Abstract
Background
The addition of lateral pelvic lymph node dissection (LPLND) in rectal cancer surgery has been reported to increase the incidence of post-operative urinary retention. Here, we assessed the predictive factors and long-term outcomes of urinary retention following laparoscopic LPLND (L-LPLND) with total mesorectal excision (TME) for advanced lower rectal cancer.
Methods
This retrospective single-institutional study reviewed post-operative urinary retention in 71 patients with lower rectal cancer who underwent L-LPLND with TME. Patients with preoperative urinary dysfunction or who underwent unilateral LPLND were excluded. Detailed information regarding patient clinicopathologic characteristics, post-void residual urine volume, and the presence or absence of urinary retention over time was collected from clinical and histopathologic reports and telephone surveys. Urinary retention was defined as residual urine > 100 mL and the need for further treatment.
Results
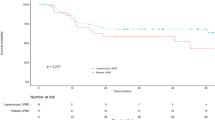
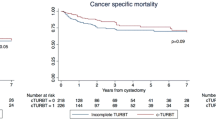
Post-operative urinary retention was observed in 25/71 patients (35.2%). Multivariate analysis revealed that blood loss ≥ 400 mL [odds ratio (OR) 4.52; 95% confidence interval (CI) 1.24–16.43; p = 0.018] and inferior vesical artery (IVA) resection (OR 8.28; 95% CI 2.46–27.81; p < 0.001) were independently correlated with the incidence of urinary retention. Furthermore, bilateral IVA resection caused urinary retention in more patients than unilateral IVA resection (88.9% vs 47.1%, respectively; p = 0.049). Although urinary retention associated with unilateral IVA resection improved relatively quickly, urinary retention associated with bilateral IVA resection tended to persist over 1 year.
Conclusion
We identified the predictive factors of urinary retention following L-LPLND with TME, including increased blood loss (≥ 400 mL) and IVA resection. Urinary retention associated with unilateral IVA resection improved relatively quickly. L-LPLND with unilateral IVA resection is a feasible and safe procedure to improve oncological curability. However, if oncological curability is guaranteed, bilateral IVA resection should be avoided to prevent irreversible urinary retention.



Similar content being viewed by others
References
MacFarlane JK, Ryall RD, Heald RJ (1993) Mesorectal excision for rectal cancer. Lancet 341:457–460
Heald RJ, Moran BJ, Ryall RD, Sexton R, MacFarlane JK (1998) Rectal cancer: the Basingstoke experience of total mesorectal excision, 1978–1997. Arch Surg 133:894–899
Dahlberg M, Pahlman L, Bergstrom R, Glimelius B (1998) Improved survival in patients with rectal cancer: a population-based register study. Br J Surg 85:515–520
Maurer CA, Z’Graggen K, Renzulli P, Schilling MK, Netzer P, Buchler MW (2001) Total mesorectal excision preserves male genital function compared with conventional rectal cancer surgery. Br J Surg 88:1501–1505
Pocard M, Zinzindohoue F, Haab F, Caplin S, Parc R, Tiret E (2002) A prospective study of sexual and urinary function before and after total mesorectal excision with autonomic nerve preservation for rectal cancer. Surgery 131:368–372
Ito M, Kobayashi A, Fujita S, Mizusawa J, Kanemitsu Y, Kinugasa Y, Komori K, Ohue M, Ota M, Akazai Y, Shiozawa M, Yamaguchi T, Akasu T, Moriya Y, Colorectal cancer study group of Japan clinical oncology G (2018) Urinary dysfunction after rectal cancer surgery: results from a randomized trial comparing mesorectal excision with and without lateral lymph node dissection for clinical stage II or III lower rectal cancer (Japan Clinical Oncology Group Study, JCOG0212). Eur J Surg Oncol 44:463–468
Kyo K, Sameshima S, Takahashi M, Furugori T, Sawada T (2006) Impact of autonomic nerve preservation and lateral node dissection on male urogenital function after total mesorectal excision for lower rectal cancer. World J Surg 30:1014–1019
Nagawa H, Muto T, Sunouchi K, Higuchi Y, Tsurita G, Watanabe T, Sawada T (2001) Randomized, controlled trial of lateral node dissection vs. nerve-preserving resection in patients with rectal cancer after preoperative radiotherapy. Dis Colon Rectum 44:1274–1280
Toritani K, Watanabe J, Suwa Y, Suzuki S, Nakagawa K, Suwa H, Ishibe A, Ota M, Kunisaki C, Endo I (2019) The risk factors for urinary dysfunction after autonomic nerve-preserving rectal cancer surgery: a multicenter retrospective study at Yokohama Clinical Oncology Group (YCOG1307). Int J Colorectal Dis 34:1697–1703
Kin C, Rhoads KF, Jalali M, Shelton AA, Welton ML (2013) Predictors of postoperative urinary retention after colorectal surgery. Dis Colon Rectum 56:738–746
Hashiguchi Y, Muro K, Saito Y, Ito Y, Ajioka Y, Hamaguchi T, Hasegawa K, Hotta K, Ishida H, Ishiguro M, Ishihara S, Kanemitsu Y, Kinugasa Y, Murofushi K, Nakajima TE, Oka S, Tanaka T, Taniguchi H, Tsuji A, Uehara K, Ueno H, Yamanaka T, Yamazaki K, Yoshida M, Yoshino T, Itabashi M, Sakamaki K, Sano K, Shimada Y, Tanaka S, Uetake H, Yamaguchi S, Yamaguchi N, Kobayashi H, Matsuda K, Kotake K, Sugihara K (2020) Japanese society for Cancer of the Colon and Rectum (JSCCR) guidelines 2019 for the treatment of colorectal cancer. Int J Clin Oncol 25:1–42
Matsuoka N, Moriya Y, Akasu T, Fujita S (2001) Long-term outcome of urinary function after extended lymphadenectomy in patients with distal rectal cancer. Eur J Surg Oncol 27:165–169
Col C, Hasdemir O, Yalcin E, Guzel H, Tunc G, Bilgen K, Kucukpinar T (2005) The assessment of urinary function following extended lymph node dissection for colorectal cancer. Eur J Surg Oncol 31:237–241
Maeda K, Maruta M, Utsumi T, Sato H, Toyama K, Matsuoka H (2003) Bladder and male sexual functions after autonomic nerve-sparing TME with or without lateral node dissection for rectal cancer. Tech Coloproctol 7:29–33
Akasu T, Sugihara K, Moriya Y (2009) Male urinary and sexual functions after mesorectal excision alone or in combination with extended lateral pelvic lymph node dissection for rectal cancer. Ann Surg Oncol 16:2779–2786
Matsuoka H, Masaki T, Sugiyama M, Atomi Y (2005) Impact of lateral pelvic lymph node dissection on evacuatory and urinary functions following low anterior resection for advanced rectal carcinoma. Langenbecks Arch Surg 390:517–522
Georgiou P, Tan E, Gouvas N, Antoniou A, Brown G, Nicholls RJ, Tekkis P (2009) Extended lymphadenectomy versus conventional surgery for rectal cancer: a meta-analysis. Lancet Oncol 10:1053–1062
Uyama I, Sugioka A, Matsui H, Fujita J, Komori Y, Hanai T, Hasumi A (2001) Laparoscopic lateral node dissection with autonomic nerve preservation for advanced lower rectal cancer. J Am Coll Surg 193:579–584
Konishi T, Kuroyanagi H, Oya M, Ueno M, Fujimoto Y, Akiyoshi T, Yoshimatsu H, Watanabe T, Yamaguchi T, Muto T (2011) Multimedia article. Lateral lymph node dissection with preoperative chemoradiation for locally advanced lower rectal cancer through a laparoscopic approach. Surg Endosc 25:2358–2359
Akiyoshi T, Nagata J, Nagasaki T, Konishi T, Fujimoto Y, Nagayama S, Fukunaga Y, Ueno M (2015) Laparoscopic salvage lateral pelvic lymph node dissection for locally recurrent rectal cancer. Colorectal Dis 17:O213–O216
Hasegawa S, Nishikawa G, Hida K, Kawada K, Sakai Y (2015) Laparoscopic pelvic sidewall dissection with combined resection of internal iliac vessels for local recurrence of rectal cancer. Tech Coloproctol 19:659–660
Nagayoshi K, Ueki T, Manabe T, Moriyama T, Yanai K, Oda Y, Tanaka M (2016) Laparoscopic lateral pelvic lymph node dissection is achievable and offers advantages as a minimally invasive surgery over the open approach. Surg Endosc 30:1938–1947
Yamaguchi T, Konishi T, Kinugasa Y, Yamamoto S, Akiyoshi T, Okamura R, Ito M, Nishimura Y, Shiozawa M, Yamaguchi S, Hida K, Sakai Y, Watanabe M (2017) Laparoscopic versus open lateral lymph node dissection for locally advanced low rectal cancer: a subgroup analysis of a large multicenter cohort study in Japan. Dis Colon Rectum 60:954–964
Ichihara M, Ikeda M, Uemura M, Miyake M, Miyazaki M, Kato T, Sekimoto M (2019) Feasibility and safety of laparoscopic lateral pelvic lymph node dissection for locally recurrent rectal cancer and risk factors for re-recurrence. Asian J Endosc Surg. https://doi.org/10.1111/ases.12778
Manabe T, Koga Y, Kubo H, Baba K, Nagayoshi K, Nagai S, Ueki T, Nakamura M, Noshiro H (2019) Adverse effects on the postoperative urinary function after combined resection of inferior vesical artery in laparoscopic lateral pelvic lymph node dissection: retrospective analysis of consecutive 95 series. Surg Laparosc Endosc Percutan Tech 29:493–497
Kim HJ, Choi GS, Park JS, Park SY, Yang CS, Lee HJ (2018) The impact of robotic surgery on quality of life, urinary and sexual function following total mesorectal excision for rectal cancer: a propensity score-matched analysis with laparoscopic surgery. Colorectal Dis 20:O103–O113
Fujita S, Akasu T, Mizusawa J, Saito N, Kinugasa Y, Kanemitsu Y, Ohue M, Fujii S, Shiozawa M, Yamaguchi T, Moriya Y, Colorectal cancer study group of Japan clinical oncology G (2012) Postoperative morbidity and mortality after mesorectal excision with and without lateral lymph node dissection for clinical stage II or stage III lower rectal cancer (JCOG0212): results from a multicentre, randomised controlled, non-inferiority trial. Lancet Oncol 13:616–621
Oh SJ, Ku JH, Lim SH, Jeon HG, Son H (2006) Effect of a ‘centralized intensive education system’ for clean intermittent self-catheterization in patients with voiding dysfunction who start catheterization for the first time. Int J Urol 13:905–909
Huang AJ, Brown JS, Boyko EJ, Moore EE, Scholes D, Walter LC, Lin F, Vittinghoff E, Fihn SD (2011) Clinical significance of postvoid residual volume in older ambulatory women. J Am Geriatr Soc 59:1452–1458
Asimakopoulos AD, De Nunzio C, Kocjancic E, Tubaro A, Rosier PF, Finazzi-Agro E (2016) Measurement of post-void residual urine. Neurourol Urodyn 35:55–57
Yamaguchi T, Kinugasa Y, Shiomi A, Tomioka H, Kagawa H (2016) Robotic-assisted laparoscopic versus open lateral lymph node dissection for advanced lower rectal cancer. Surg Endosc 30:721–728
Lange MM, Maas CP, Marijnen CA, Wiggers T, Rutten HJ, Kranenbarg EK, van de Velde CJ, Cooperative Clinical Investigators of the Dutch Total Mesorectal Excision T (2008) Urinary dysfunction after rectal cancer treatment is mainly caused by surgery. Br J Surg 95:1020–1028
Thurmond P, Yang JH, Azadzoi KM (2016) LUTS in pelvic ischemia: a new concept in voiding dysfunction. Am J Physiol Renal Physiol 310:F738–F743
Collado A, Batista JE, Garcia-Penit J, Gelabert A, Arano P, Villavicencio H (2005) Bladder blood flow and de-obstructive open prostatectomy: correlation with clinical and urodynamic parameters. Int Urol Nephrol 37:79–87
Batista JE, Wagner JR, Azadzoi KM, Krane RJ, Siroky MB (1996) Direct measurement of blood flow in the human bladder. J Urol 155:630–633
de Treigny OM, Roumiguie M, Deudon R, de Bonnecaze G, Carfagna L, Chaynes P, Rimailho J, Chantalat E (2017) Anatomical study of the inferior vesical artery: is it specific to the male sex? Surg Radiol Anat 39:961–965
Davies MR (1997) Anatomy of the nerve supply of the rectum, bladder, and internal genitalia in anorectal dysgenesis in the male. J Pediatr Surg 32:536–541
Kim HJ, Choi GS, Park JS, Park SY, Lee HJ, Woo IT, Park IK (2018) Selective lateral pelvic lymph node dissection: a comparative study of the robotic versus laparoscopic approach. Surg Endosc 32:2466–2473
Pollack J, Holm T, Cedermark B, Altman D, Holmstrom B, Glimelius B, Mellgren A (2006) Late adverse effects of short-course preoperative radiotherapy in rectal cancer. Br J Surg 93:1519–1525
Peeters KC, van de Velde CJ, Leer JW, Martijn H, Junggeburt JM, Kranenbarg EK, Steup WH, Wiggers T, Rutten HJ, Marijnen CA (2005) Late side effects of short-course preoperative radiotherapy combined with total mesorectal excision for rectal cancer: increased bowel dysfunction in irradiated patients—a Dutch colorectal cancer group study. J Clin Oncol 23:6199–6206
Acknowledgements
This work was supported by JSPS KAKENHI Grant Number 20K17621. We thank Melissa Crawford, PhD, from Edanz Group (https://en-author-services.edanz.com/ac) for editing a draft of this manuscript.
Funding
This work was supported by JSP KAKENHI Grant Number 20K17621.
Author information
Authors and Affiliations
Contributions
YS, KH, SN, and TM are responsible for conception and design. YS, KH, MS, YM, KN, and HF are responsible for acquisition of data. YS, KH, and SN performed analysis and interpretation of data. YS, TU, and MN are responsible for drafting the article or critically revising it for important intellectual content. YS, KH, MS, YM, KN, HF, SN, TM, TU, and MN gave final approval of the version to be published.
Corresponding author
Ethics declarations
Disclosures
Yoshihiko Sadakari, Kyoko Hisano, Masafumi Sada, Yusuke Mizuuchi, Kinuko Nagayoshi, Hayato Fujita, Shuntaro Nagai, Tatsuya Manabe, Takashi Ueki, and Masafumi Nakamura have no conflicts of interest or financial ties to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Sadakari, Y., Hisano, K., Sada, M. et al. Long-term effects of laparoscopic lateral pelvic lymph node dissection on urinary retention in rectal cancer. Surg Endosc 36, 999–1007 (2022). https://doi.org/10.1007/s00464-021-08364-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-021-08364-7