett BS, Goldstein SL (2008) Ascertainment and epidemiology of acute kidney injury varies with definition interpretation. Clin J Am Soc Nephrol 3:948–954. https://doi.org/10.2215/CJN.05431207
Kaddourah A, Basu RK, Bagshaw SM, Goldstein SL, AWARE Investigators (2017) Epidemiology of acute kidney injury in critically ill children and young adults. N Engl J Med 376:11–20. https://doi.org/10.1056/NEJMoa1611391
Pollack MM, Patel KM, Ruttimann UE (1996) PRISM III: an updated Pediatric Risk of Mortality score. Crit Care Med 24:743–752. https://doi.org/10.1097/00003246-199605000-00004
Collaborative Pediatric Critical Care Research Network. Pediatric risk of mortality (PRISM) calculator. https://www.cpccrn.org/calculators/prismiiicalculator/. Accessed 1 June 2022
Gaies MG, Gurney JG, Yen AH, Napoli ML, Gajarski RJ, Ohye RG, Charpie JR, Hirsch JC (2010) Vasoactive–inotropic score as a predictor of morbidity and mortality in infants after cardiopulmonary bypass. Pediatr Crit Care Med 11:234–238. https://doi.org/10.1097/PCC.0b013e3181b806fc
Jeyaraju M, McCurdy MT, Levine AR, Devarajan P, Mazzeffi MA, Mullins KE, Reif M, Yim DN, Parrino C, Lankford AS, Chow JH (2022) Renin kinetics are superior to lactate kinetics for predicting in-hospital mortality in hypotensive critically ill patients. Crit Care Med 50:50–60. https://doi.org/10.1097/CCM.0000000000005143
Barbieri A, Giuliani E, Marchetti G, Ugoletti E, Della Volpe S, Albertini G (2012) Plasma renin concentration as a predictor of outcome in a medical intensive care setting: a retrospective pilot study. Minerva Anestesiol 78:1248–1253
Bellomo R, Wunderink RG, Szerlip H, English SW, Busse LW, Deane AM, Khanna AK, McCurdy MT, Ostermann M, Young PJ, Handisides DR, Chawla LS, Tidmarsh GF, Albertson TE (2020) Angiotensin I and angiotensin II concentrations and their ratio in catecholamine-resistant vasodilatory shock. Crit Care 24:43. https://doi.org/10.1186/s13054-020-2733-x
Zhang W, Chen X, Huang L, Lu N, Zhou L, Wu G, Chen Y (2014) Severe sepsis: low expression of the renin-angiotensin system is associated with poor prognosis. Exp Ther Med 7:1342–1348. https://doi.org/10.3892/etm.2014.1566
Tumlin JA, Murugan R, Deane AM, Ostermann M, Busse LW, Ham KR, Kashani K, Szerlip HM, Prowle JR, Bihorac A, Finkel KW, Zarbock A, Forni LG, Lynch SJ, Jensen J, Kroll S, Chawla LS, Tidmarsh GF, Bellomo R (2018) Outcomes in patients with vasodilatory shock and renal replacement therapy treated with intravenous angiotensin II. Crit Care Med 46:949–957. https://doi.org/10.1097/CCM.0000000000003092
Narumi K, Hirose T, Sato E, Mori T, Kisu K, Ishikawa M, Totsune K, Ishii T, Ichihara A, Nguyen G, Sato H, Ito S (2015) A functional (pro)renin receptor is expressed in human lymphocytes and monocytes. Am J Physiol Renal Physiol 308:F487-499. https://doi.org/10.1152/ajprenal.00206.2014
Goldstein SL, Krallman KA, Kirby C, Roy J-P, Collins M, Fox K, Schmerge A, Wilder S, Gerhardt B, Chima R, Basu RK, Chawla L, Fei L (2022) Integration of the Renal Angina Index and urine neutrophil gelatinase-associated lipocalin improves severe acute kidney injury prediction in critically ill children and young adults. Kidney Int Rep 7:1842–1849. https://doi.org/10.1016/j.ekir.2022.05.021
Odum JD, Wong HR, Stanski NL (2021) A precision medicine approach to biomarker utilization in pediatric sepsis-associated acute kidney injury. Front Pediatr 9:313. https://doi.org/10.3389/fped.2021.632248
Acknowledgements
The authors thank the late Dr. Hector Wong, the leader of this multicenter study of pediatric septic shock for over a decade and a mentor to all of us. He was intimately involved in the conceptualization of this project, although he tragically passed before the data were analyzed and the manuscript was written. The authors also thank Patrick Lahni and Kelli Harmon for technical assistance in the conduct of this study.
Funding
This work was supported by the National Center for Advancing Translational Sciences of the National Institutes of Health (KL2TR001426). The original study was funded by National Institute of General Medical Sciences, R35GM126943 (PI: Hector R. Wong). The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIH.
Author information
Authors and Affiliations
Contributions
Conceptualization/methodology/formal analysis and investigation/writing, original draft and preparation: NLS, NPS, BZ, SLG. Data acquisition: NLS, NZC, JCF, PNJ, AJS, JN, GLA, NJT, BH. Writing, review and editing: NLS, NPS, BZ, SLG, NZC, JCF, PNJ, AJS, JN, GLA, NJT, BH. Funding acquisition: NLS.
Corresponding author
Ethics declarations
NLS is supported by the National Center for Advancing Translational Sciences of the National Institutes of Health (KL2TR001426). JCF is supported by the National Institutes of Health National Institute of Diabetes and Digestive and Kidney Diseases (K23DK119463). The remainder of the authors report no financial disclosures or conflict of interest relevant to this work.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Stanski, N.L., Pode Shakked, N., Zhang, B. et al. Serum renin and prorenin concentrations predict severe persistent acute kidney injury and mortality in pediatric septic shock. Pediatr Nephrol 38, 3099–3108 (2023). https://doi.org/10.1007/s00467-023-05930-0
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00467-023-05930-0