Abstract
Purpose
Clinical studies on the use of ascorbic acid (AA) have become a hot spot in cancer research. There remains an unmet need to assess AA utilization in normal tissues and tumors. 6-Deoxy-6-[18F]fluoro-L-ascorbic acid ([18F]DFA) displayed distinctive tumor localization and similar distribution as AA in mice. In this study, to evaluate the distribution, tumor detecting ability and radiation dosimetry of [18F]DFA in humans, we performed the first-in-human PET imaging study.
Methods
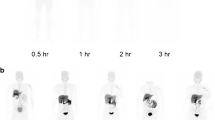
Six patients with a variety of cancers underwent whole-body PET/CT scans after injection of 313–634 MBq of [18F]DFA. Five sequential dynamic emission scans in each patient were acquired at 5–60 min. Regions of interest (ROI) were delineated along the edge of the source-organ and tumor on the transverse PET slice. Tumor-to-background ratio (TBR) was obtained using the tumor SUVmax to background SUVmean. Organ residence times were calculated via time-activity curves, and human absorbed doses were estimated from organ residence time using the medical internal radiation dosimetry method.
Results
[18F]DFA was well tolerated in all subjects without serious adverse event. The high uptake was found in the liver, adrenal glands, kidneys, choroid plexus, and pituitary gland. [18F]DFA accumulated in tumor rapidly and the TBR increased over time. The average SUVmax of [18F]DFA in tumor lesions was 6.94 ± 3.92 (range 1.62–22.85, median 5.94). The organs with the highest absorbed doses were the liver, spleen, adrenal glands, and kidneys. The mean effective dose was estimated to be 1.68 ± 0.36 E−02 mSv/MBq.
Conclusions
[18F]DFA is safe to be used in humans. It showed a similar distribution pattern as AA, and displayed high uptake and retention in tumors with appropriate kinetics. [18F]DFA might be a promising radiopharmaceutical in identifying tumors with high affinity for SVCT2 and monitoring AA distribution in both normal tissues and tumors.
Trial registration
Chinese Clinical Trial Registry; Registered Number: ChiCTR2200057842 (registered 19 March 2022).






Similar content being viewed by others
Data availability
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
Ngo B, Van Riper JM, Cantley LC, Yun J. Targeting cancer vulnerabilities with high-dose vitamin C. Nat Rev Cancer. 2019;19:271–82.
Böttger F, Vallés-Martí A, Cahn L, Jimenez CR. High-dose intravenous vitamin C, a promising multi-targeting agent in the treatment of cancer. J Exp Clin Cancer Res. 2021;40:343.
Iglesias J, Vassallo AV, Patel VV, Sullivan JB, Cavanaugh J, Elbaga Y. Outcomes of metabolic resuscitation using ascorbic acid, thiamine, and glucocorticoids in the early treatment of sepsis: the ORANGES trial. Chest. 2020;158:164–73.
Marik P.E. Hydrocortisone, ascorbic acid and thiamine (HAT therapy) for the treatment of sepsis. Focus on Ascorbic Acid. Nutrients. 2018;10:1762.
Islam MT. Angiostatic effects of ascorbic acid: current status and future perspectives. Angiogenesis. 2020;23:275–7.
van der Reest J, Gottlieb E. Anti-cancer effects of vitamin C revisited. Cell Res. 2016;26:269–70.
Darwiche W, Gomila C, Ouled-Haddou H, et al. Ascorbic acid (vitamin C) synergistically enhances the therapeutic effect of targeted therapy in chronic lymphocytic leukemia. J Exp Clin Cancer Res. 2020;39:228.
Reczek CR, Chandel NS. CANCER. Revisiting vitamin C and cancer. Science. 2015;350:1317-1318.
Shenoy N, Creagan E, Witzig T, Levine M. Ascorbic acid in cancer treatment: let the phoenix fly. Cancer Cell. 2018;34:700–6.
Lv H, Wang C, Fang T, et al. Vitamin C preferentially kills cancer stem cells in hepatocellular carcinoma via SVCT-2. NPJ Precis Oncol. 2018;2:1.
Roa FJ, Peña E, Gatica M, et al. Therapeutic use of vitamin c in cancer: physiological considerations. Front Pharmacol. 2020;11:211.
Hong SW, Lee SH, Moon JH, et al. SVCT-2 in breast cancer acts as an indicator for L-ascorbate treatment. Oncogene. 2013;32:1508–17.
Wang C, Lv H, Yang W, et al. SVCT-2 determines the sensitivity to ascorbate-induced cell death in cholangiocarcinoma cell lines and patient derived xenografts. Cancer Lett. 2017;398:1–11.
Ostriker AC, Xie Y, Chakraborty R, et al. TET2 protects against vascular smooth muscle cell apoptosis and intimal thickening in transplant vasculopathy. Circulation. 2021;144:455–70.
Miller PG, Ebert BL. Leukaemia: vitamin C regulates stem cells and cancer. Nature. 2017;549:462–4.
Blaschke K, Ebata KT, Karimi MM, et al. Vitamin C induces Tet-dependent DNA demethylation and a blastocyst-like state in ES cells. Nature. 2013;500:222–6.
Cheng H, Li L, Zhang M, et al. Recent advances on in vivo analysis of ascorbic acid in brain functions. Trac-Trend Anal Chem. 2018;109:247–59.
Yamamoto F, Kaneshiro T, Kato H, et al. Decreased tissue accumulation of 6-deoxy-6-[18F]fluoro-L-ascorbic acid in glutathione-deficient rats induced by administration of diethyl maleate. Biol Pharm Bull. 2005;28:1943–7.
He P, Zhang B, Zou Y, et al. Ascorbic acid analogue 6-Deoxy-6-[18F] fluoro-L-ascorbic acid as a tracer for identifying human colorectal cancer with SVCT2 overexpression. Transl Oncol. 2021;14: 101055.
Yamamoto F, Sasaki S, Maeda M. Positron labeled antioxidants: synthesis and tissue biodistribution of 6-deoxy-6-[18F]fluoro-L-ascorbic acid. Int J Rad Appl Instrum A. 1992;43:633–9.
Li Z, He P, Luo G, et al. Increased tumoral microenvironmental ph improves cytotoxic effect of pharmacologic ascorbic acid in castration-resistant prostate cancer cells. Front Pharmacol. 2020;11: 570939.
Yi C, Yu D, Shi X, He Q, Zhang X, Zhang X. Biodistribution and estimation of radiation-absorbed doses in humans for 13N-ammonia PET. Ann Nucl Med. 2015;29:810–5.
Hindorf C, Glatting G, Chiesa C, Lindén O, Flux G; EANM Dosimetry Committee. EANM Dosimetry Committee guidelines for bone marrow and whole-body dosimetry. Eur J Nucl Med Mol Imaging. 2010;37:1238–1250.
Laforest R, Ghai A, Fraum TJ, et al. First-in-human evaluation of safety and dosimetry of 64Cu-LLP2A for PET imaging. J Nucl Med. 2023;64:320–8.
Huang T, Wang H, Tang G, et al. Human radiation dose estimation of (11)C-CFT using whole-body PET. Clin Nucl Med. 2012;37:1159–62.
Stabin MG. MIRDOSE: personal computer software for internal dose assessment in nuclear medicine. J Nucl Med. 1996;37:538–46.
Cristy M, Eckerman KF. Specific absorbed fractions of energy at various ages from internal photon sources: VII—adult male. Oak Ridge National Laboratory; 1987. ORNL./TM-8381/V1.
Coffey JL, Watson EE. Calculating dose from remaining body activity: a comparison of two methods. Med Phys. 1979;6:307–8.
ICRP. 1990 recommendations of the International Commission on Radiological Protection: ICRP Publication 60. Ann ICRP. 1991;21:1–201.
Doseděl M, Jirkovský E, Macáková K, et al. Vitamin C-sources, physiological role, kinetics, deficiency, use, toxicity, and determination. Nutrients. 2021;13:615.
Lykkesfeldt J, Tveden-Nyborg P. The pharmacokinetics of vitamin C. Nutrients. 2019;11:2412.
Bürzle M, Suzuki Y, Ackermann D, et al. The sodium-dependent ascorbic acid transporter family SLC23. Mol Aspects Med. 2013;34:436–54.
Tsukaguchi H, Tokui T, Mackenzie B, et al. A family of mammalian Na+-dependent L-ascorbic acid transporters. Nature. 1999;399:70–5.
Linowiecka K, Foksinski M, Brożyna AA. Vitamin C transporters and their implications in carcinogenesis. Nutrients. 2020;12:3869.
Astuya A, Caprile T, Castro M, et al. Vitamin C uptake and recycling among normal and tumor cells from the central nervous system. J Neurosci Res. 2005;79:146–56.
May JM. Vitamin C transport and its role in the central nervous system. Subcell Biochem. 2012;56:85–103.
Hays MT, Watson EE, Thomas SR, Stabin M. MIRD dose estimate report no. 19: radiation absorbed dose estimates from (18)F-FDG. J Nucl Med. 2002;43:210–214.
Kim J, Yamamoto F, Kuwabara Y, et al. 6-[18F]fluoro-dehydroascorbic acid. Synthesis and tissue distribution in mice. Radioisotopes. 2009;58:47–55.
Yun J, Mullarky E, Lu C, et al. Vitamin C selectively kills KRAS and BRAF mutant colorectal cancer cells by targeting GAPDH. Science. 2015;350:1391–6.
Harding K, Thomson WH. Radiological protection and safety in medicine - ICRP 73. Eur J Nucl Med. 1997;24:1207–9.
Acknowledgements
We extend our profound appreciation to Professor Ganghua Tang for his generous contribution of the S value tables and the volunteers who participated in the imaging study.
Funding
This study was supported by the Natural Science Foundation of Guangdong province (no. 2022A1515011670) and the Key Research and Development Program of Guangzhou City (no. 202206010046).
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. YLL participated in the design of the study, collected the patients’ data, and drafted the manuscript. CY and RBW performed the material preparation, data collection, and analysis. YYZ, BZ, and XCS processed the figures and performed a critical revision of the manuscript. ZHZ and XSZ conceived and designed the study and supervised the project. All authors read and approved the final version of the manuscript.
Corresponding authors
Ethics declarations
Ethics approval
The current study was approved by the Institutional Ethics Committee of the First Affiliated Hospital of Sun Yat-Sen University (The ethical approval number is [2021]751-1).
Consent to participate
Informed consent was obtained from all individual participants included in the study.
Consent for publication
The authors affirm that all individual participants provided informed consent for anonymised evaluation and publication of their data.
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Long, Y., Yi, C., Wu, R. et al. Biodistribution and radiation dosimetry in cancer patients of the ascorbic acid analogue 6-Deoxy-6-[18F] fluoro-L-ascorbic acid PET imaging: first-in-human study. Eur J Nucl Med Mol Imaging 50, 3072–3083 (2023). https://doi.org/10.1007/s00259-023-06262-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00259-023-06262-9