Abstract
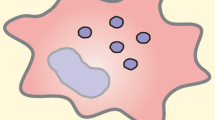
Macrophages are important precursor cell types of the innate immune system and bridge adaptive immune responses through the antigen presentation system. Meanwhile, macrophages constitute substantial portion of the stromal cells in the tumor microenvironment (TME) (referred to as tumor-associated macrophages, or TAMs) and exhibit conflicting roles in the development, invasion, and metastasis of thyroid cancer (TC). Moreover, TAMs play a crucial role to the behavior of TC due to their high degree of infiltration and prognostic relevance. Generally, TAMs can be divided into two subgroups; M1-like TAMs are capable of directly kill tumor cells, and recruiting and activating other immune cells in the early stages of cancer. However, due to changes in the TME, M2-like TAMs gradually increase and promote tumor progression. This review aims to discuss the impact of TAMs on TC, including their role in tumor promotion, gene mutation, and other factors related to the polarization of TAMs. Finally, we will explore the M2-like TAM-centered therapeutic strategies, including chemotherapy, clinical trials, and combinatorial immunotherapy.


Similar content being viewed by others
Abbreviations
- ATC:
-
Anaplastic thyroid cancer
- APC:
-
Antigen-presenting cells
- APOE:
-
Apolipoprotein E
- BRAF:
-
V-Raf murine sarcoma viral oncogene homolog B
- CAR-TAMs:
-
Chimeric antigen receptor-tumor-associated macrophages
- CCL:
-
Chemokine C-C motif ligand
- CCR:
-
C-C chemokine receptor type
- CSF-1:
-
Colony-stimulating factor
- CSF-1R:
-
Colony-stimulating factor receptor
- CTLA-4:
-
Cytotoxic T-lymphocyte-associated protein-4
- CXCL:
-
Chemokine C-X-C motif ligand
- CXCR:
-
C-X-C chemokine receptor
- DC cell:
-
Dendritic cell
- DTC:
-
Differentiated thyroid cancer
- EGF:
-
Epidermal growth factor
- EMT:
-
Epithelial-mesenchymal transition
- EVs:
-
Extracellular vehicles
- FGF:
-
Fibroblast growth factor
- FTC:
-
Follicular thyroid cancer
- GM-CSF:
-
Granulocyte-macrophage colony-stimulating factor
- HDAC:
-
Histone deacetylase
- HER2:
-
Receptor tyrosine-protein kinase erbB-2
- HGF:
-
Hepatocyte growth factor
- HIF-1α:
-
Hypoxia inducible factor-1α
- IDO:
-
Indoleamine 2,3-dioxygenase
- IFN-γ:
-
Interferons-γ
- IL:
-
Interleukin
- iNOS:
-
Inducible nitric oxide synthase
- LILRB1/2:
-
Leukocyte immunoglobulin-like receptor subfamily B1/2
- LPS:
-
Lipopolysaccharide
- MARCO:
-
Macrophage receptor with collagenous structure
- MDSC:
-
Myeloid-derived suppressor cells
- MEK:
-
Mitogen-activated protein kinase
- MET:
-
Receptor tyrosine kinase of MET proto-oncogene
- MHC-II:
-
Major histocompatibility complex class II
- MTC:
-
Medullary thyroid cancer
- miRNA:
-
MicroRNA
- MR:
-
Mannose receptor
- NF-κB:
-
Nuclear factor-κB
- NK cell:
-
Natural killer cell
- ONJ:
-
Osteonecrosis of the jaw
- PARP:
-
Poly ADP ribose polymerase
- PD-1/2:
-
Programmed cell death protein 1/2
- PDGF:
-
Platelet-derived growth factor
- PI3K:
-
Phosphoinositide 3-kinases
- PD-L1/2:
-
Programmed death-ligand 1/2
- PTC:
-
Papillary thyroid cancer
- scRNA-seq:
-
Single-cell RNA sequencing
- SIRP-α:
-
Signal regulatory protein-α
- SPP1:
-
Secreted phosphoprotein 1
- STAT3:
-
Signal transducer and activator of transcription 3
- TAMs:
-
Tumor-associated macrophage
- TC:
-
Thyroid cancer
- TGF-β:
-
Transforming growth factor-β
- Th17 cell:
-
T helper 17 cell
- TIM3:
-
T cell immunoglobulin and mucin domain-containing protein 3
- TKIs:
-
Tyrosine kinase inhibitors
- TLR:
-
Toll-like receptor
- TME:
-
Tumor microenvironment
- TNF-α:
-
Tumor necrosis factor-α
- TNM:
-
Tumor, node and metastasis
- Treg cell:
-
Regulatory T cell
- TREM2:
-
Scavenger receptor-triggering receptors expressed on myeloid cells 2
- VEGF:
-
Vascular endothelial growth factor
- VEGFR:
-
Vascular endothelial growth factor receptor
- VSIG4:
-
V-set and immunoglobulin domain containing 4
References
Wu J, Zhao X, Sun J, Cheng C, Yin C, Bai R (2022) The epidemic of thyroid cancer in China: current trends and future prediction. Front Oncol 12:932729. https://doi.org/10.3389/fonc.2022.932729
Megwalu UC, Moon PK (2022) Thyroid cancer incidence and mortality trends in the United States: 2000–2018. Thyroid 32:560–570. https://doi.org/10.1089/thy.2021.0662
Lim H, Devesa SS, Sosa JA, Check D, Kitahara CM (2017) Trends in thyroid cancer incidence and mortality in the United States, 1974–2013. JAMA 317:1338–1348. https://doi.org/10.1001/jama.2017.2719
Baloch ZW, Asa SL, Barletta JA et al (2022) Overview of the 2022 WHO classification of thyroid neoplasms. Endocr Pathol 33:27–63. https://doi.org/10.1007/s12022-022-09707-3
Oh JM, Ahn BC (2021) Molecular mechanisms of radioactive iodine refractoriness in differentiated thyroid cancer: Impaired sodium iodide symporter (NIS) expression owing to altered signaling pathway activity and intracellular localization of NIS. Theranostics 11:6251–6277. https://doi.org/10.7150/thno.57689
Stempin CC, Geysels RC, Park S et al (2021) Secreted factors by anaplastic thyroid cancer cells induce tumor-promoting M2-like macrophage polarization through a TIM3-dependent mechanism. Cancers (Basel) 13:1. https://doi.org/10.3390/cancers13194821
Jung KY, Cho SW, Kim YA, Kim D, Oh BC, Park DJ, Park YJ (2015) Cancers with higher density of tumor-associated macrophages were associated with poor survival rates. J Pathol Transl Med 49:318–324. https://doi.org/10.4132/jptm.2015.06.01
Cho SW, Kim YA, Sun HJ, Kim YA, Oh BC, Yi KH, Park DJ, Park YJ (2016) CXCL16 signaling mediated macrophage effects on tumor invasion of papillary thyroid carcinoma. Endocr Relat Cancer 23:113–124. https://doi.org/10.1530/ERC-15-0196
Fang W, Ye L, Shen L et al (2014) Tumor-associated macrophages promote the metastatic potential of thyroid papillary cancer by releasing CXCL8. Carcinogenesis 35:1780–1787. https://doi.org/10.1093/carcin/bgu060
Pan Z, Bao L, Lu X et al (2023) IL2RA(+)VSIG4(+) tumor-associated macrophage is a key subpopulation of the immunosuppressive microenvironment in anaplastic thyroid cancer. Biochim Biophys Acta Mol Basis Dis 1869:166591. https://doi.org/10.1016/j.bbadis.2022.166591
Joshi S, Singh AR, Zulcic M, Durden DL (2014) A macrophage-dominant PI3K isoform controls hypoxia-induced HIF1alpha and HIF2alpha stability and tumor growth, angiogenesis, and metastasis. Mol Cancer Res 12:1520–1531. https://doi.org/10.1158/1541-7786.MCR-13-0682
Ryder M, Ghossein RA, Ricarte-Filho JC, Knauf JA, Fagin JA (2008) Increased density of tumor-associated macrophages is associated with decreased survival in advanced thyroid cancer. Endocr Relat Cancer 15:1069–1074. https://doi.org/10.1677/ERC-08-0036
Qing W, Fang WY, Ye L et al (2012) Density of tumor-associated macrophages correlates with lymph node metastasis in papillary thyroid carcinoma. Thyroid 22:905–910. https://doi.org/10.1089/thy.2011.0452
Ryder M, Gild M, Hohl TM, Pamer E, Knauf J, Ghossein R, Joyce JA, Fagin JA (2013) Genetic and pharmacological targeting of CSF-1/CSF-1R inhibits tumor-associated macrophages and impairs BRAF-induced thyroid cancer progression. PLoS ONE 8:e54302. https://doi.org/10.1371/journal.pone.0054302
Cho JW, Kim WW, Lee YM et al (2019) Impact of tumor-associated macrophages and BRAF(V600E) mutation on clinical outcomes in patients with various thyroid cancers. Head Neck 41:686–691. https://doi.org/10.1002/hed.25469
Miyamoto T, Murakami R, Hamanishi J et al (2022) B7–H3 suppresses antitumor immunity via the CCL2-CCR2-M2 macrophage axis and contributes to ovarian cancer progression. Cancer Immunol Res 10:56–69. https://doi.org/10.1158/2326-6066.CIR-21-0407
Li X, Yao W, Yuan Y et al (2017) Targeting of tumour-infiltrating macrophages via CCL2/CCR2 signalling as a therapeutic strategy against hepatocellular carcinoma. Gut 66:157–167. https://doi.org/10.1136/gutjnl-2015-310514
Ferrari SM, Fallahi P, Galdiero MR et al (2019) Immune and Inflammatory Cells in Thyroid Cancer Microenvironment. Int J Mol Sci 20:1. https://doi.org/10.3390/ijms20184413
Shin E, Koo JS (2022) Cell component and function of tumor microenvironment in thyroid cancer. Int J Mol Sci 23:1. https://doi.org/10.3390/ijms232012578
Menicali E, Guzzetti M, Morelli S, Moretti S, Puxeddu E (2020) Immune landscape of thyroid cancers: new insights. Front Endocrinol (Lausanne) 11:637826. https://doi.org/10.3389/fendo.2020.637826
Pan Z, Xu T, Bao L et al (2022) CREB3L1 promotes tumor growth and metastasis of anaplastic thyroid carcinoma by remodeling the tumor microenvironment. Mol Cancer 21:190. https://doi.org/10.1186/s12943-022-01658-x
Wang X, Peng W, Li C, Qin R, Zhong Z, Sun C (2021) Identification of an immune-related signature indicating the dedifferentiation of thyroid cells. Cancer Cell Int 21:231. https://doi.org/10.1186/s12935-021-01939-3
Rodell CB, Arlauckas SP, Cuccarese MF, Garris CS, Li R, Ahmed MS, Kohler RH, Pittet MJ, Weissleder R (2018) TLR7/8-agonist-loaded nanoparticles promote the polarization of tumour-associated macrophages to enhance cancer immunotherapy. Nat Biomed Eng 2:578–588. https://doi.org/10.1038/s41551-018-0236-8
Bao L, Xu T, Lu X, Huang P, Pan Z, Ge M (2021) Metabolic reprogramming of thyroid cancer cells and crosstalk in their microenvironment. Front Oncol 11:773028. https://doi.org/10.3389/fonc.2021.773028
Galdiero MR, Varricchi G, Marone G (2016) The immune network in thyroid cancer. Oncoimmunology 5:e1168556. https://doi.org/10.1080/2162402X.2016.1168556
Angell TE, Lechner MG, Jang JK, Correa AJ, LoPresti JS, Epstein AL (2014) BRAF V600E in papillary thyroid carcinoma is associated with increased programmed death ligand 1 expression and suppressive immune cell infiltration. Thyroid 24:1385–1393. https://doi.org/10.1089/thy.2014.0134
Lopez-Yrigoyen M, Cassetta L, Pollard JW (2021) Macrophage targeting in cancer. Ann N Y Acad Sci 1499:18–41. https://doi.org/10.1111/nyas.14377
Liu Q, Sun W, Zhang H (2022) Roles and new insights of macrophages in the tumor microenvironment of thyroid cancer. Front Pharmacol 13:875384. https://doi.org/10.3389/fphar.2022.875384
Li B, Liu S, Yang Q, Li Z, Li J, Wu J, Sun S, Xu Z, Wu Q (2023) Macrophages in tumor-associated adipose microenvironment accelerate tumor progression. Adv Biol (Weinh) 7:e2200161. https://doi.org/10.1002/adbi.202200161
Lv J, Liu C, Chen FK, Feng ZP, Jia L, Liu PJ, Yang ZX, Hou F, Deng ZY (2021) M2-like tumour-associated macrophage-secreted IGF promotes thyroid cancer stemness and metastasis by activating the PI3K/AKT/mTOR pathway. Mol Med Rep 24:1. https://doi.org/10.3892/mmr.2021.12249
Duan Z, Luo Y (2021) Targeting macrophages in cancer immunotherapy. Signal Transduct Target Ther 6:127. https://doi.org/10.1038/s41392-021-00506-6
Passaro C, Borriello F, Vastolo V, Di Somma S, Scamardella E, Gigantino V, Franco R, Marone G, Portella G (2016) The oncolytic virus dl922-947 reduces IL-8/CXCL8 and MCP-1/CCL2 expression and impairs angiogenesis and macrophage infiltration in anaplastic thyroid carcinoma. Oncotarget 7:1500–1515. https://doi.org/10.18632/oncotarget.6430
Qiao L, Dong C, Jia W, Ma B (2022) Exosomal miR-655-3p inhibits growth, and invasion and macrophage M2 polarization through targeting CXCR4 in papillary thyroid carcinoma. Acta Biochim Pol 69:773–779. https://doi.org/10.18388/abp.2020_6027
Onuma AE, Schoenfield L, Shen C, Edwards C, Phay JE, Shirley LA, Tsung A (2020) Prognosis of macrophage density in the absence of neutrophils in differentiated thyroid cancer. J Surg Res 256:458–467. https://doi.org/10.1016/j.jss.2020.07.032
Mantovani A, Sica A, Sozzani S, Allavena P, Vecchi A, Locati M (2004) The chemokine system in diverse forms of macrophage activation and polarization. Trends Immunol 25:677–686. https://doi.org/10.1016/j.it.2004.09.015
Yao Y, Xu XH, Jin L (2019) Macrophage polarization in physiological and pathological pregnancy. Front Immunol 10:792. https://doi.org/10.3389/fimmu.2019.00792
Dungan LS, McGuinness NC, Boon L, Lynch MA, Mills KH (2014) Innate IFN-γ promotes development of experimental autoimmune encephalomyelitis: a role for NK cells and M1 macrophages. Eur J Immunol 44:2903–2917. https://doi.org/10.1002/eji.201444612
Liu J, Geng X, Hou J, Wu G (2021) New insights into M1/M2 macrophages: key modulators in cancer progression. Cancer Cell Int 21:389. https://doi.org/10.1186/s12935-021-02089-2
Kranz LM, Diken M, Haas H et al (2016) Systemic RNA delivery to dendritic cells exploits antiviral defence for cancer immunotherapy. Nature 534:396–401. https://doi.org/10.1038/nature18300
Mantovani A, Marchesi F, Malesci A, Laghi L, Allavena P (2017) Tumour-associated macrophages as treatment targets in oncology. Nat Rev Clin Oncol 14:399–416. https://doi.org/10.1038/nrclinonc.2016.217
DeNardo DG, Ruffell B (2019) Macrophages as regulators of tumour immunity and immunotherapy. Nat Rev Immunol 19:369–382. https://doi.org/10.1038/s41577-019-0127-6
Mantovani A, Allavena P, Marchesi F, Garlanda C (2022) Macrophages as tools and targets in cancer therapy. Nat Rev Drug Discov 21:799–820. https://doi.org/10.1038/s41573-022-00520-5
Kim MJ, Sun HJ, Song YS, Yoo SK, Kim YA, Seo JS, Park YJ, Cho SW (2019) CXCL16 positively correlated with M2-macrophage infiltration, enhanced angiogenesis, and poor prognosis in thyroid cancer. Sci Rep 9:13288. https://doi.org/10.1038/s41598-019-49613-z
Okikawa S, Morine Y, Saito Y et al (2022) Inhibition of the VEGF signaling pathway attenuates tumor-associated macrophage activity in liver cancer. Oncol Rep 47:1. https://doi.org/10.3892/or.2022.8282
Kabasawa T, Ohe R, Aung NY, Urano Y, Kitaoka T, Tamazawa N, Utsunomiya A, Yamakawa M (2021) Potential role of M2 TAMs around lymphatic vessels during lymphatic invasion in papillary thyroid carcinoma. Sci Rep 11:1150. https://doi.org/10.1038/s41598-020-80694-3
Jing W, Guo X, Wang G, Bi Y, Han L, Zhu Q, Qiu C, Tanaka M, Zhao Y (2020) Breast cancer cells promote CD169(+) macrophage-associated immunosuppression through JAK2-mediated PD-L1 upregulation on macrophages. Int Immunopharmacol 78:106012. https://doi.org/10.1016/j.intimp.2019.106012
Hartley GP, Chow L, Ammons DT, Wheat WH, Dow SW (2018) Programmed cell death ligand 1 (PD-L1) signaling regulates macrophage proliferation and activation. Cancer Immunol Res 6:1260–1273. https://doi.org/10.1158/2326-6066.CIR-17-0537
Lv J, Feng ZP, Chen FK, Liu C, Jia L, Liu PJ, Yang CZ, Hou F, Deng ZY (2021) M2-like tumor-associated macrophages-secreted Wnt1 and Wnt3a promotes dedifferentiation and metastasis via activating β-catenin pathway in thyroid cancer. Mol Carcinog 60:25–37. https://doi.org/10.1002/mc.23268
Lan J, Sun L, Xu F et al (2019) M2 macrophage-derived exosomes promote cell migration and invasion in colon cancer. Cancer Res 79:146–158. https://doi.org/10.1158/0008-5472.CAN-18-0014
Matsubayashi S, Kawai K, Matsumoto Y et al (1995) The correlation between papillary thyroid carcinoma and lymphocytic infiltration in the thyroid gland. J Clin Endocrinol Metab 80:3421–3424. https://doi.org/10.1210/jcem.80.12.8530576
Cunha LL, Ward LS (2022) Translating the immune microenvironment of thyroid cancer into clinical practice. Endocr Relat Cancer 29:R67–R83. https://doi.org/10.1530/ERC-21-0414
Stempin CC, Geysels RC, Park S et al (2021) Secreted factors by anaplastic thyroid cancer cells induce tumor-promoting M2-like macrophage polarization through a TIM3-dependent mechanism. Cancers 13:4821
Zhang P, Guan H, Yuan S et al (2022) Targeting myeloid derived suppressor cells reverts immune suppression and sensitizes BRAF-mutant papillary thyroid cancer to MAPK inhibitors. Nat Commun 13:1588. https://doi.org/10.1038/s41467-022-29000-5
Spourquet C, Delcorte O, Lemoine P et al (2022) BRAF(V600E) expression in thyrocytes causes recruitment of immunosuppressive STABILIN-1 macrophages. Cancers (Basel) 14:1. https://doi.org/10.3390/cancers14194687
Xing M (2016) Clinical utility of RAS mutations in thyroid cancer: a blurred picture now emerging clearer. BMC Med 14:12. https://doi.org/10.1186/s12916-016-0559-9
Aydogan BI, Yuksel B, Tuna MM et al (2016) Distribution of RET mutations and evaluation of treatment approaches in hereditary medullary thyroid carcinoma in Turkey. J Clin Res Pediatr Endocrinol 8:13–20. https://doi.org/10.4274/jcrpe.2219
Pu W, Shi X, Yu P et al (2021) Single-cell transcriptomic analysis of the tumor ecosystems underlying initiation and progression of papillary thyroid carcinoma. Nat Commun 12:6058. https://doi.org/10.1038/s41467-021-26343-3
Borrello MG, Alberti L, Fischer A et al (2005) Induction of a proinflammatory program in normal human thyrocytes by the RET/PTC1 oncogene. Proc Natl Acad Sci USA 102:14825–14830. https://doi.org/10.1073/pnas.0503039102
Cho JW, Kim WW, Lee YM et al (2019) Impact of tumor-associated macrophages and BRAF. Head Neck 41:686–691. https://doi.org/10.1002/hed.25469
Cho SW, Kim YA, Sun HJ, Oh BC, Yi KH, Park DJ, Park YJ (2016) CXCL16 signaling mediated macrophage effects on tumor invasion of papillary thyroid carcinoma. Endocr Relat Cancer 23:113–124. https://doi.org/10.1530/ERC-15-0196
Luo Y, Yang YC, Ma B, Xu WB, Liao T, Wang Y (2022) Integrated analysis of novel macrophage related signature in anaplastic thyroid cancer. Endocrine 78:517–530. https://doi.org/10.1007/s12020-022-03179-5
Melillo RM, Castellone MD, Guarino V et al (2016) The RET/PTC-RAS-BRAF linear signaling cascade mediates the motile and mitogenic phenotype of thyroid cancer cells. J Clin Invest 126:1603. https://doi.org/10.1172/JCI87345
Xing M, Alzahrani AS, Carson KA et al (2015) Association between BRAF V600E mutation and recurrence of papillary thyroid cancer. J Clin Oncol 33:42–50. https://doi.org/10.1200/JCO.2014.56.8253
Ferrari SM, Elia G, Piaggi S, Baldini E, Ulisse S, Miccoli M, Materazzi G, Antonelli A, Fallahi P (2018) CCL2 is modulated by cytokines and PPAR-γ in anaplastic thyroid cancer. Anti-Cancer Agents Med Chem 18:458–466
Ma M, Lin B, Wang M, Liang X, Su L, Okose O, Lv W, Li J (2020) Immunotherapy in anaplastic thyroid cancer. Am J Transl Res 12:974–988
Cassetta L, Kitamura T (2018) Targeting tumor-associated macrophages as a potential strategy to enhance the response to immune checkpoint inhibitors. Front Cell Dev Biol 6:38. https://doi.org/10.3389/fcell.2018.00038
Kim DI, Kim E, Kim YA, Cho SW, Lim JA, Park YJ (2016) Macrophage densities correlated with CXC chemokine receptor 4 expression and related with poor survival in anaplastic thyroid cancer. Endocrinol Metab (Seoul) 31:469–475. https://doi.org/10.3803/EnM.2016.31.3.469
Lv J, Chen FK, Liu C, Liu PJ, Feng ZP, Jia L, Yang ZX, Hou F, Deng ZY (2020) Zoledronic acid inhibits thyroid cancer stemness and metastasis by repressing M2-like tumor-associated macrophages induced Wnt/β-catenin pathway. Life Sci 256:117925. https://doi.org/10.1016/j.lfs.2020.117925
Mazzoni M, Mauro G, Erreni M et al (2019) Senescent thyrocytes and thyroid tumor cells induce M2-like macrophage polarization of human monocytes via a PGE2-dependent mechanism. J Exp Clin Cancer Res 38:208. https://doi.org/10.1186/s13046-019-1198-8
Liu H, Dong H, Jiang L, Li Z, Ma X (2018) Bleomycin inhibits proliferation and induces apoptosis in TPC-1 cells through reversing M2-macrophages polarization. Oncol Lett 16:3858–3866. https://doi.org/10.3892/ol.2018.9103
Luo H, Xia X, Kim GD et al (2021) Characterizing dedifferentiation of thyroid cancer by integrated analysis. Sci Adv 7:1. https://doi.org/10.1126/sciadv.abf3657
Yu X, Wang D, Wang X, Sun S, Zhang Y, Wang S, Miao R, Xu X, Qu X (2019) CXCL12/CXCR4 promotes inflammation-driven colorectal cancer progression through activation of RhoA signaling by sponging miR-133a-3p. J Exp Clin Cancer Res 38:32. https://doi.org/10.1186/s13046-018-1014-x
Aust G, Hofmann A, Laue S, Ode-Hakim S, Scherbaum WA (1996) Differential regulation of granulocyte-macrophage colony-stimulating factor mRNA and protein expression in human thyrocytes and thyroid-derived fibroblasts by interleukin-1 alpha and tumor necrosis factor-alpha. J Endocrinol 151:277–285. https://doi.org/10.1677/joe.0.1510277
Li W, Liu Z, Cen X, Xu J, Zhao S, Wang B, Zhang W, Qiu M (2022) Integrated analysis of fibroblasts molecular features in papillary thyroid cancer combining single-cell and bulk RNA sequencing technology. Front Endocrinol (Lausanne) 13:1019072. https://doi.org/10.3389/fendo.2022.1019072
Ferrari SM, Elia G, Piaggi S, Baldini E, Ulisse S, Miccoli M, Materazzi G, Antonelli A, Fallahi P (2018) CCL2 is Modulated by Cytokines and PPAR-γ in Anaplastic Thyroid Cancer. Anticancer Agents Med Chem 18:458–466. https://doi.org/10.2174/1871520617666170719152349
Wang D, Wang X, Si M, Yang J, Sun S, Wu H, Cui S, Qu X, Yu X (2020) Exosome-encapsulated miRNAs contribute to CXCL12/CXCR4-induced liver metastasis of colorectal cancer by enhancing M2 polarization of macrophages. Cancer Lett 474:36–52. https://doi.org/10.1016/j.canlet.2020.01.005
Baek SH, Lee HW, Gangadaran P, Oh JM, Zhu L, Rajendran RL, Lee J, Ahn BC (2020) Role of M2-like macrophages in the progression of ovarian cancer. Exp Cell Res 395:112211. https://doi.org/10.1016/j.yexcr.2020.112211
de Azevedo RA, Shoshan E, Whang S, Markel G, Jaiswal AR, Liu A, Curran MA, Travassos LR, Bar-Eli M (2020) MIF inhibition as a strategy for overcoming resistance to immune checkpoint blockade therapy in melanoma. Oncoimmunology 9:1846915. https://doi.org/10.1080/2162402X.2020.1846915
Ghoochani A, Schwarz MA, Yakubov E, Engelhorn T, Doerfler A, Buchfelder M, Bucala R, Savaskan NE, Eyüpoglu IY (2016) MIF-CD74 signaling impedes microglial M1 polarization and facilitates brain tumorigenesis. Oncogene 35:6246–6261. https://doi.org/10.1038/onc.2016.160
Sloot YJE, Rabold K, Ulas T et al (2019) Interplay between thyroid cancer cells and macrophages: effects on IL-32 mediated cell death and thyroid cancer cell migration. Cell Oncol (Dordr) 42:691–703. https://doi.org/10.1007/s13402-019-00457-9
He L, Qing F, Li M, Lan D (2021) Effects of laparoscopic and traditional open surgery on the levels of IL-6, TNF-α, and Gal-3 in patients with thyroid cancer. Gland Surg 10:1085–1092. https://doi.org/10.21037/gs-21-60
Madani I, De Neve W, Mareel M (2008) Does ionizing radiation stimulate cancer invasion and metastasis? Bull Cancer 95:292–300. https://doi.org/10.1684/bdc.2008.0598
Sherman EJ, Harris J, Bible KC et al (2023) Radiotherapy and paclitaxel plus pazopanib or placebo in anaplastic thyroid cancer (NRG/RTOG 0912): a randomised, double-blind, placebo-controlled, multicentre, phase 2 trial. Lancet Oncol 24:175–186. https://doi.org/10.1016/s1470-2045(22)00763-x
Cui YH, Suh Y, Lee HJ et al (2015) Radiation promotes invasiveness of non-small-cell lung cancer cells through granulocyte-colony-stimulating factor. Oncogene 34:5372–5382. https://doi.org/10.1038/onc.2014.466
Mathew B, Jacobson JR, Siegler JH et al (2013) Role of migratory inhibition factor in age-related susceptibility to radiation lung injury via NF-E2-related factor-2 and antioxidant regulation. Am J Respir Cell Mol Biol 49:269–278. https://doi.org/10.1165/rcmb.2012-0291OC
Zhang C, Gu X, Pan M, Yuan Q, Cheng H (2021) Senescent thyroid tumor cells promote their migration by inducing the polarization of M2-like macrophages. Clin Transl Oncol 23:1253–1261. https://doi.org/10.1007/s12094-020-02516-2
Cheng Z, Wang L, Wu C, Huang L, Ruan Y, Xue W (2021) Tumor-derived exosomes induced M2 macrophage polarization and promoted the metastasis of osteosarcoma cells through Tim-3. Arch Med Res 52:200–210. https://doi.org/10.1016/j.arcmed.2020.10.018
Weitzman SP, Sherman SI (2019) Novel drug treatments of progressive radioiodine-refractory differentiated thyroid cancer. Endocrinol Metab Clin North Am 48:253–268. https://doi.org/10.1016/j.ecl.2018.10.009
Kim DW, Jung YS, Park HS, Jung HD (2013) Osteonecrosis of the jaw related to everolimus: a case report. Br J Oral Maxillofac Surg 51:e302–e304. https://doi.org/10.1016/j.bjoms.2013.09.008
Magaway C, Kim E, Jacinto E (2019) Targeting mTOR and metabolism in cancer: lessons and innovations. Cells 8:1. https://doi.org/10.3390/cells8121584
Gunda V, Gigliotti B, Ashry T et al (2019) Anti-PD-1/PD-L1 therapy augments lenvatinib’s efficacy by favorably altering the immune microenvironment of murine anaplastic thyroid cancer. Int J Cancer 144:2266–2278. https://doi.org/10.1002/ijc.32041
Cassetta L, Pollard JW (2018) Targeting macrophages: therapeutic approaches in cancer. Nat Rev Drug Discov 17:887–904. https://doi.org/10.1038/nrd.2018.169
Huang JK, Ma L, Song WH, Lu BY, Huang YB, Dong HM, Ma XK, Zhu ZZ, Zhou R (2017) LncRNA-MALAT1 promotes angiogenesis of thyroid cancer by modulating tumor-associated macrophage FGF2 protein secretion. J Cell Biochem 118:4821–4830. https://doi.org/10.1002/jcb.26153
Dowlati A, Harvey RD, Carvajal RD et al (2021) LY3022855, an anti-colony stimulating factor-1 receptor (CSF-1R) monoclonal antibody, in patients with advanced solid tumors refractory to standard therapy: phase 1 dose-escalation trial. Invest New Drugs 39:1057–1071. https://doi.org/10.1007/s10637-021-01084-8
Li XJ, Gangadaran P, Kalimuthu S, Oh JM, Zhu L, Jeong SY, Lee SW, Lee J, Ahn BC (2016) Role of pulmonary macrophages in initiation of lung metastasis in anaplastic thyroid cancer. Int J Cancer 139:2583–2592. https://doi.org/10.1002/ijc.30387
Varricchi G, Loffredo S, Marone G, Modestino L, Fallahi P, Ferrari SM, de Paulis A, Antonelli A, Galdiero MR (2019) The immune landscape of thyroid cancer in the context of immune checkpoint inhibition. Int J Mol Sci 20:1. https://doi.org/10.3390/ijms20163934
Chen S, Morine Y, Tokuda K, Yamada S, Saito Y, Nishi M, Ikemoto T, Shimada M (2021) Cancer-associated fibroblast-induced M2-polarized macrophages promote hepatocellular carcinoma progression via the plasminogen activator inhibitor-1 pathway. Int J Oncol 59:1. https://doi.org/10.3892/ijo.2021.5239
Rashid K, Ahmad A, Meerasa SS, Khan AQ, Wu X, Liang L, Cui Y, Liu T (2023) Cancer stem cell-derived exosome-induced metastatic cancer: an orchestra within the tumor microenvironment. Biochimie. https://doi.org/10.1016/j.biochi.2023.03.014
Gonzalez-Melero L, Hernandez RM, Santos-Vizcaino E, Igartua M (2023) Tumour-derived extracellular vesicle based vaccines for melanoma treatment. Drug Deliv Transl Res. https://doi.org/10.1007/s13346-023-01328-5
Zhao S, Mi Y, Guan B et al (2020) Tumor-derived exosomal miR-934 induces macrophage M2 polarization to promote liver metastasis of colorectal cancer. J Hematol Oncol 13:156. https://doi.org/10.1186/s13045-020-00991-2
Ying X, Wu Q, Wu X, Zhu Q, Wang X, Jiang L, Chen X (2016) Epithelial ovarian cancer-secreted exosomal miR-222-3p induces polarization of tumor-associated macrophages. Oncotarget 7:43076–43087. https://doi.org/10.18632/oncotarget.9246
Shinohara H, Kuranaga Y, Kumazaki M, Sugito N, Yoshikawa Y, Takai T, Taniguchi K, Ito Y, Akao Y (2017) Regulated polarization of tumor-associated macrophages by miR-145 via colorectal cancer-derived extracellular vesicles. J Immunol 199:1505–1515. https://doi.org/10.4049/jimmunol.1700167
Chen X, Zhou J, Li X, Wang X, Lin Y (2018) Exosomes derived from hypoxic epithelial ovarian cancer cells deliver microRNAs to macrophages and elicit a tumor-promoted phenotype. Cancer Lett 435:80–91. https://doi.org/10.1016/j.canlet.2018.08.001
Huang X, Yuan T, Liang M et al (2015) Exosomal miR-1290 and miR-375 as prognostic markers in castration-resistant prostate cancer. Eur Urol 67:33–41. https://doi.org/10.1016/j.eururo.2014.07.035
Huang D, Qiu H, Miao L, Guo L, Zhang X, Lin M, Li Z, Li F (2022) Cdc42 promotes thyroid cancer cell proliferation and migration and tumor-associated macrophage polarization through the PTEN/AKT pathway. J Biochem Mol Toxicol 36:e23115. https://doi.org/10.1002/jbt.23115
Hou X, Shi X, Zhang W et al (2021) LDHA induces EMT gene transcription and regulates autophagy to promote the metastasis and tumorigenesis of papillary thyroid carcinoma. Cell Death Dis 12:347. https://doi.org/10.1038/s41419-021-03641-8
Cassetta L, Pollard JW (2023) A timeline of tumour-associated macrophage biology. Nat Rev Cancer 23:238–257. https://doi.org/10.1038/s41568-022-00547-1
von Tresckow B, Morschhauser F, Ribrag V et al (2015) An open-label, multicenter, phase I/II study of JNJ-40346527, a CSF-1R inhibitor, in patients with relapsed or refractory hodgkin lymphoma. Clin Cancer Res 21:1843–1850. https://doi.org/10.1158/1078-0432.CCR-14-1845
Pass HI, Lavilla C, Canino C, Goparaju C, Preiss J, Noreen S, Blandino G, Cioce M (2016) Inhibition of the colony-stimulating-factor-1 receptor affects the resistance of lung cancer cells to cisplatin. Oncotarget 7:56408–56421. https://doi.org/10.18632/oncotarget.10895
Passaro C, Volpe M, Botta G, Scamardella E, Perruolo G, Gillespie D, Libertini S, Portella G (2015) PARP inhibitor olaparib increases the oncolytic activity of dl922-947 in in vitro and in vivo model of anaplastic thyroid carcinoma. Mol Oncol 9:78–92. https://doi.org/10.1016/j.molonc.2014.07.022
Schürch CM, Roelli MA, Forster S et al (2019) Targeting CD47 in anaplastic thyroid carcinoma enhances tumor phagocytosis by macrophages and is a promising therapeutic strategy. Thyroid 29:979–992. https://doi.org/10.1089/thy.2018.0555
Capdevila J, Wirth LJ, Ernst T et al (2020) PD-1 blockade in anaplastic thyroid carcinoma. J Clin Oncol 38:2620–2627. https://doi.org/10.1200/JCO.19.02727
Chae YK, Othus M, Patel S et al. (2020) 270 A phase II basket trial of dual anti-CTLA-4 and anti-PD-1 blockade in rare tumors (DART) SWOG S1609: the thyroid tumor cohort. J ImmunoTherapy Cancer 8: A161-A. https://doi.org/10.1136/jitc-2020-SITC2020.0270
Zhu Y, Knolhoff BL, Meyer MA et al (2014) CSF1/CSF1R blockade reprograms tumor-infiltrating macrophages and improves response to T-cell checkpoint immunotherapy in pancreatic cancer models. Cancer Res 74:5057–5069. https://doi.org/10.1158/0008-5472.CAN-13-3723
Rodriguez-Perdigon M, Jimaja S, Haeni L, Bruns N, Rothen-Rutishauser B, Ruegg C (2022) Polymersomes-mediated delivery of CSF1R inhibitor to tumor associated macrophages promotes M2 to M1-Like macrophage repolarization. Macromol Biosci 22:e2200168. https://doi.org/10.1002/mabi.202200168
Wen J, Wang S, Guo R, Liu D (2023) CSF1R inhibitors are emerging immunotherapeutic drugs for cancer treatment. Eur J Med Chem 245:114884. https://doi.org/10.1016/j.ejmech.2022.114884
Roskoski R (2020) Properties of FDA-approved small molecule protein kinase inhibitors: A 2020 update. Pharmacol Res 152:104609. https://doi.org/10.1016/j.phrs.2019.104609
A Study of ARRY-382 in Patients With Selected Advanced or Metastatic Cancers. https://ClinicalTrials.gov/show/NCT01316822
Phase 1 Study of PLX7486 as Single Agent in Patients With Advanced Solid Tumors. https://ClinicalTrials.gov/show/NCT01804530
A Study of BLZ945 Single Agent or BLZ945 in Combination With PDR001 in Advanced Solid Tumors. https://ClinicalTrials.gov/show/NCT02829723
Gomez-Roca CA, Italiano A, Le Tourneau C et al (2019) Phase I study of emactuzumab single agent or in combination with paclitaxel in patients with advanced/metastatic solid tumors reveals depletion of immunosuppressive M2-like macrophages. Ann Oncol 30:1381–1392. https://doi.org/10.1093/annonc/mdz163
Papadopoulos KP, Gluck L, Martin LP et al (2017) First-in-human study of AMG 820, a monoclonal anti-colony-stimulating factor 1 receptor antibody, in patients with advanced solid tumors. Clin Cancer Res 23:5703–5710. https://doi.org/10.1158/1078-0432.CCR-16-3261
Razak AR, Cleary JM, Moreno V et al (2020) Safety and efficacy of AMG 820, an anti-colony-stimulating factor 1 receptor antibody, in combination with pembrolizumab in adults with advanced solid tumors. J Immunother Cancer 8:1. https://doi.org/10.1136/jitc-2020-001006
Study of Cabiralizumab in Combination With Nivolumab in Patients With Selected Advanced Cancers. https://ClinicalTrials.gov/show/NCT02526017
A Study of Cabiralzumab Given by Itself or With Nivolumab in Advanced Cancer or Cancer That Has Spread. https://ClinicalTrials.gov/show/NCT03158272
MCS110 With BRAF/MEK Inhibition in Patients With Melanoma. https://ClinicalTrials.gov/show/NCT03455764
Luo J, Wang Y, Zhao L, Wang C, Zhang Z (2022) Anti-anaplastic thyroid cancer (ATC) effects and mechanisms of PLX3397 (Pexidartinib), a multi-targeted tyrosine kinase inhibitor (TKI). Cancers (Basel) 15:1. https://doi.org/10.3390/cancers15010172
A Combination Clinical Study of PLX3397 and Pembrolizumab To Treat Advanced Melanoma and Other Solid Tumors. https://ClinicalTrials.gov/show/NCT02452424
A Study of LY3022855 in Combination With Durvalumab or Tremelimumab in Participants With Advanced Solid Tumors. https://ClinicalTrials.gov/show/NCT02718911
Tap WD, Wainberg ZA, Anthony SP et al (2015) Structure-guided blockade of CSF1R kinase in tenosynovial giant-cell tumor. N Engl J Med 373:428–437. https://doi.org/10.1056/NEJMoa1411366
Salajegheh A, Pakneshan S, Rahman A et al (2013) Co-regulatory potential of vascular endothelial growth factor-A and vascular endothelial growth factor-C in thyroid carcinoma. Hum Pathol 44:2204–2212. https://doi.org/10.1016/j.humpath.2013.04.014
Hamada Y, Tanoue K, Kita Y et al (2023) Vascular endothelial growth factor inhibitors promote antitumor responses via tumor microenvironment immunosuppression in advanced colorectal cancer. Scand J Gastroenterol 1:1–12. https://doi.org/10.1080/00365521.2023.2194011
Dong F, Ruan S, Wang J, Xia Y, Le K, Xiao X, Hu T, Wang Q (2020) M2 macrophage-induced lncRNA PCAT6 facilitates tumorigenesis and angiogenesis of triple-negative breast cancer through modulation of VEGFR2. Cell Death Dis 11:728. https://doi.org/10.1038/s41419-020-02926-8
Andrade F, Probstner D, Decnop M, Bulzico D, Momesso D, Corbo R, Vaisman M, Vaisman F (2019) The impact of zoledronic acid and radioactive iodine therapy on morbi-mortality of patients with bone metastases of thyroid cancer derived from follicular cells. Eur Thyroid J 8:46–55. https://doi.org/10.1159/000493190
Iniguez-Ariza NM, Bible KC, Clarke BL (2020) Bone metastases in thyroid cancer. J Bone Oncol 21:100282. https://doi.org/10.1016/j.jbo.2020.100282
Coperchini F, Greco A, Croce L, Petrosino E, Grillini B, Magri F, Chiovato L, Rotondi M (2022) Vitamin D reduces thyroid cancer cells migration independently from the modulation of CCL2 and CXCL8 chemokines secretion. Front Endocrinol (Lausanne) 13:876397. https://doi.org/10.3389/fendo.2022.876397
The Role of Vitamin D3 Supplementation in Advanced Cancer Patients With Pain. https://ClinicalTrials.gov/show/NCT05450419
Bonapace L, Coissieux M-M, Wyckoff J, Mertz KD, Varga Z, Junt T, Bentires-Alj M (2014) Cessation of CCL2 inhibition accelerates breast cancer metastasis by promoting angiogenesis. Nature 515:130–133. https://doi.org/10.1038/nature13862
Hitchcock JR, Watson CJ (2015) Anti-CCL2: building a reservoir or opening the floodgates to metastasis? Breast Cancer Res 17:68. https://doi.org/10.1186/s13058-015-0573-4
Arwert EN, Harney AS, Entenberg D, Wang Y, Sahai E, Pollard JW, Condeelis JS (2018) A Unidirectional Transition from Migratory to Perivascular Macrophage Is Required for Tumor Cell Intravasation. Cell Rep 23:1239–1248. https://doi.org/10.1016/j.celrep.2018.04.007
Khan SU, Khan MU, Din AU, M, Khan IM, Khan MI, Bungau S, Hassan SSU, (2023) Reprogramming tumor-associated macrophages as a unique approach to target tumor immunotherapy. Front Immunol 14:1166487. https://doi.org/10.3389/fimmu.2023.1166487
Yang Y, Xia S, Zhang L, Wang W, Chen L, Zhan W (2020) MiR-324-5p/PTPRD/CEBPD axis promotes papillary thyroid carcinoma progression via microenvironment alteration. Cancer Biol Ther 21:522–532. https://doi.org/10.1080/15384047.2020.1736465
Chen HM, van der Touw W, Wang YS et al (2018) Blocking immunoinhibitory receptor LILRB2 reprograms tumor-associated myeloid cells and promotes antitumor immunity. J Clin Invest 128:5647–5662. https://doi.org/10.1172/JCI97570
Yin SP, Gao Y, Xie XS, Xu DD, Riabov V, Du WD (2020) Accumulation of stabilin-1 positive macrophages in the early stage of gastric cancer is associated with short cumulative survival. Oncol Lett 19:2404–2412. https://doi.org/10.3892/ol.2020.11310
Fiani ML, Barreca V, Sargiacomo M, Ferrantelli F, Manfredi F, Federico M (2020) Exploiting manipulated small extracellular vesicles to subvert immunosuppression at the tumor microenvironment through mannose receptor/CD206 targeting. Int J Mol Sci 21:1. https://doi.org/10.3390/ijms21176318
Zhou Y, Do DC, Ishmael FT et al (2018) Mannose receptor modulates macrophage polarization and allergic inflammation through miR-511-3p. J Allergy Clin Immunol 141:350–64.e8. https://doi.org/10.1016/j.jaci.2017.04.049
Jaynes JM, Sable R, Ronzetti M et al (2020) Mannose receptor (CD206) activation in tumor-associated macrophages enhances adaptive and innate antitumor immune responses. Sci Transl Med 12:1. https://doi.org/10.1126/scitranslmed.aax6337
Mazzoni M, Mauro G, Minoli L et al (2021) Senescent thyrocytes, similarly to thyroid tumor cells, elicit M2-like macrophage polarization in vivo. Biology (Basel) 10:1. https://doi.org/10.3390/biology10100985
Borson-Chazot F, Dantony E, Illouz F et al (2018) Effect of Buparlisib, a Pan-Class I PI3K inhibitor, in refractory follicular and poorly differentiated thyroid cancer. Thyroid 28:1174–1179. https://doi.org/10.1089/thy.2017.0663
Kim YD, Park SM, Ha HC, Lee AR, Won H, Cha H, Cho S, Cho JM (2020) HDAC inhibitor, CG-745, enhances the anti-cancer effect of anti-PD-1 immune checkpoint inhibitor by modulation of the immune microenvironment. J Cancer 11:4059–4072. https://doi.org/10.7150/jca.44622
Han Y, Sun J, Yang Y, Liu Y, Lou J, Pan H, Yao J, Han W (2022) TMP195 exerts antitumor effects on colorectal cancer by promoting M1 macrophages polarization. Int J Biol Sci 18:5653–5666. https://doi.org/10.7150/ijbs.73264
Wang S, Hu G, Chen L, Ma K, Hu C, Zhu H, Xu N, Zhou C, Liu M (2023) Celastrol acts as a new histone deacetylase inhibitor to inhibit colorectal cancer cell growth via regulating macrophage polarity. Cell Biol Int 47:492–501. https://doi.org/10.1002/cbin.11952
Woyach JA, Kloos RT, Ringel MD, Arbogast D, Collamore M, Zwiebel JA, Grever M, Villalona-Calero M, Shah MH (2009) Lack of therapeutic effect of the histone deacetylase inhibitor vorinostat in patients with metastatic radioiodine-refractory thyroid carcinoma. J Clin Endocrinol Metab 94:164–170. https://doi.org/10.1210/jc.2008-1631
Chen JS, Hsieh YC, Chou CH, Wu YH, Yang MH, Chu SH, Chao YS, Chen CN (2022) Chidamide plus tyrosine kinase inhibitor remodel the tumor immune microenvironment and reduce tumor progression when combined with immune checkpoint inhibitor in naïve and anti-PD-1 resistant CT26-bearing mice. Int J Mol Sci 23:1. https://doi.org/10.3390/ijms231810677
Spartalis E, Kotrotsios K, Chrysikos D et al (2021) Histone deacetylase inhibitors and papillary thyroid cancer. Curr Pharm Des 27:2199–2208. https://doi.org/10.2174/1381612826666201211112234
Lin SF, Lin JD, Chou TC, Huang YY, Wong RJ (2013) Utility of a histone deacetylase inhibitor (PXD101) for thyroid cancer treatment. PLoS ONE 8:e77684. https://doi.org/10.1371/journal.pone.0077684
Sym023 (Anti-TIM-3) in Patients With Advanced Solid Tumor Malignancies or Lymphomas. https://ClinicalTrials.gov/show/NCT03489343
Solís-Martínez R, Cancino-Marentes M, Hernández-Flores G et al (2018) Regulation of immunophenotype modulation of monocytes-macrophages from M1 into M2 by prostate cancer cell-culture supernatant via transcription factor STAT3. Immunol Lett 196:140–148. https://doi.org/10.1016/j.imlet.2018.02.009
Kubala MH, Punj V, Placencio-Hickok VR, Fang H, Fernandez GE, Sposto R, DeClerck YA (2018) Plasminogen activator inhibitor-1 promotes the recruitment and polarization of macrophages in cancer. Cell Rep 25:2177–91.e7. https://doi.org/10.1016/j.celrep.2018.10.082
Oral STAT3 Inhibitor, TTI-101, in Patients With Advanced Cancers. https://ClinicalTrials.gov/show/NCT03195699
Phase I/II Open Label Study Evaluating the Safety and Efficacy of Combining STAT3 Inhibition (TTI-101) With Anti-PD-1 Therapy (Pembrolizumab) in Patients With Recurrent or Metastatic (RM) Head and Neck Squamous Cell Carcinoma (HNSCC). https://ClinicalTrials.gov/show/NCT05668949
A Study of TTI-101 as Monotherapy and in Combination in Participants With Locally Advanced or Metastatic, and Unresectable Hepatocellular Carcinoma. https://ClinicalTrials.gov/show/NCT05440708
Study of TTI-101 in Combination for Participants With Metastatic Hormone Receptor-Positive and Human Epithelial Receptor 2 (HER2)-Negative Breast Cancer. https://ClinicalTrials.gov/show/NCT05384119
Phase 1 Study of OPB-31121 in Patients With Relapsed or Refractory Non-Hodgkin's Lymphoma or Multiple Myeloma. https://ClinicalTrials.gov/show/NCT00511082
Phase I/II Study of OPB-31121 in Patients With Progressive Hepatocellular Carcinoma. https://ClinicalTrials.gov/show/NCT01406574
Study to Assess OPB-31121 in Advanced Leukemias or Myelodysplastic Syndromes. https://ClinicalTrials.gov/show/NCT01029509
IMX-110 in Patients With Advanced Solid Tumors. https://ClinicalTrials.gov/show/NCT03382340
Vidyarthi A, Khan N, Agnihotri T et al (2018) TLR-3 stimulation skews M2 macrophages to M1 through IFN-alphabeta signaling and restricts tumor progression. Front Immunol 9:1650. https://doi.org/10.3389/fimmu.2018.01650
Le Mercier I, Poujol D, Sanlaville A et al (2013) Tumor promotion by intratumoral plasmacytoid dendritic cells is reversed by TLR7 ligand treatment. Cancer Res 73:4629–4640. https://doi.org/10.1158/0008-5472.CAN-12-3058
Mullins SR, Vasilakos JP, Deschler K et al (2019) Intratumoral immunotherapy with TLR7/8 agonist MEDI9197 modulates the tumor microenvironment leading to enhanced activity when combined with other immunotherapies. J Immunother Cancer 7:244. https://doi.org/10.1186/s40425-019-0724-8
Singh M, Khong H, Dai Z, Huang XF, Wargo JA, Cooper ZA, Vasilakos JP, Hwu P, Overwijk WW (2014) Effective innate and adaptive antimelanoma immunity through localized TLR7/8 activation. J Immunol 193:4722–4731. https://doi.org/10.4049/jimmunol.1401160
Hagström J, Heikkilä A, Siironen P, Louhimo J, Heiskanen I, Mäenpää H, Arola J, Haglund C (2012) TLR-4 expression and decrease in chronic inflammation: indicators of aggressive follicular thyroid carcinoma. J Clin Pathol 65:333–338. https://doi.org/10.1136/jclinpath-2011-200402
Peyret V, Nazar M, Martín M et al (2018) Functional toll-like receptor 4 overexpression in papillary thyroid cancer by MAPK/ERK-induced ETS1 transcriptional activity. Mol Cancer Res 16:833–845. https://doi.org/10.1158/1541-7786.MCR-17-0433
A Study of DSP-0509 in Patients With Advanced Solid Tumors to Determine the Safety and the Pharmacokinetic Profile. https://ClinicalTrials.gov/show/NCT03416335
Safety, Pharmacokinetics, Pharmacodynamics, and Preliminary Efficacy Trial of BNT411. https://ClinicalTrials.gov/show/NCT04101357
A First-in-human Study Using BDC-1001 as a Single Agent and in Combination With Nivolumab in Advanced HER2-Expressing Solid Tumors. https://ClinicalTrials.gov/show/NCT04278144
Clinical Study of BDB018: Monotherapy and in Combination With Pembrolizumab in Subjects With Advanced Solid Tumors. https://ClinicalTrials.gov/show/NCT04840394
Pressure Enabled Delivery of SD-101 With Checkpoint Blockade for Primary Liver Tumors. https://ClinicalTrials.gov/show/NCT05220722
Pressure Enabled Intrapancreatic Delivery of SD-101 With Checkpoint Blockade for Locally Advanced Pancreatic Adenocarcinoma. https://ClinicalTrials.gov/show/NCT05607953
TLR9 Agonist SD-101, Ibrutinib, and Radiation Therapy in Treating Patients With Relapsed or Refractory Grade 1-3A Follicular Lymphoma. https://ClinicalTrials.gov/show/NCT02927964
CMP-001 and Pre-operative Stereotactic Body Radiation Therapy (SBRT) in Early Stage Triple Negative Breast Cancer (TNBC). https://ClinicalTrials.gov/show/NCT04807192
CMP-001 for Relapsed and Refractory Lymphoma. https://ClinicalTrials.gov/show/NCT03983668
CMP-001 in Combination With IV PD-1-Blocking Antibody in Subjects With Certain Types of Advanced or Metastatic Cancer. https://ClinicalTrials.gov/show/NCT04916002
Intratumoral Tilsotolimod, a TLR-9 Agonist, Together With Intratumoral Ipilimumab and Intravenous Nivolumab in Patients With Advanced Cancers. https://ClinicalTrials.gov/show/NCT04270864
A Randomized Controlled Phase II Trial With Intradermal IMO-2125 in Pathological Tumor Stage (p) T3-4 cN0M0 Melanoma. https://ClinicalTrials.gov/show/NCT04126876
Study of Tilsotolimod in Combination With Nivolumab and Ipilimumab for the Treatment of Solid Tumors (ILLUMINATE-206). https://ClinicalTrials.gov/show/NCT03865082
Jiang K, Song C, Kong L et al (2018) Recombinant oncolytic Newcastle disease virus displays antitumor activities in anaplastic thyroid cancer cells. BMC Cancer 18:746. https://doi.org/10.1186/s12885-018-4522-3
Banerjee S, Halder K, Ghosh S, Bose A, Majumdar S (2015) The combination of a novel immunomodulator with a regulatory T cell suppressing antibody (DTA-1) regress advanced stage B16F10 solid tumor by repolarizing tumor associated macrophages in situ. Oncoimmunology 4:e995559. https://doi.org/10.1080/2162402X.2014.995559
Kumar P, Tyagi R, Das G, Bhaskar S (2014) Mycobacterium indicus pranii and Mycobacterium bovis BCG lead to differential macrophage activation in Toll-like receptor-dependent manner. Immunology 143:258–268. https://doi.org/10.1111/imm.12306
Mardente S, Aventaggiato M, Splendiani E, Mari E, Zicari A, Catanzaro G, Po A, Coppola L, Tafani M (2023) Extra-cellular vesicles derived from thyroid cancer cells promote the epithelial to mesenchymal transition (EMT) and the transfer of malignant phenotypes through immune mediated mechanisms. Int J Mol Sci 24:1. https://doi.org/10.3390/ijms24032754
Bravo-Miana RdC, Soler MF, Ceschin DG et al (2022) Extracellular vesicles from thyroid cancer harbor a functional machinery involved in extracellular matrix remodeling. Eur J Cell Biol 101:151254. https://doi.org/10.1016/j.ejcb.2022.151254
Cai J, Qiao B, Gao N, Lin N, He W (2019) Oral squamous cell carcinoma-derived exosomes promote M2 subtype macrophage polarization mediated by exosome-enclosed miR-29a-3p. Am J Physiol Cell Physiol 316:C731–C740. https://doi.org/10.1152/ajpcell.00366.2018
Hsu YL, Hung JY, Chang WA, Jian SF, Lin YS, Pan YC, Wu CY, Kuo PL (2018) Hypoxic lung-cancer-derived extracellular vesicle microRNA-103a increases the oncogenic effects of macrophages by targeting PTEN. Mol Ther 26:568–581. https://doi.org/10.1016/j.ymthe.2017.11.016
Takano Y, Masuda T, Iinuma H et al (2017) Circulating exosomal microRNA-203 is associated with metastasis possibly via inducing tumor-associated macrophages in colorectal cancer. Oncotarget 8:78598–78613. https://doi.org/10.18632/oncotarget.20009
Chen X, Ying X, Wang X, Wu X, Zhu Q (2017) Exosomes derived from hypoxic epithelial ovarian cancer deliver microRNA-940 to induce macrophage M2 polarization. Oncol Rep 38:522–528. https://doi.org/10.3892/or.2017.5697
Thulin P, Wei T, Werngren O, Cheung L, Fisher RM, Grandér D, Corcoran M, Ehrenborg E (2013) MicroRNA-9 regulates the expression of peroxisome proliferator-activated receptor δ in human monocytes during the inflammatory response. Int J Mol Med 31:1003–1010. https://doi.org/10.3892/ijmm.2013.1311
Jang JY, Lee JK, Jeon YK, Kim CW (2013) Exosome derived from epigallocatechin gallate treated breast cancer cells suppresses tumor growth by inhibiting tumor-associated macrophage infiltration and M2 polarization. BMC Cancer 13:421. https://doi.org/10.1186/1471-2407-13-421
Shao Y, Chen T, Zheng X et al (2018) Colorectal cancer-derived small extracellular vesicles establish an inflammatory premetastatic niche in liver metastasis. Carcinogenesis 39:1368–1379. https://doi.org/10.1093/carcin/bgy115
Ying H, Kang Y, Zhang H, Zhao D, Xia J, Lu Z, Wang H, Xu F, Shi L (2015) MiR-127 modulates macrophage polarization and promotes lung inflammation and injury by activating the JNK pathway. J Immunol 194:1239–1251. https://doi.org/10.4049/jimmunol.1402088
Su MJ, Aldawsari H, Amiji M (2016) Pancreatic cancer cell exosome-mediated macrophage reprogramming and the role of microRNAs 155 and 125b2 transfection using nanoparticle delivery systems. Sci Rep 6:30110. https://doi.org/10.1038/srep30110
Trivedi M, Talekar M, Shah P, Ouyang Q, Amiji M (2016) Modification of tumor cell exosome content by transfection with wt-p53 and microRNA-125b expressing plasmid DNA and its effect on macrophage polarization. Oncogenesis 5:e250. https://doi.org/10.1038/oncsis.2016.52
Williams C, Royo F, Aizpurua-Olaizola O, Pazos R, Boons GJ, Reichardt NC, Falcon-Perez JM (2018) Glycosylation of extracellular vesicles: current knowledge, tools and clinical perspectives. J Extracell Vesicles 7:1442985. https://doi.org/10.1080/20013078.2018.1442985
Gerlach JQ, Griffin MD (2016) Getting to know the extracellular vesicle glycome. Mol Biosyst 12:1071–1081. https://doi.org/10.1039/c5mb00835b
Choo YW, Kang M, Kim HY et al (2018) M1 macrophage-derived nanovesicles potentiate the anticancer efficacy of immune checkpoint inhibitors. ACS Nano 12:8977–8993. https://doi.org/10.1021/acsnano.8b02446
Luo H, Zhang H, Mao J et al (2023) Exosome-based nanoimmunotherapy targeting TAMs, a promising strategy for glioma. Cell Death Dis 14:235. https://doi.org/10.1038/s41419-023-05753-9
Lee JC, Zhao JT, Gundara J et al (2015) Papillary thyroid cancer-derived exosomes contain miRNA-146b and miRNA-222. J Surg Res 196(1):39–48. https://doi.org/10.1016/j.jss.2015.02.027
Jiang K, Li G, Chen W et al (2020) Plasma exosomal miR-146b-5p and miR-222-3p are potential biomarkers for lymph node metastasis in papillary thyroid carcinomas. Oncol Targets Ther 13:1311–1319. https://doi.org/10.2147/OTT.S231361
Pan Q, Zhao J, Li M, Liu X, Xu Y, Li W, Wu S, Su Z (2020) Exosomal miRNAs are potential diagnostic biomarkers between malignant and benign thyroid nodules based on next-generation sequencing. Carcinogenesis 41:18–24. https://doi.org/10.1093/carcin/bgz160
Liang M, Yu S, Tang S et al (2020) A panel of plasma exosomal miRNAs as potential biomarkers for differential diagnosis of thyroid nodules. Front Genet 11:449. https://doi.org/10.3389/fgene.2020.00449
Han S, Wang W, Wang S et al (2021) Tumor microenvironment remodeling and tumor therapy based on M2-like tumor associated macrophage-targeting nano-complexes. Theranostics 11:2892–2916. https://doi.org/10.7150/thno.50928
Niu M, Naguib YW, Aldayel AM, Shi Y-c, Hursting SD, Hersh MA, Cui Z (2014) Biodistribution and in vivo activities of tumor-associated macrophage-targeting nanoparticles incorporated with doxorubicin. Mol Pharm 11:4425–4436. https://doi.org/10.1021/mp500565q
Cao M, Yan H, Han X et al (2019) Ginseng-derived nanoparticles alter macrophage polarization to inhibit melanoma growth. J Immunother Cancer 7:326. https://doi.org/10.1186/s40425-019-0817-4
Deng G, Sun Z, Li S, Peng X, Li W, Zhou L, Ma Y, Gong P, Cai L (2018) Cell-membrane immunotherapy based on natural killer cell membrane coated nanoparticles for the effective inhibition of primary and abscopal tumor growth. ACS Nano 12:12096–12108. https://doi.org/10.1021/acsnano.8b05292
Su L, Zhang W, Wu X, Zhang Y, Chen X, Liu G, Chen G, Jiang M (2015) Glycocalyx-mimicking nanoparticles for stimulation and polarization of macrophages via specific interactions. Small 11:4191–4200. https://doi.org/10.1002/smll.201403838
Habanjar O, Bingula R, Decombat C, Diab-Assaf M, Caldefie-Chezet F, Delort L (2023) Crosstalk of inflammatory cytokines within the breast tumor microenvironment. Int J Mol Sci 24:1. https://doi.org/10.3390/ijms24044002
Wang Y, Lin YX, Qiao SL, An HW, Ma Y, Qiao ZY, Rajapaksha RP, Wang H (2017) Polymeric nanoparticles promote macrophage reversal from M2 to M1 phenotypes in the tumor microenvironment. Biomaterials 112:153–163. https://doi.org/10.1016/j.biomaterials.2016.09.034
He XY, Liu BY, Xu C, Zhuo RX, Cheng SX (2018) A multi-functional macrophage and tumor targeting gene delivery system for the regulation of macrophage polarity and reversal of cancer immunoresistance. Nanoscale 10:15578–15587. https://doi.org/10.1039/c8nr05294h
Kulkarni A, Chandrasekar V, Natarajan SK et al (2018) A designer self-assembled supramolecule amplifies macrophage immune responses against aggressive cancer. Nat Biomed Eng 2:589–599. https://doi.org/10.1038/s41551-018-0254-6
Nilubol N, Yuan Z, Paciotti GF et al (2018) Novel dual-action targeted nanomedicine in mice with metastatic thyroid cancer and pancreatic neuroendocrine tumors. J Natl Cancer Inst 110:1019–1029. https://doi.org/10.1093/jnci/djy003
Liu F, Ma D, Chen W et al (2019) Gold nanoparticles suppressed proliferation, migration, and invasion in papillary thyroid carcinoma cells via downregulation of CCT3. J Nanomater 2012:1. https://doi.org/10.1155/2019/1687340
Willingham SB, Volkmer JP, Gentles AJ et al (2012) The CD47-signal regulatory protein alpha (SIRPa) interaction is a therapeutic target for human solid tumors. Proc Natl Acad Sci USA 109:6662–6667. https://doi.org/10.1073/pnas.1121623109
Weiskopf K, Jahchan NS, Schnorr PJ et al (2016) CD47-blocking immunotherapies stimulate macrophage-mediated destruction of small-cell lung cancer. J Clin Investig 126:2610–2620
Liu R, Wei H, Gao P et al (2017) CD47 promotes ovarian cancer progression by inhibiting macrophage phagocytosis. Oncotarget 8:39021
Ansell SM, Maris MB, Lesokhin AM et al (2021) Phase I study of the CD47 blocker TTI-621 in patients with relapsed or refractory hematologic malignancies. Clin Cancer Res 27:2190–2199. https://doi.org/10.1158/1078-0432.CCR-20-3706
Barkal AA, Weiskopf K, Kao KS et al (2018) Engagement of MHC class I by the inhibitory receptor LILRB1 suppresses macrophages and is a target of cancer immunotherapy. Nat Immunol 19:76–84
Cercek A, Lumish M, Sinopoli J et al (2022) PD-1 blockade in mismatch repair-deficient, locally advanced rectal cancer. N Engl J Med 386:2363–2376. https://doi.org/10.1056/NEJMoa2201445
Janjigian YY, Kawazoe A, Yanez P et al (2021) The KEYNOTE-811 trial of dual PD-1 and HER2 blockade in HER2-positive gastric cancer. Nature 600:727–730. https://doi.org/10.1038/s41586-021-04161-3
Cho BC, Abreu DR, Hussein M et al (2022) Tiragolumab plus atezolizumab versus placebo plus atezolizumab as a first-line treatment for PD-L1-selected non-small-cell lung cancer (CITYSCAPE): primary and follow-up analyses of a randomised, double-blind, phase 2 study. Lancet Oncol 23:781–792. https://doi.org/10.1016/S1470-2045(22)00226-1
Liu Y, Zugazagoitia J, Ahmed FS, Henick BS, Gettinger SN, Herbst RS, Schalper KA, Rimm DL (2020) Immune cell PD-L1 colocalizes with macrophages and is associated with outcome in PD-1 pathway blockade therapy. Clin Cancer Res 26:970–977. https://doi.org/10.1158/1078-0432.CCR-19-1040
Gordon SR, Maute RL, Dulken BW et al (2017) PD-1 expression by tumour-associated macrophages inhibits phagocytosis and tumour immunity. Nature 545:495–499. https://doi.org/10.1038/nature22396
Gunda V, Gigliotti B, Ndishabandi D et al (2018) Combinations of BRAF inhibitor and anti-PD-1/PD-L1 antibody improve survival and tumour immunity in an immunocompetent model of orthotopic murine anaplastic thyroid cancer. Br J Cancer 119:1223–1232. https://doi.org/10.1038/s41416-018-0296-2
Dhupkar P, Gordon N, Stewart J, Kleinerman ES (2018) Anti-PD-1 therapy redirects macrophages from an M2 to an M1 phenotype inducing regression of OS lung metastases. Cancer Med 7:2654–2664. https://doi.org/10.1002/cam4.1518
Li Z, Ding Y, Liu J et al (2022) Depletion of tumor associated macrophages enhances local and systemic platelet-mediated anti-PD-1 delivery for post-surgery tumor recurrence treatment. Nat Commun 13:1845. https://doi.org/10.1038/s41467-022-29388-0
Mehnert JM, Varga A, Brose MS et al (2019) Safety and antitumor activity of the anti-PD-1 antibody pembrolizumab in patients with advanced, PD-L1-positive papillary or follicular thyroid cancer. BMC Cancer 19:196. https://doi.org/10.1186/s12885-019-5380-3
Sakamuri D, Glitza IC, Betancourt Cuellar SL et al (2018) Phase I dose-escalation study of anti-CTLA-4 antibody ipilimumab and lenalidomide in patients with advanced cancers. Mol Cancer Ther 17:671–676. https://doi.org/10.1158/1535-7163.MCT-17-0673
Vudalimab for the Treatment of Locally Advanced or Metastatic Anaplastic Thyroid Cancer or Hurthle Cell Thyroid Cancer. https://ClinicalTrials.gov/show/NCT05453799
Testing the Combination of Cabozantinib, Nivolumab, and Ipilimumab (CaboNivoIpi) for Advanced Differentiated Thyroid Cancer. https://ClinicalTrials.gov/show/NCT03914300
Cunha LL, Marcello MA, Ward LS (2014) The role of the inflammatory microenvironment in thyroid carcinogenesis. Endocr Relat Cancer 21:R85–R103. https://doi.org/10.1530/ERC-13-0431
Luo T, Sun J, Zhu S et al (2017) Ultrasound-mediated destruction of oxygen and paclitaxel loaded dual-targeting microbubbles for intraperitoneal treatment of ovarian cancer xenografts. Cancer Lett 391:1–11. https://doi.org/10.1016/j.canlet.2016.12.032
Gunassekaran GR, Poongkavithai Vadevoo SM, Baek MC, Lee B (2021) M1 macrophage exosomes engineered to foster M1 polarization and target the IL-4 receptor inhibit tumor growth by reprogramming tumor-associated macrophages into M1-like macrophages. Biomaterials 278:121137. https://doi.org/10.1016/j.biomaterials.2021.121137
Zhang W, Zhu XD, Sun HC et al (2010) Depletion of tumor-associated macrophages enhances the effect of sorafenib in metastatic liver cancer models by antimetastatic and antiangiogenic effects. Clin Cancer Res 16:3420–3430. https://doi.org/10.1158/1078-0432.CCR-09-2904
Lorusso L, Pieruzzi L, Gabriele M, Nisi M, Viola D, Molinaro E, Bottici V, Elisei R, Agate L (2021) Osteonecrosis of the jaw: a rare but possible side effect in thyroid cancer patients treated with tyrosine-kinase inhibitors and bisphosphonates. J Endocrinol Invest 44:2557–2566. https://doi.org/10.1007/s40618-021-01634-0
Beuselinck B, Wolter P, Karadimou A et al (2012) Concomitant oral tyrosine kinase inhibitors and bisphosphonates in advanced renal cell carcinoma with bone metastases. Br J Cancer 107:1665–1671. https://doi.org/10.1038/bjc.2012.385
Gralow JR, Barlow WE, Paterson AHG et al (2020) Phase III randomized trial of bisphosphonates as adjuvant therapy in breast cancer: S0307. J Natl Cancer Inst 112:698–707. https://doi.org/10.1093/jnci/djz215
Gainford MC, Dranitsaris G, Ooi W, Vanhuyse M, Clemons M (2006) Comparing the results of bisphosphonate use in clinical trials with actual practice: a case of apples and oranges? Curr Oncol 13:187–190
Zylberberg HM, Rustgi SD, Yang A, Aronson A, Kessel E, Amin S, Lucas AL (2021) Bisphosphonate use does not impact survival in patients with pancreatic cancer: a propensity score matching analysis. Gut Liver 15:782–790. https://doi.org/10.5009/gnl20297
Guerriero JL (2019) Macrophages: their untold story in T cell activation and function. Int Rev Cell Mol Biol 342:73–93. https://doi.org/10.1016/bs.ircmb.2018.07.001
Wang Y, Johnson KCC, Gatti-Mays ME, Li Z (2022) Emerging strategies in targeting tumor-resident myeloid cells for cancer immunotherapy. J Hematol Oncol 15:118. https://doi.org/10.1186/s13045-022-01335-y
Krieg C, Nowicka M, Guglietta S et al (2018) High-dimensional single-cell analysis predicts response to anti-PD-1 immunotherapy. Nat Med 24:144–153. https://doi.org/10.1038/nm.4466
Romano E, Kusio-Kobialka M, Foukas PG et al (2015) Ipilimumab-dependent cell-mediated cytotoxicity of regulatory T cells ex vivo by nonclassical monocytes in melanoma patients. Proc Natl Acad Sci USA 112:6140–6145. https://doi.org/10.1073/pnas.1417320112
La Fleur L, Botling J, He F et al (2021) Targeting MARCO and IL37R on immunosuppressive macrophages in lung cancer blocks regulatory T cells and supports cytotoxic lymphocyte function. Cancer Res 81:956–967. https://doi.org/10.1158/0008-5472.CAN-20-1885
Nakamura K, Smyth MJ (2020) TREM2 marks tumor-associated macrophages. Signal Transduct Target Ther 5:233. https://doi.org/10.1038/s41392-020-00356-8
Li PH, Kong XY, He YZ, Liu Y, Peng X, Li ZH, Xu H, Luo H, Park J (2022) Recent developments in application of single-cell RNA sequencing in the tumour immune microenvironment and cancer therapy. Mil Med Res 9:52. https://doi.org/10.1186/s40779-022-00414-y
Azizi E, Carr AJ, Plitas G et al (2018) Single-cell map of diverse immune phenotypes in the breast tumor microenvironment. Cell 174:1293–308.e36. https://doi.org/10.1016/j.cell.2018.05.060
Hirz T, Mei S, Sarkar H et al (2023) Dissecting the immune suppressive human prostate tumor microenvironment via integrated single-cell and spatial transcriptomic analyses. Nat Commun 14:663. https://doi.org/10.1038/s41467-023-36325-2
Schepisi G, Gianni C, Palleschi M, Bleve S, Casadei C, Lolli C, Ridolfi L, Martinelli G, De Giorgi U (2023) The new frontier of immunotherapy: chimeric antigen receptor T (CAR-T) cell and macrophage (CAR-M) therapy against breast cancer. Cancers (Basel) 15:1. https://doi.org/10.3390/cancers15051597
CAR-macrophages for the Treatment of HER2 Overexpressing Solid Tumors. https://ClinicalTrials.gov/show/NCT04660929
Cohort Study to Determine the Antitumor Activity of New CAR-macrophages in Breast Cancer Patients' Derived Organoids. https://ClinicalTrials.gov/show/NCT05007379
Reyes-García J, Montaño LM, Carbajal-García A, Wang YX (2021) Sex hormones and lung inflammation. Adv Exp Med Biol 1304:259–321. https://doi.org/10.1007/978-3-030-68748-9_15
Becerra-Díaz M, Lerner AD, Yu DH, Thiboutot JP, Liu MC, Yarmus LB, Bose S, Heller NM (2021) Sex differences in M2 polarization, chemokine and IL-4 receptors in monocytes and macrophages from asthmatics. Cell Immunol 360:104252. https://doi.org/10.1016/j.cellimm.2020.104252
Keselman A, Fang X, White PB, Heller NM (2017) Estrogen signaling contributes to sex differences in macrophage polarization during asthma. J Immunol 199:1573–1583. https://doi.org/10.4049/jimmunol.1601975
Adachi A, Honda T, Egawa G et al (2022) Estradiol suppresses psoriatic inflammation in mice by regulating neutrophil and macrophage functions. J Allergy Clin Immunol 150:909–19.e8. https://doi.org/10.1016/j.jaci.2022.03.028
Becerra-Díaz M, Strickland AB, Keselman A, Heller NM (2018) Androgen and androgen receptor as enhancers of M2 macrophage polarization in allergic lung inflammation. J Immunol 201:2923–2933. https://doi.org/10.4049/jimmunol.1800352
Chae YK, Othus M, Patel S et al (2020) 270 A phase II basket trial of dual anti-CTLA-4 and anti-PD-1 blockade in rare tumors (DART) SWOG S1609: the thyroid tumor cohort. J Immunother Cancer 8:A161. https://doi.org/10.1136/jitc-2020-SITC2020.0270
Acknowledgements
Not applicable.
Funding
This work was supported by the National Research Foundation of Korea (NRF) grant funded by the Korea government (MSIT), Grant/Award Number: NRF-2022R1A2C2005057.
Author information
Authors and Affiliations
Contributions
In this paper, B-CA and XJL planned the project and the main conceptual ideas. LZ drafted the initial draft of the manuscript and designed the figures. PG and XJ contributed significantly to the modification and discussion of the manuscript. All authors have approved the final version of the manuscript.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Zhu, L., Li, X.J., Gangadaran, P. et al. Tumor-associated macrophages as a potential therapeutic target in thyroid cancers. Cancer Immunol Immunother 72, 3895–3917 (2023). https://doi.org/10.1007/s00262-023-03549-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00262-023-03549-6