Abstract
Background
Stem cell therapy is a promising new approach to wound healing. Stromal vascular fraction is a heterogeneous collection of cells, including adipose-derived stem cells, which are traditionally isolated using a manual collagenase-based technique. To our knowledge, this is the first human study that histologically assesses the potential of intraoperative intradermal injection of stromal vascular fraction on skin regeneration.
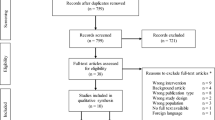
Methods
In this controlled study, 20 patients undergoing deep inferior epigastric perforator flap breast reconstruction and bilateral flank liposuction were included. Stromal vascular fraction was injected intradermally into one side of the abdominal suture line, while the other side served as a control. Outcome measures included analysis of stromal vascular fraction by flow cytometry, histological analysis of scar tissue, and scar photography.
Results
Cell yield for application and cell viability were 55.9 ± 28.5 × 106 and 75.1% ± 14.5%, respectively. Age and body mass index were positively correlated with the number of cells for application and adipose-derived stem cells. Mean vascular density, elastic fiber content, collagen maturity (scar index), epidermal thickness, and number of rete ridges all showed higher values on the treated side. Furthermore, the injected number of adipose-derived stem cells and pericytes positively correlated with vascular density.
Conclusions
It is safe to speculate that intradermal stromal vascular fraction injection at the beginning of the healing process increases vascular density, collagen maturity and organization, elastic fiber content, epidermal thickness, epidermal–dermal anchoring of the scarring skin and is therefore responsible for improved skin regeneration. It is a viable and safe method that can be used as an adjunctive treatment in plastic surgery procedures where suboptimal wound healing is anticipated.
Level of Evidence IV
This journal requires that authors assign a level of evidence to each article. For a full description of these Evidence-Based Medicine ratings, please refer to the Table of Contents or the online Instructions to Authors www.springer.com/00266.










Similar content being viewed by others
References
Brown BC, McKenna SP, Siddhi K, McGrouther DA, Bayat A (2008) The hidden cost of skin scars: quality of life after skin scarring. J Plast Reconstr Aesthet Surg 61(9):1049–1058
Sen CK, Gordillo GM, Roy S et al (2009) Human skin wounds: a major and snowballing threat to public health and the economy. Wound Repair Regen. 17(6):763–771
Kishi K, Okabe K, Shimizu R, Kubota Y (2012) Fetal skin possesses the ability to regenerate completely: complete regeneration of skin. Keio J Med 61(4):101–108
Larson BJ, Longaker MT, Lorenz HP (2010) Scarless fetal wound healing: a basic science review. Plast Reconstr Surg 126(4):1172–1180
Hu MS, Maan ZN, Wu JC et al (2014) Tissue engineering and regenerative repair in wound healing. Ann Biomed Eng 42(7):1494–1507
Moore AL, Marshall CD, Barnes LA, Murphy MP, Ransom RC, Longaker MT (2018) Scarless wound healing: transitioning from fetal research to regenerative healing. Wiley Interdiscip Rev Dev Biol. 7(2):e309
Hu MS, Rennert RC, McArdle A et al (2014) The role of stem cells during scarless skin wound healing. Adv Wound Care (New Rochelle). 3(4):304–314
Leung A, Crombleholme TM, Keswani SG (2012) Fetal wound healing: implications for minimal scar formation. Curr Opin Pediatr 24(3):371–378
Guo J, Nguyen A, Banyard DA et al (2016) Stromal vascular fraction: a regenerative reality? Part 2: mechanisms of regenerative action. J Plast Reconstr Aesthet Surg 69(2):180–188
Hu MS, Borrelli MR, Lorenz HP, Longaker MT, Wan DC (2018) Mesenchymal stromal cells and cutaneous wound healing: a comprehensive review of the background, role, and therapeutic potential. Stem Cells Int. 2018:6901983
Nguyen A, Guo J, Banyard DA et al (2016) Stromal vascular fraction: a regenerative reality? Part 1: current concepts and review of the literature. J Plast Reconstr Aesthet Surg 69(2):170–179
Spiekman M, van Dongen JA, Willemsen JC, Hoppe DL, van der Lei B, Harmsen MC (2017) The power of fat and its adipose-derived stromal cells: emerging concepts for fibrotic scar treatment. J Tissue Eng Regen Med 11(11):3220–3235
Gentile P, Orlandi A, Scioli MG, Di Pasquali C, Bocchini I, Cervelli V (2012) Concise review: adipose-derived stromal vascular fraction cells and platelet-rich plasma: basic and clinical implications for tissue engineering therapies in regenerative surgery. Stem Cells Transl Med 1(3):230–236
Rohrich RJ, Wan D (2019) Making sense of stem cells and fat grafting in plastic surgery: the hype, evidence, and evolving U.S. food and drug administration regulations. Plast Reconstr Surg 143(2):417e–424e
Zimmerlin L, Donnenberg VS, Pfeifer ME et al (2010) Stromal vascular progenitors in adult human adipose tissue. Cytometry A 77(1):22–30
Andia I, Maffulli N, Burgos-Alonso N (2019) Stromal vascular fraction technologies and clinical applications. Expert Opin Biol Ther 19(12):1289–1305
Blaber SP, Webster RA, Hill CJ et al (2012) Analysis of in vitro secretion profiles from adipose-derived cell populations. J Transl Med 10:172
Aronowitz JA, Ellenhorn JD (2013) Adipose stromal vascular fraction isolation: a head-to-head comparison of four commercial cell separation systems. Plast Reconstr Surg 132(6):932e–939e
Aronowitz JA, Lockhart RA, Hakakian CS (2015) Mechanical versus enzymatic isolation of stromal vascular fraction cells from adipose tissue. Springerplus 4:713
Bourin P, Bunnell BA, Casteilla L et al (2013) Stromal cells from the adipose tissue-derived stromal vascular fraction and culture expanded adipose tissue-derived stromal/stem cells: a joint statement of the international federation for adipose therapeutics and science (IFATS) and the international society for cellular therapy (ISCT). Cytotherapy 15(6):641–648
Junqueira LCU, Bignolas G, Brentani RR (1979) Picrosirius staining plus polarization microscopy, a specific method for collagen detection in tissue sections. Histochem J 11(4):447–455
Flanders KC, Major CD, Arabshahi A et al (2003) Interference with transforming growth factor-β/ Smad3 signaling results in accelerated healing of wounds in previously irradiated skin. Am J Pathol 163(6):2247–2257
Sultan SM, Stern CS, Allen RJ Jr et al (2011) Human fat grafting alleviates radiation skin damage in a murine model. Plast Reconstr Surg 128(2):363–372
Koh YJ, Koh BI, Kim H et al (2011) Stromal vascular fraction from adipose tissue forms profound vascular network through the dynamic reassembly of blood endothelial cells. Arterioscler Thromb Vasc Biol 31(5):1141–1150
Kwon HM, Hur SM, Park KY et al (2014) Multiple paracrine factors secreted by mesenchymal stem cells contribute to angiogenesis. Vascul Pharmacol 63(1):19–28
Rigotti G, Marchi A, Galie M et al (2007) Clinical treatment of radiotherapy tissue damage by lipoaspirate transplant: a healing process mediated by adipose-derived adult stem cells. Plast Reconstr Surg. 119(5):1409–1422 (discussion 1423-1404)
Atalay S, Coruh A, Deniz K (2014) Stromal vascular fraction improves deep partial thickness burn wound healing. Burns 40(7):1375–1383
Cuttle L, Nataatmadja M, Fraser JF, Kempf M, Kimble RM, Hayes MT (2005) Collagen in the scarless fetal skin wound: detection with picrosirius-polarization. Wound Rep Regen 13(2):198–204
Zerbinati N, Calligaro A (2018) Calcium hydroxylapatite treatment of human skin: evidence of collagen turnover through picrosirius red staining and circularly polarized microscopy. Clin Cosmet Investig Dermatol 11:29–35
Verhaegen PD, van Zuijlen PP, Pennings NM et al (2009) Differences in collagen architecture between keloid, hypertrophic scar, normotrophic scar, and normal skin: an objective histopathological analysis. Wound Rep Regen 17(5):649–656
Hanson SE, Kleinbeck KR, Cantu D et al (2016) Local delivery of allogeneic bone marrow and adipose tissue-derived mesenchymal stromal cells for cutaneous wound healing in a porcine model. J Tissue Eng Regen Med 10(2):E90–E100
Beausang E, Floyd H, Dunn KW, Orton CI, Ferguson MW (1998) A new quantitative scale for clinical scar assessment. Plast Reconstr Surg 102(6):1954–1961
Beanes SR, Hu FY, Soo C et al (2002) Confocal microscopic analysis of scarless repair in the fetal rat: defining the transition. Plast Reconst Surg 109:160–170
Andjelkov K, Conde-Green A, Mosahebi A (2021) Smoking and physical activity significantly influence stromal vascular fraction cell yield and viability. Aesthet Plast Surg 45(1):315–321
Dos-Anjos Vilaboa S, Navarro-Palou M, Llull R (2014) Age influence on stromal vascular fraction cell yield obtained from human lipoaspirates. Cytotherapy 16(8):1092–1097
Zuk PA, Zhu M, Mizuno H et al (2001) Multilineage cells from human adipose tissue: implications for cell-based therapies. Tissue Eng 7(2):211–228
Covarrubias P, Cardenas-Camarena L, Guerrerosantos J et al (2013) Evaluation of the histologic changes in the fat-grafted facial skin: clinical trial. Aesthet Plast Surg 37(4):778–783
Mojallal A, Lequeux C, Shipkov C et al (2009) Improvement of skin quality after fat grafting: clinical observation and an animal study. Plast Reconstr Surg 124(3):765–774
Foubert P, Zafra D, Liu M et al (2017) Autologous adipose-derived regenerative cell therapy modulates development of hypertrophic scarring in a red Duroc porcine model. Stem Cell Res Ther 8(1):261
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest
Ethical Approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Zivec, K., Veber, M., Pizem, J. et al. Intraoperative Intradermal Application of Stromal Vascular Fraction into the Abdominal Suture Line: Histological Analysis of Abdominal Scar Tissue. Aesth Plast Surg 46, 2853–2862 (2022). https://doi.org/10.1007/s00266-022-02860-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00266-022-02860-4