Abstract
Introduction
Acute cholecystitis is a common disease and a frequent cause of emergency admission to surgical wards. Evidence regarding antibiotic administration in urgent procedures is limited and remains a contentious issue. According to the Tokyo guidelines, the antibiotic administration should be guided by the severity of cholecystitis, but internationally accepted guidelines are lacking. In particular, the need to perform antibiotic therapy after laparoscopic cholecystectomy is controversial for mild and moderate acute calculous cholecystitis (Tokio I and II).
Materials and methods
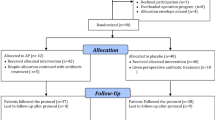
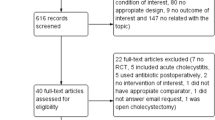
We performed a comprehensive computer literature search of PubMed and MEDLINE databases in accordance to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) Guidelines. We selected patients treated with cholecystectomy for mild or moderate acute calculous cholecystitis (Tokio I or II), only randomized controlled trials, (post-operative antibiotic administration versus placebo or untreated), data about local or systemic infection rate in the next 30 days after surgery.
Results
Three hundred and fifty-nine articles were identified, and three articles were considered eligible for the meta-analysis, including 676 patients. Overall surgical site infections were documented in 18 (5.49%) of 328 patients treated with post-operative antibiotics versus 25 (7.18%) of 348 patients treated without post-operative antibiotics. Overall results and the subgroup analysis (superficial and deep incisional infection and organ/space infection) showed no statistically significant reduction of surgical site infections rate under antibiotic therapy.
Conclusions
Our meta-analysis shows no significant benefit of extended antibiotic therapy in reducing SSI after cholecystectomy for mild and moderate acute cholecystitis (Tokio I and II). Further RCTs with adequate statistical power and involving a higher number of patients with subgroups are needed to better evaluate the benefit of post-operative antibiotic treatment in reducing the rate of organ/space surgical site infections.


Similar content being viewed by others
References
Schirmer BD, Winters KL, Edlich RF (2005) Cholelithiasis and cholecystitis. J Long Term Eff Med Implants 15(3):329–338
Jaafar G, Persson G, Svennblad B, Sandblom G (2014) Outcomes of antibiotic prophylaxis in acute cholecystectomy in a population-based gallstone surgery registry. Br J Surg 101(2):69–73
Pasquali S, Boal M, Griffiths EA, Alderson D, Vohra RS, CholeS Study Group (2016) West Midlands research collaborative. Meta-analysis of perioperative antibiotics in patients undergoing laparoscopic cholecystectomy. Br J Surg 103(1):27–34
Bratzler DW, Dellinger EP, Olsen KM, Perl TM, Auwaerter PG, Bolon MK, Fish DN, Napolitano LM, Sawyer RG, Slain D, Steinberg JP, Weinstein RA, American Society of Health-System Pharmacists; Infectious Disease Society of America; Surgical Infection Society; Society for Healthcare Epidemiology of America (2013) Clinical practice guidelines for antimicrobial prophylaxis in surgery. Am J Health Syst Pharm 70(3):195–283
Friedman GD (1993) Natural history of asymptomatic and symptomatic gallstones. Am J Surg 165:399–404
Yoshida M, Takada T, Kawarada Y, Tanaka A, Nimura Y, Gomi H, Hirota M, Miura F, Wada K, Mayumi T, Solomkin JS, Strasberg S, Pitt HA, Belghiti J, de Santibanes E, Fan ST, Chen MF, Belli G, Hilvano SC, Kim SW, Ker CG (2007) Antimicrobial therapy for acute cholecystitis: Tokyo guidelines. J Hepatobiliary Pancreat Surg 14(1):83–90
Yokoe M, Takada T, Strasberg SM, Solomkin JS, Mayumi T, Gomi H, Pitt HA, Gouma DJ, Garden OJ, Büchler MW, Kiriyama S, Kimura Y, Tsuyuguchi T, Itoi T, Yoshida M, Miura F, Yamashita Y, Okamoto K, Gabata T, Hata J, Higuchi R, Windsor JA, Bornman PC, Fan ST, Singh H, de Santibanes E, Kusachi S, Murata A, Chen XP, Jagannath P, Lee S, Padbury R, Chen MF, Tokyo Guidelines Revision Committee (2012) New diagnostic criteria and severity assessment of acute cholecystitis in revised Tokyo guidelines. J Hepatobiliary Pancreat Sci 19(5):578–585
Loozen CS, van Santvoort HC, van Geloven AAW, Nieuwenhuijzen GAP, de Reuver PR, Besselink MHG, Vlaminckx B, Kelder JC, Knibbe CAJ, Boerma D (2017) Perioperative antibiotic prophylaxis in the treatment of acute cholecystitis (PEANUTS II trial): study protocol for a randomized controlled trial. Trials 18(1):390
Coccolini F, Catena F, Pisano M, Gheza F, Fagiuoli S, Di Saverio S, Leandro G, Montori G, Ceresoli M, Corbella D, Sartelli M, Sugrue M, Ansaloni L (2015) Open versus laparoscopic cholecystectomy in acute cholecystitis. Systematic review and meta-analysis. Int J Surg 18:196–204
Yildiz B, Abbasoglu O, Tirnaksiz B, Hamaloglu E, Ozdemir A, Sayek I (2009) Determinants of postoperative infection after laparoscopic cholecystectomy. Hepatogastroenterology 56(91–92):589–592
Sözener U, Gedik E, Kessaf Aslar A, Ergun H, Halil Elhan A, Memikoğlu O, Bulent Erkek A, Ayhan Kuzu M (2011) Does adjuvant antibiotic treatment after drainage of anorectal abscess prevent development of anal fistulas? A randomized, placebo-controlled, double-blind, multicenter study. Dis Colon Rectum 54(8):923–929
Dindo D, Demartines N, Clavien PA (2004) Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg 240:205–213
Clark HD, Wells GA, Huët C, McAlister FA, Salmi LR, Fergusson D, Laupacis A (1999) Assessing the quality of randomized trials: reliability of the Jadad scale. Control Clin Trials 20(5):448–452
OCEBM Levels of Evidence Working Group. The Oxford levels of evidence 2. Oxford Centre for Evidence-Based Medicine. http://www.cebm.net/index.aspx?o=5653
DerSimonian R, Laird N (2015) Meta-analysis in clinical trials revisited. Contemp Clin Trials 45(Pt A):139–145
Higgins JP, Thompson SG (2002) Quantifying heterogeneity in a meta-analysis. Stat Med 21(11):1539–1558
StataCorp (2015) Stata statistical software: release 14.2. StataCorp LP, College Station
Regimbeau JM, Fuks D, Pautrat K, Mauvais F, Haccart V, Msika S, Mathonnet M, Scotté M, Paquet JC, Vons C, Sielezneff I, Millat B, Chiche L, Dupont H, Duhaut P, Cossé C, Diouf M, Pocard M, FRENCH Study Group (2014) Effect of postoperative antibiotic administration on postoperative infection following cholecystectomy for acute calculous cholecystitis: a randomized clinical trial. JAMA 312(2):145–154
Loozen CS, Kortram K, Kornmann VN, van Ramshorst B, Vlaminckx B, Knibbe CA, Kelder JC, Donkervoort SC, Nieuwenhuijzen GA, Ponten JE, van Geloven AA, van Duijvendijk P, Bos WJ, Besselink MG, Gouma DJ, van Santvoort HC, Boerma D (2017) Randomized clinical trial of extended versus single-dose perioperative antibiotic prophylaxis for acute calculous cholecystitis. Br J Surg 104(2):e151–e157
Kim EY, Yoon YC, Choi HJ, Kim KH, Park JH, Hong TH (2017) Is there a real role of postoperative antibiotic administration for mildmoderate acute cholecystitis? A prospective randomized controlled trial. J Hepatobiliary Pancreat Sci 24:550–558
Berríos-Torres SI, Umscheid CA, Bratzler DW, Leas B, Stone EC, Kelz RR, Reinke CE, Morgan S, Solomkin JS, Mazuski JE, Dellinger EP, Itani KMF, Berbari EF, Segreti J, Parvizi J, Blanchard J, Allen G, Kluytmans JAJW, Donlan R, Schecter WP, Healthcare Infection Control Practices Advisory Committee (2017) Centers for disease control and prevention guideline for the prevention of surgical site infection, 2017 JAMA Surg 152(8):784–791
Llor C, Bjerrum L (2014) Antimicrobial resistance: risk associated with antibiotic overuse and initiatives to reduce the problem. Ther Adv Drug Saf 5(6):229–241
van Dijk AH, de Reuver PR, Tasma TN, van Dieren S, Hugh TJ, Boermeester MA (2016) Systematic review of antibiotic treatment for acute calculous cholecystitis. Br J Surg 103(7):797–811
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
Drs. Davide La Regina, Matteo Di Giuseppe, Stefano Cafarotti, Andrea Saporito, Marcello Ceppi, Francesco Mongelli, Florian Bihl, Ruben Carlo Balzarotti Canger and Antonjacopo Ferrario di Tor Vajana have no conflicts of interest or financial ties to disclose.
Rights and permissions
About this article
Cite this article
La Regina, D., Di Giuseppe, M., Cafarotti, S. et al. Antibiotic administration after cholecystectomy for acute mild-moderate cholecystitis: a PRISMA-compliant meta-analysis. Surg Endosc 33, 377–383 (2019). https://doi.org/10.1007/s00464-018-6498-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-018-6498-0