Abstract
Introduction
The SAGES Fundamental Use of Surgical Energy (FUSE) program accompanied by a bench-top simulation has shown to improve knowledge of the safe use of energy devices. However, there are significant barriers and costs associated with delivering an effective structured simulation curriculum to a widespread international audience. The purpose of this study was to evaluate if bench-top simulation FUSE curriculum through telementoring is as effective as a live-in house proctor for electrosurgical training.
Methods
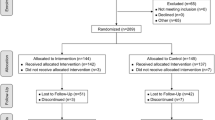
A two-armed multi-institutional randomized controlled trial was designed, including a 1-h didactic electrosurgery course (FUSE curriculum), followed by a structured 1-h bench-top simulation training session. For the simulation, participants were randomized to either a live proctor who delivered the course on-site (LIVE group), or a proctor from a remote location using videoconferencing platform (TELEM group). Pre- and post-curriculum (immediate and 6 months) knowledge and self-perceived comfort and competence were assessed. Data are expressed as median [interquartile range], *p < 0.05.
Results
Sixty-five (35 LIVE; 30 TELEM) surgical trainees from three institutions participated. Baseline characteristics were similar. Total score on the exam improved from 47% [40–54] to 78% [71–84]* amongst all participants, with similar immediate post-curriculum scores in the LIVE group compared to the TELEM group (77% [69–83] vs 80% [75–85]). At 6 months, performance on the exam declined significantly for both groups, but remained similar between the two (LIVE: 59% [51–71] vs TELEM: 71% [57–77]). Participants in both groups reported feeling greater comfort and competence post-curriculum (immediate and at 6 months) compared to baseline, with no difference between the two groups.
Conclusion
A bench-top simulation FUSE course delivered via a telementoring platform seems to improve surgical trainees’ knowledge and comfort in the safe use of electrosurgical devices as effectively as when it is delivered by a live proctor, despite long-term decay for both methods.


Similar content being viewed by others
References
Health devices: top 10 health technology hazards for 2011. ECRI Institute 2010. https://www.ecri.org/Products/Pages/Top-10-Hazards-Resources.aspx. Accessed 17 Jan 2017
Nduka CC, Super PA, Monson JR, Darzi AW (1994) Cause and prevention of electrosurgical injuries in laparoscopy. J Am Coll Surg 179(2):161–170
Lee J (2002) Update on electrosurgery. Outpatient Surg 2(2):44–53
Govekar HR, Robinson TN, Varosy PD et al (2012) Effect of monopolar radiofrequency energy on pacemaker function. Surg Endosc 26:2784–2788
Perantinides PG, Tsarouhas AP, Katzman VS (1998) The medicolegal risks of thermal injury during laparoscopic monopolar electrosurgery. J Healthc Risk Manag 18(1):47–55
Sankaranarayanan G, Resapu R, Jones DB, Schwaitzberg S, De S (2013) Common uses and cited complications of energy in surgery. Surg Endosc 27(9):3056–3072
Chandler JG, Voyles CR, Floore TL, Bartholomew LA (1997) Litigious consequences of open and laparoscopic biliary surgical mishaps. J Gastrointest Surg 1(2):138–145
Feldman LS, Fuchshuber P, Jones DB, Mischna J, Schwaitzberg SD, Force FT (2012) Surgeons don’t know what they don’t know about the safe use of energy in surgery. Surg Endosc 26:2735–2739
Madani A, Jones DB, Fuchshuber P, Robinson TN, Feldman LS (2014) Fundamental Use of Surgical Energy™ (FUSE): a curriculum on surgical energy-based devices. Surg Endosc 28(9):2509–2512
The SAGES Manual on the Fundamental Use of Surgical Energy (FUSE) (2012) Springer, New York.
Palter VN, Orzech N, Reznick RK, Grantcharov TP (2012) Validation of a structured training and assessment curriculum for technical skill acquisition in minimally invasive surgery: a randomized controlled trial. Ann Surg 257(2):224–230
Sroka G, Feldman LS, Vassiliou MC, Kaneva PA, Fayez R, Fried GM (2010) Fundamentals of laparoscopic surgery simulator training to proficiency improves laparoscopic performance in the operating room-a randomized controlled trial. Am J Surg 199(1):115–120
Madani A, Watanabe Y, Vassiliou MC et al (2014) Impact of a hands-on component on learning in the Fundamental Use of Surgical Energy™ (FUSE) curriculum: a randomized-controlled trial in surgical trainees. Surg Endosc 28(10):2772–2782
Madani A, Watanabe Y, Townsend N et al (2016) Structured simulation improves learning of the Fundamental Use of Surgical Energy™ curriculum: a multicenter randomized-controlled trial. Surg Endosc 30(2):684–691
Anastakis DJRG, Reznick RK, Cusimano M et al (1999) Assessment of technical skills transfer from the bench training model to the human model. Am J Surg 177:167–170
Scott DJBP, Rege RV, Laycock R et al (2000) Laparoscopic training on bench models: better and more cost effective than operating room experience? J Am Coll Surg Endosc 191:272–283
Anastakis DJ, Regehr G, Reznick RK et al (1999) Assessment of technical skills transfer from the bench training model to the human model. Am J Surg 177:167–170
Scott DJ, Bergen PC, Rege RV et al (2000) Laparoscopic training on bench models: better and more cost effective than operating room experience? J Am Coll Surg Endosc 191(3):272–283
Madani A, Watanabe Y, Townsend N et al (2015) Structured simulation improves learning of the Fundamental Use of Surgical EnergyTM curriculum: a multicenter randomized controlled trial. Surg Endosc 30(2):684–691
Bogen EM, Schlachta CM, Ponsky T (2019) White paper: technology for surgical telementoring-SAGES Project 6 Technology Working Group. Surg Endosc 33(3):684–690
Erridge S, Yeung DKT, Patel HRH, Purkayastha S (2019) Telementoring of surgeons: a systematic review. Surg Innov 26(1):95–111
Treter S, Perrier N, Sosa JA et al (2013) Telementoring: a multi-institutional experience with the introduction of a novel surgical approach for adrenalectomy. Ann Surg Oncol 20(8):2754–2758
Okrainec A, Soper NJ, Swanstrom LL et al (2011) Trends and results of the first 5 years of Fundamentals of Laparoscopic Surgery (FLS) certification testing. Surg Endosc 25(4):1192–1198
Anvari M (2007) Remote telepresence surgery: the Canadian experience. Surg Endosc 21(4):537–541
Schlachta CM, Sorsdahl AK, Lefebvre KL et al (2009) A model for longitudinal mentoring and telementoring of laparoscopic colon surgery. Surg Endosc 23(7):1634–1638
Forgione A, Kislov V, Guraya SY et al (2015) Safe introduction of laparoscopic colorectal surgery even in remote areas of the world: the value of a comprehensive telementoring training program. J Lap Adv Surg Tech 25(1):37–42
Bonrath EM, Dedy NJ, Gordon LE et al (2015) Comprehensive surgical coaching enhances surgical skill in the operating room: a randomized controlled trial. Ann Surg 262(2):205–212
Moore RGAJ, Partin AW, Docimo SG, Kavoussi LR (1996) Telementoring of laparoscopic procedures: initial clinical experience. Surg Endosc 10:107–110
Ponsky TASM, Parry J, Rothenberg S, Augestad KM (2014) Telementoring: the surgical tool of the future. Eur J Pediatr Surg 24:287–294
Acknowledgements
This study was sponsored by a grant provided by the Society of American Gastrointestinal and Endoscopic Surgeons grant in 2016 titled: “2016 - Educational Value of Telementoring for a Simulation-Based Fundamental Use of Surgical Energy™ (FUSE) Curriculum: A Randomized-Controlled Trial in Surgical Trainees”
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
Dr. Pryor is a speaker for Ethicon, Gore, Merck and Stryker, and a consultant for Medtronic. She has research support from Baronova and Obalon. Drs. Altieri, Madani, Carmichael, Robinson, and Jones have no conflicts of interest or financial ties to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Altieri, M.S., Carmichael, H., Jones, E. et al. Educational value of telementoring for a simulation-based fundamental use of surgical energy™ (FUSE) curriculum: a randomized controlled trial in surgical trainees. Surg Endosc 34, 3650–3655 (2020). https://doi.org/10.1007/s00464-020-07609-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-020-07609-1