Abstract
Purpose
After the COVID-19 pandemic, many challenges arose regarding the impact of this disease on people with ulcerative colitis. The aims of this study were to estimate the prevalence, severity, and death consequences of COVID-19 in patients with ulcerative colitis using a systematic review and meta-analysis.
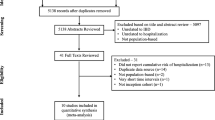
Methods
This study was conducted using a systematic review and meta-analysis method in the field of prevalence, severity, and clinical consequences of COVID-19 in people with ulcerative colitis worldwide. The search was conducted in international scientific databases, such as Web of Science, PubMed, Scopus, Cochrane Library, and Google Scholar, from the beginning of 2020 to October 2023. The quality of the eligible studies was assessed using the Strobe and Newcastle Ottawa checklists. The data were analyzed using a fixed-effects model in the meta-analysis. Subgroup analysis and meta-regression were performed using STATA version 17.
Results
Nineteen studies with a sample size of 224,520 patients were included in this meta-analysis. The results showed that, in COVID-19 patients with ulcerative colitis, the prevalence of hospitalization, death, COVID-19 severity, and mortality rate in severe patients was 54% (95% CI, 27–80%), 10% (95% CI, 4–16%), 20% (95% CI, 8–34%), 63% (95% CI, 46–80%), respectively. In comparison with the general population, the odds ratio (OR) of hospitalization in patients due to COVID-19 was OR = 1.28 (95% CI, 1.19–1.38, P < 0.001), and the chance of severe COVID-19 was OR = 1.30 (95% CI, 1.22–1.53, P < 0.001).
Conclusion
The probability of contracting the severe type of COVID-19 and hospitalization in patients with ulcerative colitis was higher than in the general population.









Similar content being viewed by others
Data availability
The data that support the findings of this study are available on request from the corresponding author, (Xueliang Jiang).
References
Silverberg MS, Satsangi J, Ahmad T, Arnott ID, Bernstein CN, Brant SR et al (2005) Toward an integrated clinical, molecular and serological classification of inflammatory bowel disease: report of a Working Party of the 2005 Montreal World Congress of Gastroenterology. Can J Gastroenterol 19(Suppl A):5A–36A
Halling ML, Kjeldsen J, Knudsen T, Nielsen J, Hansen LK (2017) Patients with inflammatory bowel disease have increased risk of autoimmune and inflammatory diseases. World J Gastroenterol 23(33):6137
Das KM, Biancone L (2008) Is IBD an autoimmune disorder? Inflamm Bowel Dis 14(suppl_2):S97–S101
MacDonald TT, Monteleone G (2005) Immunity, inflammation, and allergy in the gut. Science 307(5717):1920–1925
Du L, Ha C (2020) Epidemiology and pathogenesis of ulcerative colitis. Gastroenterol Clin 49(4):643–654
Gajendran M, Loganathan P, Jimenez G, Catinella AP, Ng N, Umapathy C et al (2019) A comprehensive review and update on ulcerative colitis. Dis Mon 65(12):100851
Shivashankar R, Tremaine WJ, Harmsen WS, Loftus EV Jr (2017) Incidence and prevalence of Crohn’s disease and ulcerative colitis in Olmsted County, Minnesota from 1970 through 2010. Clin Gastroenterol Hepatol 15(6):857–863
Samuel S, Ingle SB, Dhillon S, Yadav S, Harmsen WS, Zinsmeister AR et al (2013) Cumulative incidence and risk factors for hospitalization and surgery in a population-based cohort of ulcerative colitis. Inflamm Bowel Dis 19(9):1858–1866
Kappelman MD, Moore KR, Allen JK, Cook SF (2013) Recent trends in the prevalence of Crohn’s disease and ulcerative colitis in a commercially insured US population. Dig Dis Sci 58:519–525
Subasinghe D, Nawarathna N, Samarasekera DN (2011) Disease characteristics of inflammatory bowel disease (IBD) findings from a tertiary care centre in South Asia. J Gastrointest Surg 15:1562–1567
Carr I, Mayberry JF (1999) The effects of migration on ulcerative colitis: a three-year prospective study among Europeans and first-and second-generation South Asians in Leicester (1991–1994). Am J Gastroenterol 94(10):2918–2922
Higuchi LM, Khalili H, Chan AT, Richter JM, Bousvaros A, Fuchs CS (2012) A prospective study of cigarette smoking and the risk of inflammatory bowel disease in women. Am J Gastroenterol 107(9):1399
Zhu N, Zhang D, Wang W, Li X, Yang B, Song J et al (2020) A novel coronavirus from patients with pneumonia in China, 2019. N Engl J Med
Dulai PS, Thompson KD, Blunt HB, Dubinsky MC, Siegel CA (2014) Risks of serious infection or lymphoma with anti–tumor necrosis factor therapy for pediatric inflammatory bowel disease: a systematic review. Clin Gastroenterol Hepatol 12(9):1443–1451
Hoffmann M, Kleine-Weber H, Schroeder S, Krüger N, Herrler T, Erichsen S et al (2020) SARS-CoV-2 cell entry depends on ACE2 and TMPRSS2 and is blocked by a clinically proven protease inhibitor. Cell 181(2):271–80. e8
Harmer D, Gilbert M, Borman R, Clark KL (2002) Quantitative mRNA expression profiling of ACE 2, a novel homologue of angiotensin converting enzyme. FEBS Lett 532(1–2):107–110
Garg M, Royce SG, Tikellis C, Shallue C, Batu D, Velkoska E et al (2020) Imbalance of the renin–angiotensin system may contribute to inflammation and fibrosis in IBD: a novel therapeutic target? Gut 69(5):841–851
Ning L, Shan G, Sun Z, Zhang F, Xu C, Lou X et al (2019) Quantitative proteomic analysis reveals the deregulation of nicotinamide adenine dinucleotide metabolism and CD38 in inflammatory bowel disease. BioMed Res Int 2019
Jablaoui A, Kriaa A, Mkaouar H, Akermi N, Soussou S, Wysocka M et al (2020) Fecal serine protease profiling in inflammatory bowel diseases. Front Cell Infect Microbiol 10:21
Bezzio C, Saibeni S, Variola A, Allocca M, Massari A, Gerardi V et al (2020) Outcomes of COVID-19 in 79 patients with IBD in Italy: an IG-IBD study. Gut 69(7):1213–1217
Maconi G, Bosetti C, De Monti A, Boyapati RK, Shelton E, Piazza N et al (2021) Risk of COVID-19 in patients with inflammatory bowel diseases compared to a control population. Dig Liver Dis 53(3):263–270
Moher D, Shamseer L, Clarke M, Ghersi D, Liberati A, Petticrew M et al (2015) Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015 statement. Syst Rev 4(1):1
Von Elm E, Altman DG, Egger M, Pocock SJ, Gøtzsche PC, Vandenbroucke JP et al (2014) The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) Statement: guidelines for reporting observational studies. Int J Surg 12(12):1495–1499
Freeman MF, Tukey JW (1950) Transformations related to the angular and the square root. Ann Math Statist pp. 607–611
Stang A (2010) Critical evaluation of the Newcastle-Ottawa scale for the assessment of the quality of nonrandomized studies in meta-analyses. Eur J Epidemiol 25(9):603–605
Sterne JA, Gavaghan D, Egger M (2000) Publication and related bias in meta-analysis: the power of statistical tests and prevalence in the literature. J Clin Epidemiol 53(11):1119–1129
Duval S, Tweedie R (2000) A nonparametric “trim and fill” method of accounting for publication bias in meta-analysis. J Am Stat Assoc 95(449):89–98
Queiroz NS, Martins CdA, Quaresma AB, Hino AA, Steinwurz F, Ungaro RC et al (2021) COVID‐19 outcomes in patients with inflammatory bowel diseases in Latin America: results from SECURE‐IBD registry. J Gastroenterol Hepat 36(11):3033–40
Xu F, Carlson SA, Wheaton AG, Greenlund KJ (2021) COVID-19 hospitalizations among US Medicare beneficiaries with inflammatory bowel disease, April 1 to July 31, 2020. Inflamm Bowel Dis 27(7):1166–1169
Allocca M, Fiorino G, Zallot C, Furfaro F, Gilardi D, Radice S et al (2020) Incidence and patterns of COVID-19 among inflammatory bowel disease patients from the Nancy and Milan cohorts. Clin Gastroenterol Hepatol 18(9):2134–2135
Attauabi M, Poulsen A, Theede K, Pedersen N, Larsen L, Jess T et al (2021) Prevalence and outcomes of COVID-19 among patients with inflammatory bowel disease—a Danish prospective population-based cohort study. J Crohns Colitis 15(4):540–550
Ludvigsson JF, Axelrad J, Halfvarson J, Khalili H, Larsson E, Lochhead P et al (2021) Inflammatory bowel disease and risk of severe COVID-19: a nationwide population-based cohort study in Sweden. United Eur Gastroenterol J 9(2):177–192
Taxonera C, Sagastagoitia I, Alba C, Manas N, Olivares D, Rey E (2020) 2019 Novel coronavirus disease (COVID‐19) in patients with inflammatory bowel diseases. Aliment Pharmacol Ther 52(2):276–83
Ardizzone S, Ferretti F, Monico MC, Carvalhas Gabrielli AM, Carmagnola S, Bezzio C et al (2021) Lower incidence of COVID-19 in patients with inflammatory bowel disease treated with non-gut selective biologic therapy. J Gastroenterol Hepatol 36(11):3050–3055
Derikx LA, Lantinga MA, De Jong DJ, Van Dop WA, Creemers RH, Römkens TE et al (2021) Clinical outcomes of Covid-19 in patients with inflammatory bowel disease: a nationwide cohort study. J Crohns Colitis 15(4):529–539
Tripathi K, Godoy Brewer G, Thu Nguyen M, Singh Y, Saleh Ismail M, Sauk JS et al (2022) COVID-19 and outcomes in patients with inflammatory bowel disease: systematic review and meta-analysis. Inflamm Bowel Dis 28(8):1265–1279
Abdulla M, Mohammed N, AlQamish J, Mosli M (2022) Inflammatory bowel disease and COVID-19 outcomes: a meta-analysis. Sci Rep 12(1):21333
Singh AK, Jena A, Kumar-M P, Sharma V, Sebastian S (2021) Risk and outcomes of coronavirus disease in patients with inflammatory bowel disease: a systematic review and meta-analysis. United Eur Gastroenterol J 9(2):159–176
Hu Y, Sun J, Dai Z, Deng H, Li X, Huang Q et al (2020) Prevalence and severity of corona virus disease 2019 (COVID-19): A systematic review and meta-analysis. J Clin Virol 127:104371
Morin L, Savale L, Pham T, Colle R, Figueiredo S, Harrois A et al (2021) Four-month clinical status of a cohort of patients after hospitalization for COVID-19. JAMA 325(15):1525–1534
Kim L, Whitaker M, O’Halloran A, Kambhampati A, Chai SJ, Reingold A et al (2020) Hospitalization rates and characteristics of children aged< 18 years hospitalized with laboratory-confirmed COVID-19—COVID-NET, 14 states, March 1–July 25, 2020. Morb Mortal Wkly Rep 69(32):1081
Nowak JK, Lindstrøm JC, Kalla R, Ricanek P, Halfvarson J, Satsangi J (2020) Age, inflammation, and disease location are critical determinants of intestinal expression of SARS-CoV-2 receptor ACE2 and TMPRSS2 in inflammatory bowel disease. Gastroenterology 159(3):1151–4.e2
Burgueño JF, Reich A, Hazime H, Quintero MA, Fernandez I, Fritsch J et al (2020) Expression of SARS-CoV-2 entry molecules ACE2 and TMPRSS2 in the gut of patients with IBD. Inflamm Bowel Dis 26(6):797–808
Alulis S, Vadstrup K, Borsi A, Nielsen A, Rikke Jørgensen T, Qvist N et al (2020) Treatment patterns for biologics in ulcerative colitis and Crohn’s disease: a Danish Nationwide Register Study from 2003 to 2015. Scand J Gastroenterol 55(3):265–271
Fletcher J (2007) What is heterogeneity and is it important? BMJ 334:94
Acknowledgements
We thank all researchers of the article that we used their data.
Author information
Authors and Affiliations
Contributions
JK, JY, XJ, and LW designed the conception of the study; original draft preparation, review, and editing; JK and JY, did search and data extraction; XJ and LW did validation and quality assessment, and statistical analysis. All the authors approved the final manuscript and the authorship.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Yang, J., Ke, J., Jiang, X. et al. The association between ulcerative colitis and COVID-19 severity: a systematic review and meta-analysis systematic review. Int J Colorectal Dis 39, 5 (2024). https://doi.org/10.1007/s00384-023-04568-6
Accepted:
Published:
DOI: https://doi.org/10.1007/s00384-023-04568-6