Abstract
Introduction
In patients with benign and refractory esophageal strictures (BES), repeating initial dilations in short intervals could be recommended, but little data are available to validate this strategy. Our aim was to evaluate long-term results of a scheduled program of repeated and sustained esophageal dilations in patients with refractory strictures.
Methods
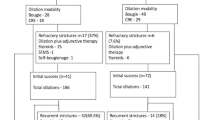
Patients with BES requiring five or more dilations were retrospectively included and divided in two groups for analysis: a SCHEDULED group (SDG) where patients were systematically rescheduled for the 5 first dilations; ON-DEMAND group (ODG) where patients were dilated only in case of recurrence of the dysphagia. Comparison between SDG and ODG was done with a 1:1 matching analysis and etiology of stricture. Clinical success was defined as the absence of dysphagia for more than a year.
Results
39 patients with refractory BES were included with post-operative stenosis in 51.2% and post-caustic injury 28.2%; 10 were in SDG and 29 in ODG. In overall analysis (39 patients), the follow-up was 64.4 ± 32 months, success rate was 79.5% and duration of treatment was 27.3 ± 20 months, and mean number of dilations was 11.7 per patient. The need for dilations decreased significantly after 18 months of treatment with an average of 0.56 dilations per semester. Self-expandable metallic stent insertion was associated with an increased rate of complications (5.9% vs 59.1% p = 0.001). In matched analysis (10 ODG vs 10 SDG patients), the duration of treatment was lower in SDG (18.8 vs 41.4 months, p = 0,032) with a higher probability of remission (survival analysis, Log-rank: p = 0,019) and the success rate did not differ between ODG and SDG patients (80% vs 90%; NS).
Conclusion
Overall, long-term esophageal dilations resulted in a 79.5% success rate and the need for further dilatations decreased significantly in both groups after 18-month follow-up. A scheduled dilation program was associated with a higher probability of final success and lower treatment duration.



Similar content being viewed by others
References
Pereira-Lima JC, Ramires RP, Zamin I et al (1999) Endoscopic dilation of benign esophageal strictures: report on 1043 procedures. Am J Gastroenterol 94:1497–1501
Kochhar R, Makharia GK (2002) Usefulness of intralesional triamcinolone in treatment of benign esophageal strictures. Gastrointest Endosc 56:829–834
Cox JG, Winter RK, Maslin SC et al (1988) Balloon or bougie for dilatation of benign oesophageal stricture? An interim report of a randomised controlled trial. Gut 29:1741–1747
Yamamoto H, Hughes RW, Schroeder KW et al (1992) Treatment of benign esophageal stricture by Eder-Puestow or balloon dilators: a comparison between randomized and prospective nonrandomized trials. Mayo Clin Proc 67:228–236
Saeed ZA, Winchester CB, Ferro PS et al (1995) Prospective randomized comparison of polyvinyl bougies and through-the-scope balloons for dilation of peptic strictures of the esophagus. Gastrointest Endosc 41:189–195
van Boeckel PGA, Siersema PD (2015) Refractory esophageal strictures: what to do when dilation fails. Curr Treat Options Gastroenterol 13:47–58
Repici A, Small AJ, Mendelson A et al (2016) Natural history and management of refractory benign esophageal strictures. Gastrointest Endosc 84:222–228
Kochman ML, McClave SA, Boyce HW (2005) The refractory and the recurrent esophageal stricture: a definition. Gastrointest Endosc 62:474–475
Ramage JI, Rumalla A, Baron TH et al (2005) A prospective, randomized, double-blind, placebo-controlled trial of endoscopic steroid injection therapy for recalcitrant esophageal peptic strictures. Am J Gastroenterol 100:2419–2425
Altintas E, Kacar S, Tunc B et al (2004) Intralesional steroid injection in benign esophageal strictures resistant to bougie dilation. J Gastroenterol Hepatol 19:1388–1391
Hirdes MMC, van Hooft JE, Koornstra JJ et al (2013) Endoscopic corticosteroid injections do not reduce dysphagia after endoscopic dilation therapy in patients with benign esophagogastric anastomotic strictures. Clin Gastroenterol Hepatol 11(795–801):e1
Camargo MA, Lopes LR, de Grangeia T et al (2003) Use of corticosteroids after esophageal dilations on patients with corrosive stenosis: prospective, randomized and double-blind study. Rev Assoc Med Bras 49:286–292
Hordijk ML, Siersema PD, Tilanus HW et al (2006) Electrocautery therapy for refractory anastomotic strictures of the esophagus. Gastrointest Endosc 63:157–163
Yano T, Yoda Y, Satake H et al (2013) Radial incision and cutting method for refractory stricture after nonsurgical treatment of esophageal cancer. Endoscopy 45:316–319
Hordijk ML, van Hooft JE, Hansen BE et al (2009) A randomized comparison of electrocautery incision with Savary bougienage for relief of anastomotic gastroesophageal strictures. Gastrointest Endosc 70:849–855
Eloubeidi MA, Talreja JP, Lopes TL et al (2011) Success and complications associated with placement of fully covered removable self-expandable metal stents for benign esophageal diseases (with videos). Gastrointest Endosc 73:673–681
Fuccio L, Hassan C, Frazzoni L et al (2015) Clinical outcomes following stent placement in refractory benign esophageal stricture: a systematic review and meta-analysis. Endoscopy 48:141–148
Javed A, Pal S, Dash NR et al (2011) Outcome Following Surgical Management of Corrosive Strictures of the Esophagus. Ann Surg 254:62–66
Sami SS, Haboubi HN, Ang Y et al (2018) UK guidelines on oesophageal dilatation in clinical practice. Gut 67:1000–1023
Chiu Y-C, Hsu C-C, Chiu K-W et al (2004) Factors Influencing Clinical Applications of Endoscopic Balloon Dilation for Benign Esophageal Strictures. Endoscopy 36:595–600
Park JY, Song H-Y, Kim JH et al (2012) Benign Anastomotic Strictures After Esophagectomy: Long-Term Effectiveness of Balloon Dilation and Factors Affecting Recurrence in 155 Patients. Am J Roentgenol 198:1208–1213
Saeed ZA, Ramirez FC, Hepps KS et al (1997) An objective end point for dilation improves outcome of peptic esophageal strictures: a prospective randomized trial. Gastrointest Endosc 45:354–359
Tringali A, Barbaro F, Pizzicannella M et al (2016) Endoscopic management with multiple plastic stents of anastomotic biliary stricture following liver transplantation: long-term results. Endoscopy 48:546–551
Wolfram D, Tzankov A, Pülzl P et al (2009) Hypertrophic scars and keloids–a review of their pathophysiology, risk factors, and therapeutic management. Dermatol Surg 35:171–181
Mahdavian Delavary B, van der Veer WM, Ferreira JA et al (2012) Formation of hypertrophic scars: evolution and susceptibility. J Plast Surg Hand Surg 46:95–101
Costa AM, Peyrol S, Pôrto LC et al (1999) Mechanical forces induce scar remodeling Study in non-pressure-treated versus pressure-treated hypertrophic scars. Am J Pathol 155:1671–1679
Chirica M, Veyrie N, Munoz-Bongrand N et al (2010) Late Morbidity After Colon Interposition for Corrosive Esophageal Injury. Ann Surg 252:271–280
Kim JH, Song H-Y, Choi EK et al (2009) Temporary metallic stent placement in the treatment of refractory benign esophageal strictures: results and factors associated with outcome in 55 patients. Eur Radiol 19:384–390
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
Dr. Marc Barthet, Véronique Vitton, Jean-Michel Gonzalez, MD. Véronique Vitton, and Antoine Debourdeau declare that they have no conflicts of interest or financial ties to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Debourdeau, A., Barthet, M., Benezech, A. et al. Assessment of long-term results of repeated dilations and impact of a scheduled program of dilations for refractory esophageal strictures: a retrospective case–control study. Surg Endosc 36, 1098–1105 (2022). https://doi.org/10.1007/s00464-021-08376-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-021-08376-3