Abstract
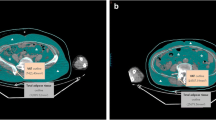
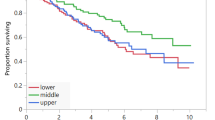
This study aimed to clarify the clinical and prognostic role of body composition and metabolic parameters extracted from baseline 18F-FDG PET/CT in patients with diffuse large B-cell lymphoma (DLBCL). We retrospectively collected the clinicopathological and 18F-FDG PET/CT parameters of 181 DLBCL patients. The indexes of skeletal muscle, subcutaneous adipose tissue, and visceral adipose tissue were calculated using the area measured at the 3rd lumbar level normalized for height. Additionally, the metabolic activity of corresponding muscle and adipose tissue, and maximum standardized uptake value (SUVmax), metabolic tumor volume (MTV), and total lesion glycolysis (TLG) of all lesions were measured. Survival endpoints included progression-free survival (PFS) and overall survival (OS). We identified 75 (41.4%) patients with low skeletal muscle index (sarcopenia), presenting risk factors including male, high β2-microglobulin, low BMI, high visceral adipose tissue index, low SUVmax of skeletal muscle, and high SUVmax of visceral adipose tissue. Male, low BMI, low visceral adipose tissue index, and high SUVmax of subcutaneous adipose tissue were risk factors for low subcutaneous adipose tissue index diagnosed in 105 (58.0%) patients. In total, 132 (79.2%) patients represented low visceral adipose tissue index, associated with younger age, B symptoms, and low BMI. Eastern Cooperative Oncology Group (ECOG) status, sarcopenia, and visceral adipose tissue index were found independently predictive of PFS and OS, while β2-microglobulin was independently predictive of OS. In conclusion, body composition indexes were correlated with both clinical characteristics and 18F-FDG PET/CT metabolic parameters, significantly impacting survival, such that sarcopenia and high visceral adipose tissue index were powerful predictors of poor DLBCL outcomes.



Similar content being viewed by others
Data availability
Data are available based on the reasonable request to the corresponding author.
References
Sung H, Ferlay J, Siegel RL, Laversanne M, Soerjomataram I, Jemal A et al (2021) Global Cancer Statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin 71:209–249. https://doi.org/10.3322/caac.21660
Sehn LH, Salles G (2021) Diffuse large B-cell lymphoma. N Engl J Med 384:842–858. https://doi.org/10.1056/NEJMra2027612
Ruppert AS, Dixon JG, Salles G, Wall A, Cunningham D, Poeschel V et al (2020) International prognostic indices in diffuse large B-cell lymphoma: a comparison of IPI, R-IPI, and NCCN-IPI. Blood 135:2041–2048. https://doi.org/10.1182/blood.2019002729
Chen LK, Liu LK, Woo J, Assantachai P, Auyeung TW, Bahyah KS et al (2014) Sarcopenia in Asia: consensus report of the Asian Working Group for Sarcopenia. J Am Med Dir Assoc 15:95–101. https://doi.org/10.1016/j.jamda.2013.11.025
Meza-Valderrama D, Marco E, Dávalos-Yerovi V, Muns MD, Tejero-Sánchez M, Duarte E et al (2021) Sarcopenia, malnutrition, and cachexia: adapting definitions and terminology of nutritional disorders in older people with cancer. Nutrients 13. https://doi.org/10.3390/nu13030761
Cruz-Jentoft AJ, Bahat G, Bauer J, Boirie Y, Bruyère O, Cederholm T et al (2019) Sarcopenia: revised European consensus on definition and diagnosis. Age Ageing 48:16–31. https://doi.org/10.1093/ageing/afy169
Fang P, Zhou J, Xiao X, Yang Y, Luan S, Liang Z et al (2023) The prognostic value of sarcopenia in oesophageal cancer: a systematic review and meta-analysis. J Cachexia Sarcopenia Muscle 14:3–16. https://doi.org/10.1002/jcsm.13126
Yang M, Shen Y, Tan L, Li W (2019) Prognostic value of sarcopenia in lung cancer: a systematic review and meta-analysis. Chest 156:101–111. https://doi.org/10.1016/j.chest.2019.04.115
Zilioli VR, Albano D, Arcari A, Merli F, Coppola A, Besutti G et al (2021) Clinical and prognostic role of sarcopenia in elderly patients with classical Hodgkin lymphoma: a multicentre experience. J Cachexia Sarcopenia Muscle 12:1042–1055. https://doi.org/10.1002/jcsm.12736
Shin DY, Kim A, Byun BH, Moon H, Kim S, Ko YJ et al (2016) Visceral adipose tissue is prognostic for survival of diffuse large B cell lymphoma treated with frontline R-CHOP. Ann Hematol 95:409–416. https://doi.org/10.1007/s00277-015-2571-0
Besutti G, Massaro F, Bonelli E, Braglia L, Casali M, Versari A et al (2021) Prognostic impact of muscle quantity and quality and fat distribution in diffuse large B-cell lymphoma patients. Front Nutr 8:620696. https://doi.org/10.3389/fnut.2021.620696
Zelenetz AD, Gordon LI, Chang JE, Christian B, Abramson JS, Advani RH, et al. NCCN Guidelines® insights: B-cell lymphomas, Version 5.2021. J Natl Compr Canc Netw. 2021;19:1218–30. https://doi.org/10.6004/jnccn.2021.0054
Barrington SF, Mikhaeel NG, Kostakoglu L, Meignan M, Hutchings M, Müeller SP et al (2014) Role of imaging in the staging and response assessment of lymphoma: consensus of the International Conference on Malignant Lymphomas Imaging Working Group. J Clin Oncol 32:3048–58. https://doi.org/10.1200/jco.2013.53.5229
Ceriani L, Martelli M, Zinzani PL, Ferreri AJ, Botto B, Stelitano C et al (2015) Utility of baseline 18FDG-PET/CT functional parameters in defining prognosis of primary mediastinal (thymic) large B-cell lymphoma. Blood 126:950–956. https://doi.org/10.1182/blood-2014-12-616474
Sasanelli M, Meignan M, Haioun C, Berriolo-Riedinger A, Casasnovas RO, Biggi A et al (2014) Pretherapy metabolic tumour volume is an independent predictor of outcome in patients with diffuse large B-cell lymphoma. Eur J Nucl Med Mol Imaging 41:2017–2022. https://doi.org/10.1007/s00259-014-2822-7
Zeng X, Shi ZW, Yu JJ, Wang LF, Luo YY, Jin SM et al (2021) Sarcopenia as a prognostic predictor of liver cirrhosis: a multicentre study in China. J Cachexia Sarcopenia Muscle 12:1948–1958. https://doi.org/10.1002/jcsm.12797
Xu XT, He DL, Tian MX, Wu HJ, Jin X (2022) Prognostic value of sarcopenia in patients with diffuse large B-cell lymphoma treated with R-CHOP: a systematic review and meta-analysis. Front Nutr 9:816883. https://doi.org/10.3389/fnut.2022.816883
Nakamura N, Hara T, Shibata Y, Matsumoto T, Nakamura H, Ninomiya S et al (2015) Sarcopenia is an independent prognostic factor in male patients with diffuse large B-cell lymphoma. Ann Hematol 94:2043–2053. https://doi.org/10.1007/s00277-015-2499-4
Lanic H, Kraut-Tauzia J, Modzelewski R, Clatot F, Mareschal S, Picquenot JM et al (2014) Sarcopenia is an independent prognostic factor in elderly patients with diffuse large B-cell lymphoma treated with immunochemotherapy. Leuk Lymphoma 55:817–823. https://doi.org/10.3109/10428194.2013.816421
Yuan H, Tan X, Sun X, He L, Li D, Jiang L (2023) Role of (18)F-FDG PET/CT and sarcopenia in untreated non-small cell lung cancer with advanced stage. Jpn J Radiol 41:521–530. https://doi.org/10.1007/s11604-022-01369-9
Kim JK, Choi SR, Choi MJ, Kim SG, Lee YK, Noh JW et al (2014) Prevalence of and factors associated with sarcopenia in elderly patients with end-stage renal disease. Clin Nutr 33:64–68. https://doi.org/10.1016/j.clnu.2013.04.002
Choi H, Park YS, Na KJ, Park S, Park IK, Kang CH et al (2021) Association of adipopenia at preoperative PET/CT with mortality in stage I non-small cell lung cancer. Radiology 301:645–653. https://doi.org/10.1148/radiol.2021210576
Ebadi M, Tandon P, Moctezuma-Velazquez C, Ghosh S, Baracos VE, Mazurak VC et al (2018) Low subcutaneous adiposity associates with higher mortality in female patients with cirrhosis. J Hepatol 69:608–616. https://doi.org/10.1016/j.jhep.2018.04.015
Fujiwara N, Nakagawa H, Kudo Y, Tateishi R, Taguri M, Watadani T et al (2015) Sarcopenia, intramuscular fat deposition, and visceral adiposity independently predict the outcomes of hepatocellular carcinoma. J Hepatol 63:131–140. https://doi.org/10.1016/j.jhep.2015.02.031
Ebadi M, Martin L, Ghosh S, Field CJ, Lehner R, Baracos VE et al (2017) Subcutaneous adiposity is an independent predictor of mortality in cancer patients. Br J Cancer 117:148–155. https://doi.org/10.1038/bjc.2017.149
Iliodromiti S, Celis-Morales CA, Lyall DM, Anderson J, Gray SR, Mackay DF et al (2018) The impact of confounding on the associations of different adiposity measures with the incidence of cardiovascular disease: a cohort study of 296 535 adults of white European descent. Eur Heart J 39:1514–1520. https://doi.org/10.1093/eurheartj/ehy057
Zeng Q, Wang L, Dong S, Zha X, Ran L, Li Y et al (2021) CT-derived abdominal adiposity: distributions and better predictive ability than BMI in a nationwide study of 59,429 adults in China. Metabolism 115:154456. https://doi.org/10.1016/j.metabol.2020.154456
Neeland IJ, Ross R, Després JP, Matsuzawa Y, Yamashita S, Shai I et al (2019) Visceral and ectopic fat, atherosclerosis, and cardiometabolic disease: a position statement. Lancet Diabetes Endocrinol 7:715–725. https://doi.org/10.1016/s2213-8587(19)30084-1
Reijrink M, de Boer SA, Antunes IF, Spoor DS, Heerspink HJL, Lodewijk ME et al (2021) [(18)F]FDG uptake in adipose tissue is not related to inflammation in type 2 diabetes mellitus. Mol Imaging Biol 23:117–126. https://doi.org/10.1007/s11307-020-01538-0
Van de Wiele C, Van Vlaenderen M, D’Hulst L, Delcourt A, Copin D, De Spiegeleer B et al (2017) Metabolic and morphological measurements of subcutaneous and visceral fat and their relationship with disease stage and overall survival in newly diagnosed pancreatic adenocarcinoma : metabolic and morphological fat measurements in pancreatic adenocarcinoma. Eur J Nucl Med Mol Imaging 44:110–116. https://doi.org/10.1007/s00259-016-3525-z
Okumura S, Kaido T, Hamaguchi Y, Kobayashi A, Shirai H, Yao S et al (2017) Visceral adiposity and sarcopenic visceral obesity are associated with poor prognosis after resection of pancreatic cancer. Ann Surg Oncol 24:3732–3740. https://doi.org/10.1245/s10434-017-6077-y
Camus V, Lanic H, Kraut J, Modzelewski R, Clatot F, Picquenot JM et al (2014) Prognostic impact of fat tissue loss and cachexia assessed by computed tomography scan in elderly patients with diffuse large B-cell lymphoma treated with immunochemotherapy. Eur J Haematol 93:9–18. https://doi.org/10.1111/ejh.12285
Crudele L, Piccinin E, Moschetta A (2021) Visceral adiposity and cancer: role in pathogenesis and prognosis. Nutrients 13. https://doi.org/10.3390/nu13062101
Doyle SL, Donohoe CL, Lysaght J, Reynolds JV (2012) Visceral obesity, metabolic syndrome, insulin resistance and cancer. Proc Nutr Soc 71:181–189. https://doi.org/10.1017/s002966511100320x
Lutz CT, Quinn LS (2012) Sarcopenia, obesity, and natural killer cell immune senescence in aging: altered cytokine levels as a common mechanism. Aging (Albany NY). 4:535–46. https://doi.org/10.18632/aging.100482
Neeman E, Gresham G, Ovasapians N, Hendifar A, Tuli R, Figlin R et al (2019) Comparing physician and nurse Eastern Cooperative Oncology Group Performance Status (ECOG-PS) ratings as predictors of clinical outcomes in patients with cancer. Oncologist 24:e1460–e1466. https://doi.org/10.1634/theoncologist.2018-0882
Chen Y, Neelapu S, Feng L, Bi W, Yang TH, Wang M et al (2016) Prognostic significance of baseline peripheral absolute neutrophil, monocyte and serum β2-microglobulin level in patients with diffuse large b-cell lymphoma: a new prognostic model. Br J Haematol 175:290–299. https://doi.org/10.1111/bjh.14237
Chen H, Zhong Q, Zhou Y, Qin Y, Yang J, Liu P et al (2022) Enhancement of the International prognostic index with β2-microglobulin, platelet count and red blood cell distribution width: a new prognostic model for diffuse large B-cell lymphoma in the rituximab era. BMC Cancer 22:583. https://doi.org/10.1186/s12885-022-09693-z
Funding
This work was supported by the fund from the National Natural Science Foundation of China (81971645), Guangdong Provincial People’s Hospital (KY0120211130), and Guangdong Provincial Key Laboratory of Artificial Intelligence in Medical Image Analysis and Application (2022B1212010011).
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Ethics approval
All procedures performed in studies involving human participants were approved by the ethics committee at Guangdong Provincial People’s Hospital, and with the principles of the 1964 Declaration of Helsinki and its later amendments.
Informed consent
Informed consent was waived due to the retrospective nature of this study.
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Chen, Y., Chen, Z., Tan, X. et al. Role of body composition and metabolic parameters extracted from baseline 18F-FDG PET/CT in patients with diffuse large B-cell lymphoma. Ann Hematol 102, 2779–2789 (2023). https://doi.org/10.1007/s00277-023-05379-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00277-023-05379-z