Abstract
Background
Success rate of endoscopic dilation (ED) of complex benign esophageal strictures (CBES) can be as low as 65%. Since EDs are usually performed at 2–4-week intervals, the aim of this study was to evaluate the clinical outcomes of EDs done initially at weekly intervals.
Methods
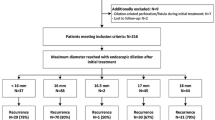
A cohort of patients with CBES (luminal diameter < 10 mm) underwent ED at weekly intervals and subsequent dilation intervals adjusted based on response. Weekly EDs were also re-initiated in those requiring additional interventions (electro-cautery/stents). Group A patients: Failed prior EDs done at ≥ 2-week intervals. Group B: CBES with no prior dilations. Success was defined as achieving and maintaining a luminal diameter of ≥ 14 mm and patient remaining dysphagia-free with minimal re-interventions.
Results
488 EDs were performed on a cohort of 57 consecutive patients with CBES. Median follow-up was 4 years. Group A: 21 patients (mean age 65 ± 13 years; mean interval between prior failed dilations 17 ± 9 days). 57% of these patients achieved long-term success with weekly dilations (mean 8 ± 4.7 dilations/patient). Group B: 36 patients (mean age 61 ± 13 years, mean 6.5 ± 5.5 dilations/patient). Long-term success was 83.3% (P = 0.033). Despite weekly dilations, unable to achieve a diameter of 14 mm in 5 patients. AE: perforation 1 (0.2%), bleeding 1 (0.2%).
Conclusion
Significant proportion of patients with CBES who failed prior dilations done at ≥ 2-week intervals achieved dysphagia-free status by initiating weekly dilations. Hence, before considering other options (electro-cautery/stents), one can consider using this approach. This approach can also be used upfront in patients with newly diagnosed CBES.
Graphical abstract





Similar content being viewed by others
Abbreviations
- ED:
-
Endoscopic dilation
- CBES:
-
Complex benign esophageal stricture
- RBES:
-
Refractory benign esophageal stricture
- FC-SEMS:
-
Fully covered self-expanding metal esophageal stent
- LAMS:
-
Lumen apposing metal stent
- AE:
-
Adverse events
References
Sami SS et al (2018) UK guidelines on oesophageal dilatation in clinical practice. Gut 67(6):1000–1023
Poincloux L, Rouquette O, Abergel A (2017) Endoscopic treatment of benign esophageal strictures: a literature review. Expert Rev Gastroenterol Hepatol 11(1):53–64
Robles-Medranda C et al (2019) Treating simple benign esophageal strictures with Savary-Gilliard dilators: is the rule of three still necessary? Arq Gastroenterol 56(1):95–98
Pereira-Lima JC et al (1999) Endoscopic dilation of benign esophageal strictures: report on 1043 procedures. Am J Gastroenterol 94(6):1497–1501
Persson ST, Fraser AG, Lane MR (1999) Long-term follow-up of the management of benign oesophageal strictures at Auckland Hospital 1990–1994. N Z Med J 112(1081):28–30
Kochman ML, McClave SA, Boyce HW (2005) The refractory and the recurrent esophageal stricture: a definition. Gastrointest Endosc 62(3):474–475
Vermeulen BD et al (2020) Risk factors and clinical outcomes of endoscopic dilation in benign esophageal strictures: a long-term follow-up study. Gastrointest Endosc 91(5):1058–1066
Badir M et al (2021) Endoscopic dilation of benign post-esophagectomy anastomotic strictures: long-term outcomes and risk of recurrence. Ann Gastroenterol 34(3):337–343
Honda M et al (2010) Process of healing of mucosal defects in the esophagus after endoscopic mucosal resection: histological evaluation in a dog model. Endoscopy 42(12):1092–1095
Kakushima N et al (2006) Histopathologic characteristics of gastric ulcers created by endoscopic submucosal dissection. Endoscopy 38(4):412–415
Mellow MH, Pinkas H (1985) Endoscopic laser therapy for malignancies affecting the esophagus and gastroesophageal junction. Analysis of technical and functional efficacy. Arch Intern Med 145(8):1443–1446
van Halsema EE et al (2017) Endoscopic dilation of benign esophageal anastomotic strictures over 16 mm has a longer lasting effect. Surg Endosc 31(4):1871–1881
Beilstein MC, Kochman ML (2005) Endoscopic incision of a refractory esophageal stricture: novel management with an endoscopic scissors. Gastrointest Endosc 61(4):623–625
Choi J, Choi SI (2021) A new simple endoscopic incision therapy for refractory benign oesophageal anastomotic stricture. BMJ Case Rep 14(3).
Hordijk ML et al (2006) Electrocautery therapy for refractory anastomotic strictures of the esophagus. Gastrointest Endosc 63(1):157–163
Schubert D et al (2003) Endoscopic treatment of benign gastrointestinal anastomotic strictures using argon plasma coagulation in combination with diathermy. Surg Endosc 17(10):1579–1582
Li J et al (2020) Endoscopic incision and selective cutting for primary treatment of benign esophageal anastomotic stricture: outcomes of 5 cases with a minimum follow-up of 12 months. Ann Palliat Med 9(3):1206–1210
Adler DG (2017) Esophageal placement of a lumen-apposing metal stent in a patient with a chronic anastomotic stricture. Gastrointest Endosc 85(6):1291–1293
Irani S et al (2017) Use of a lumen-apposing metal stent to treat GI strictures (with videos). Gastrointest Endosc 85(6):1285–1289
Tandon S et al (2019) Self-expanding esophageal stents for the management of benign refractory esophageal strictures in children: a systematic review and review of outcomes at a single center. J Pediatr Surg 54(12):2479–2486
Lange B, et al (2018) Experience with fully covered self-expandable metal stents for anastomotic stricture following esophageal atresia repair. Dis Esophagus 31(11).
Manfredi MA et al (2014) Externally removable stents in the treatment of benign recalcitrant strictures and esophageal perforations in pediatric patients with esophageal atresia. Gastrointest Endosc 80(2):246–252
Liu J et al (2012) Removable, fully covered, self-expandable metal stents for the treatment of refractory benign esophagogastric anastomotic strictures. Dysphagia 27(2):260–264
Dua KS et al (2008) Removable self-expanding plastic esophageal stent as a continuous, non-permanent dilator in treating refractory benign esophageal strictures: a prospective two-center study. Am J Gastroenterol 103(12):2988–2994
Granata A et al (2020) Endoscopic management of post-surgical GI wall defects with the overstitch endosuturing system: a single-center experience. Surg Endosc 34(9):3805–3817
Dolezel R et al (2018) Fixation of biomaterial to metallic stent and fixation of stents after circular endoscopic dissection in the esophagus on an animal model. Rozhl Chir 97(5):208–213
Dzeletovic I et al (2013) Self-dilation as a treatment for resistant, benign esophageal strictures. Dig Dis Sci 58(11):3218–3223
van Halsema EE et al (2018) Self-dilation for therapy-resistant benign esophageal strictures: towards a systematic approach. Surg Endosc 32(7):3200–3207
Abdelhay S, Mousa M, Elsherbeny MS (2020) Corticosteroid injection of impassable caustic esophageal strictures without dilatation: does it pave the way to interval endoscopic dilatation? J Pediatr Surg 55(11):2348–2351
Dasari CS et al (2020) Intralesional steroids and endoscopic dilation for anastomotic strictures after esophagectomy: systematic review and meta-analysis. Endoscopy 52(9):721–726
Henskens N, Wauters L, Vanuytsel T (2020) Intralesional steroid injections in addition to endoscopic dilation in benign refractory esophageal strictures : a systematic review. Acta Gastroenterol Belg 83(3):432–440
Nie D, Yan X, Huang Y (2020) Efficacy of hydrocortisone sodium succinate and aluminum phosphate gel for stricture prevention after >/=3/4 circumferential endoscopic submucosal dissection. J Int Med Res 48(4):300060519894122
Honda M et al (2011) Use of adipose tissue-derived stromal cells for prevention of esophageal stricture after circumferential EMR in a canine model. Gastrointest Endosc 73(4):777–784
Sakurai T et al (2007) Autologous buccal keratinocyte implantation for the prevention of stenosis after EMR of the esophagus. Gastrointest Endosc 66(1):167–173
Ohki T et al (2006) Treatment of oesophageal ulcerations using endoscopic transplantation of tissue-engineered autologous oral mucosal epithelial cell sheets in a canine model. Gut 55(12):1704–1710
Kanai N et al (2012) Fabricated autologous epidermal cell sheets for the prevention of esophageal stricture after circumferential ESD in a porcine model. Gastrointest Endosc 76(4):873–881
Takagi R et al (2012) Cell sheet technology for regeneration of esophageal mucosa. World J Gastroenterol 18(37):5145–5150
Ohki T, et al (2012) Prevention of esophageal stricture after endoscopic submucosal dissection using tissue-engineered cell sheets. Gastroenterology 143(3):582–588 e2.
Sasaki R et al (2012) Punch and spindle-shaped biopsies for collecting oral mucosal tissue for the fabrication of transplantable autologous epithelial cell sheets. J Biomed Mater Res A 100(10):2849–2854
Liu Y et al (2021) Autologous esophageal mucosa with polyglycolic acid transplantation and temporary stent implantation can prevent stenosis after circumferential endoscopic submucosal dissection. Ann Transl Med 9(7):546
Ohki T, Yamamoto M (2020) Esophageal regenerative therapy using cell sheet technology. Regen Ther 13:8–17
Dua KS, Sasikala M (2018) Repairing the human esophagus with tissue engineering. Gastrointest Endosc 88(4):579–588
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
Sowmya Palam, Mathew Mohorek, Syed Rizvi and Kulwinder Dua have declare no conflict of interest or financial ties to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Supplementary file1 (WMV 23823 kb)
Rights and permissions
About this article
Cite this article
Palam, S., Mohorek, M., Rizvi, S. et al. Clinical outcomes on weekly endoscopic dilations as the initial approach to manage patients with complex benign esophageal strictures: report on 488 dilations. Surg Endosc 36, 7056–7065 (2022). https://doi.org/10.1007/s00464-022-09248-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-022-09248-0