Abstract
Purpose
This study aimed to explore the value of dynamic magnetic resonance imaging (MRI) before and after operation for pelvic organ prolapse (POP).
Methods
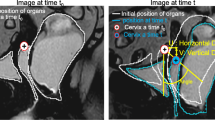
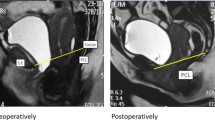
Twenty-nine patients with POP (POP group) before and one month after surgery and 12 healthy women (control group) underwent static and dynamic MRI at rest and during straining (Valsalva maneuver). The preoperative MRI images of the POP and control groups were analyzed, and various measurements were recorded. Differences in measurements were compared between the POP and control groups; similarly, changes in measurements before and after operation were compared.
Results
In the POP group, MRI detected 29 anterior vaginal prolapses, 27 uterine prolapses, 1 rectoceles, and 14 pouch of Douglas hernias. In addition, 27 levator ani muscle defect and 15 pubocervical fascial defect cases were observed. The bladder-pubococcygeal line (B-PCL), uterus-pubococcygeal line (U-PCL), Douglas pouch-pubococcygeal line, the length of the hiatus, the descent of the levator plate, levator hiatus size, levator plate angle, iliococcygeus angle, and urethral inclination angle (UA) were larger in the POP group than in the control group. The pelvic organs’ positions returned to normal postoperatively in 9 of 21 cases. The B-PCL, U-PCL, and UA were smaller post-surgery than pre-surgery.
Conclusions
Static and dynamic MRI can comprehensively evaluate morphological and functional changes of the pelvic floor postoperatively.





Similar content being viewed by others
Data availability
The datasets used or analyzed during the current study are available from the corresponding author on reasonable request.
References
Bradley CS (2018) Progress toward understanding pelvic organ prolapse. Am J Obstet Gynecol 218:267-268. doi: https://doi.org/10.1016/j.ajog.2018.01.042
Huang L, Zhao Z, Wen J, Ling W, Miao Y, Wu J (2020) Cellular senescence: A pathogenic mechanism of pelvic organ prolapse (Review). Mol Med Rep 22:2155-2162. doi: https://doi.org/10.3892/mmr.2020.11339
Iglesia CB, Smithling KR (2017) Pelvic Organ Prolapse. Am Fam Physician 96:179-185
Haylen BT, Maher CF, Barber MD, Camargo S, Dandolu V, Digesu A, Goldman HB, Huser M, Milani AL, Moran PA, Schaer GN, Withagen MI (2016) An International Urogynecological Association (IUGA) / International Continence Society (ICS) Joint Report on the Terminology for Female Pelvic Organ Prolapse (POP). Neurourol Urodyn 35:137-168. doi: https://doi.org/10.1002/nau.22922
Easley DC, Abramowitch SD, Moalli PA (2017) Female pelvic floor biomechanics: bridging the gap. Curr Opin Urol 27:262-267. doi: https://doi.org/10.1097/MOU.0000000000000380
Pannu HK, Javitt MC, Glanc P, Bhosale PR, Harisinghani MG, Khati NJ, Mitchell DG, Nyberg DA, Pandharipande PV, Shipp TD, Siegel CL, Simpson L, Wall DJ, Wong-You-Cheong JJ (2015) ACR Appropriateness Criteria pelvic floor dysfunction. J Am Coll Radiol 12:134-142. doi: https://doi.org/10.1016/j.jacr.2014.10.021
Salvador JC, Coutinho MP, Venâncio JM, Viamonte B (2019) Dynamic magnetic resonance imaging of the female pelvic floor-a pictorial review. Insights Imaging 10:4. doi: https://doi.org/10.1186/s13244-019-0687-9
El Sayed RF, Alt CD, Maccioni F, Meissnitzer M, Masselli G, Manganaro L, Vinci V, Weishaupt D; ESUR and ESGAR Pelvic Floor Working Group (2017) Magnetic resonance imaging of pelvic floor dysfunction - joint recommendations of the ESUR and ESGAR Pelvic Floor Working Group. Eur Radiol 27:2067-2085. doi: https://doi.org/10.1007/s00330-016-4471-7
Maccioni F, Al Ansari N, Buonocore V, Mazzamurro F, Indinnimeo M, Mongardini M, Catalano C (2016) Prospective Comparison between two different magnetic resonance defecography techniques for evaluating pelvic floor disorders: air-balloon versus gel for rectal filling. Eur Radiol 26:1783-1791. doi: https://doi.org/10.1007/s00330-015-4016-5
Kobi M, Flusberg M, Paroder V, Chernyak V (2018) Practical guide to dynamic pelvic floor MRI. J Magn Reson Imaging 47:1155-1170. doi: https://doi.org/10.1002/jmri.25998
Reiner CS, Weishaupt D (2013) Dynamic pelvic floor imaging: MRI techniques and imaging parameters. Abdom Imaging 38:903-911. doi: https://doi.org/10.1007/s00261-012-9857-7
El-Haieg DO, Madkour NM, Basha MAA, Ahmad RA, Sadek SM, Al-Molla RM, Tantwy EF, Almassry HN, Altaher KM, Mahmoud NEM, Aly SA (2019) Magnetic resonance imaging and 3-dimensional transperineal ultrasound evaluation of pelvic floor dysfunction in symptomatic women: a prospective comparative study. Ultrasonography 38:355-364. doi: https://doi.org/10.14366/usg.19007
Hsu Y, Summers A, Hussain HK, Guire KE, Delancey JO (2006) Levator plate angle in women with pelvic organ prolapse compared to women with normal support using dynamic MR imaging. Am J Obstet Gynecol 194:1427-1433. doi: https://doi.org/10.1016/j.ajog.2006.01.055
Ansquer Y, Fernandez P, Chapron C, Frey C, Bennis M, Roy C, Salomon L, Mandelbrot L, Carbonne B (2006) Static and dynamic MRI features of the levator ani and correlation with severity of genital prolapse. Acta Obstet Gynecol Scand 85:1468-1475. doi: https://doi.org/10.1080/00016340600984837
Li M, Wang B, Liu X, Qiao P, Jiao W, Jiang T (2020) MR defecography in the assessment of anatomic and functional abnormalities in stress urinary incontinence before and after pelvic reconstruction. Eur J Radiol 126:108935. doi: https://doi.org/10.1016/j.ejrad.2020.108935
Krofta L, Havelková L, Urbánková I, Krčmář M, Hynčík L, Feyereisl J (2017) Finite element model focused on stress distribution in the levator ani muscle during vaginal delivery. Int Urogynecol J 28:275-284. doi: https://doi.org/10.1007/s00192-016-3126-1
Lamblin G, Delorme E, Cosson M, Rubod C (2016) Cystocele and functional anatomy of the pelvic floor: review and update of the various theories. Int Urogynecol J 27:1297-1305. doi: https://doi.org/10.1007/s00192-015-2832-4
Li JR, Lei L, Luo N, Chen N, Xu HT, Xin Hu, Song Y, Wu Y (2021) Architecture of female urethral supporting structures based on undeformed high-resolution sectional anatomical images. Anat Sci Int 96:30-41. doi: https://doi.org/10.1007/s12565-020-00554-y
García del Salto L, de Miguel Criado J, Aguilera del Hoyo LF, Gutiérrez Velasco L, Fraga Rivas P, Manzano Paradela M, Díez Pérez de las Vacas MI, Marco Sanz AG, Fraile Moreno E (2014) MR imaging-based assessment of the female pelvic floor. Radiographics 34:1417-1439. doi: https://doi.org/10.1148/rg.345140137
Schmid FA, Gomolka RS, Hötker AM, Boss A, Kessler TM, Rossi C, Eberli D (2020) Evaluation of Urinary Sphincter Function by Rapid Magnetic Resonance Diffusion Tensor Imaging. Int Neurourol J 24:349-357. doi: https://doi.org/10.5213/inj.2040208.104
Picchia S, Rengo M, Bellini D, Caruso D, Pironti E, Floris R, Laghi A (2019) Dynamic MR of the pelvic floor: Influence of alternative methods to draw the pubococcygeal line (PCL) on the grading of pelvic floor descent. Eur J Radiol Open 6:187-191. doi: https://doi.org/10.1016/j.ejro.2019.05.002
Su D, Wen Y, Lin Q (2021) Particle Swarm Algorithm-Based Analysis of Pelvic Dynamic MRI Images in Female Stress Urinary Incontinence. Contrast Media Mol Imaging 2021:8233511. doi: https://doi.org/10.1155/2021/8233511
Li N, Cui C, Cheng Y, Wu Y, Yin J, Shen W (2018) Association between Magnetic Resonance Imaging Findings of the Pelvic Floor and de novo Stress Urinary Incontinence after Vaginal Delivery. Korean J Radiol 19:715-723. doi: https://doi.org/10.3348/kjr.2018.19.4.715
Handa VL, Roem J, Blomquist JL, Dietz HP, Muñoz A (2019) Pelvic organ prolapse as a function of levator ani avulsion, hiatus size, and strength. Am J Obstet Gynecol 221:41.e1-41.e7. doi: https://doi.org/10.1016/j.ajog.2019.03.004
Kasturi S, Lowman JK, Kelvin FM, Akisik FM, Terry CL, Hale DS (2010) Pelvic magnetic resonance imaging for assessment of the efficacy of the Prolift system for pelvic organ prolapse. Am J Obstet Gynecol 203:504.e1-504.e5. doi: https://doi.org/10.1016/j.ajog.2010.06.034
Mahfouz W, Elmissiry M, Gomaa SA, Koraitim A, Hassan H (2020) Evaluation of the effect of abdominal sacrocolpopexy (ASC) on urethral anatomy and continence mechanism using dynamic MRI. Int Urol Nephrol 52:1429-1435. doi: https://doi.org/10.1007/s11255-020-02444-8
Acknowledgements
None.
Funding
This research did not receive any funding.
Author information
Authors and Affiliations
Contributions
HZ participated in data collection, analysis, manuscript writing, and approval; ZW participated in project development, data collection, analysis, and approval; BZ participated in project development, data collection, analysis, manuscript writing and approval; XX participated in project development, data analysis; JW participated in analysis.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflicts of interest regarding this research.
Ethical approval
This manuscript has not been published or presented elsewhere in part or in entirety and is not under consideration by another journal. All study participants provided informed consent, and the study design was approved by the appropriate ethics review board.
Consent to participate and consent to publish
Informed consent was obtained from all individual participants included in the study. The authors affirm that the participants provided informed consent for publication of the images in Figs. 1, 2, 3, 4, and 5.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Zhang, H., Wang, Z., Xiao, X. et al. Dynamic magnetic resonance imaging evaluation before and after operation for pelvic organ prolapse. Abdom Radiol 47, 848–857 (2022). https://doi.org/10.1007/s00261-021-03361-9
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00261-021-03361-9