Abstract
Background
Pectus excavatum is the most common congenital deformity of the chest, with a frequency of one in 300 to 500 births. Twenty-five percent of pectus excavatum patients are female. Different surgical methods are used to treat female patients, depending on the degree of their thorax’s deformity. For patients with mild deformity, fat transfer alone is often used to augment their breasts and improve appearance. This study aims to evaluate the thickness of the subdermal fat of adult female patients with pectus excavatum.
Methods
The thickness of subdermal fat of the central regions of the chest was measured by referring to computer tomographic data of 62 adult Japanese female patients with pectus excavatum and 64 intact Japanese adult females. The pectus excavatum patients have no other comorbidities. These two groups were defined as pectus group and intact group, respectively. The two groups showed no statistically significant differences in ages, BMI, and thoracic cage width. Fat thickness was measured for each person at the levels of the clavicle, middle-height of the sternum, nipples, and inframammary fold. The data for each level were compared between the two groups.
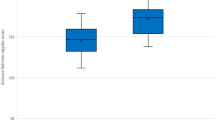
Results
Fat thickness presented statistically significant differences at the levels of nipples and inframammary fold between pectus group (17.8 ± 5.2 SD mm at the nipple level; 19.2 ± 4.9 SD mm at the inframammary fold level) and intact group (8.0 ± 2.6 SD mm at the nipple level; 10.2 ± 4.3SD mm at the inframammary fold level). Fat thickness presented no statistically significant differences between the two groups at the levels of clavicle and middle-height of the sternum.
Conclusions
The intramammary fat of female pectus excavatum patients is thicker than that of intact adult women. Because of the thick fat, the intramammary groove can appear shallow after the depressed sternum is elevated in the correction surgery for pectus excavatum. Accordingly, the breasts can look smaller. Removal or positional transfer of intramammary fat can remedy this esthetic complication.
Level of evidence: Level III, diagnostic study.






Similar content being viewed by others

References
Nagasao T, Morotomi T, Kuriyama M, Kogure T, Kudo H, Hamamoto Y, Tamai M (2017) Thoracic outlet syndrome after the Nuss procedure for pectus excavatum: is it a rare complication? J Plast Reconstr Aesthet Surg 70(10):1433–1439
Ravitch MM (1949) The operative treatment of pectus excavatum. Ann Surg 129(4):429–444
Ravitch MM (1980) A symmetric congenital deformity of the ribs. Collapse of the right side of the chest. Ann Surg 191(5):534–538
Hawkins JA, Ehrenhaft JL, Doty DB (1984) Repair of pectus excavatum by sternal eversion. Ann Thorac Surg 38(4):368–373
Taguchi TK, Mochizuki T, Nakagaki M, Kato K (1975) A new plastic operation for pectus excavatum: sternal turnover surgical procedure with preserved internal mammary vessels. Chest. 67(5):606–608
Nagasao T, Hamamoto Y, Tamai M, Kogure T, Jiang H, Takano N, Tanaka Y (2016) Scoring of deformed costal cartilages reduces postoperative pain after Nuss procedure for pectus excavatum. Thorac Cardiovasc Surg 64(1):62–69
Nagasao T, Noguchi M, Miyamoto J, Jiang H, Ding W, Shimizu Y, Kishi K (2010) Dynamic effects of the Nuss procedure on the spine in asymmetric pectus excavatum. J Thorac Cardiovasc Surg 140(6):1294–9.e1
Nagaso T, Miyamoto J, Kokaji K, Yozu R, Jiang H, Jin H, Tamaki T (2010)Double-bar application decreases postoperative pain after the Nuss procedure. J Thorac Cardiovasc Surg 140(1):39–44 44.e1–2
Nagasao T, Aizezi N, Noguchi M, Morotomi T, Kudo H, Kogure T (2019)Bone-cartilage proportion in deformed ribs of male pectus excavatum patients. J Plast Surg Hand Surg 53(3):143–148
Ors S (2017) Incidence and classification of chest wall deformities in breast augmentation patients. Aesthet Plast Surg 41(6):1280–1290
Ma IT, Rebecca AM, Notrica DM, McMahon LE, Jaroszewski DE (2015) Pectus excavatum in adult women: repair and the impact of prior or concurrent breast augmentation. Plast Reconstr Surg 135(2):303e–312e
Pereira LH, Sterodimas A (2008) Free fat transplantation for the aesthetic correction of mild pectus excavatum. Aesthet Plast Surg 32(2):393–396
Rha EY, Kim JM, Yoo G, Jeong JY, Hwang DK, Kim KJ (2016) Is breast asymmetry caused by volume differences in women with pectus excavatum? J Plast Reconstr Aesthet Surg 69(4):470–474
Schwabegger AH, Del Frari B, Pierer G (2012) Aesthetic improvement of the female breast in funnel chest deformity by surgical repair of the thoracic wall: indication or lifestyle surgery? Plast Reconstr Surg 130(2):245e–253e
Bracaglia R, D'Ettorre M, Gentileschi S, Tambasco D (2014) Was the surgeon a satisfactory informant? How to minimize room for claims. Aesthet Surg J 34(4):632–635
Ho Quoc C, Delaporte T, Meruta A, La Marca S, Toussoun G, Delay E (2013) Breast asymmetry and pectus excavatum improvement with fat grafting. Aesthet Surg J 33(6):822–829
Gentileschi S, Bracaglia R, Garganese G, Gallucci V, Corrado G, Pacelli F, Scambia G (2013) Immediate definitive prosthetic reconstruction in patients with ptotic breasts. Ann Plast Surg 70(2):144–148
Rodrigues PL, Direito-Santos B, Moreira AH, Fonseca JC, Pinho AC, Rodrigues NF, Henriques-Coelho T, Correia-Pinto J, Vilaça JL (2013) Variations of the soft tissue thicknesses external to the ribs in pectus excavatum patients. J Pediatr Surg 48(9):1878–1886
Funding
Part of this study was funded by the Grand-in-Aid for Scientific Research (C) (18K12034) provided by the Japanese Government. Part of this study was supported by JSPS KAKENHI Grant-in-Aid for Scientific Research (C) 18 K12034.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Tomohisa Nagasao, Tomoki Miyanagi, Motoki Tamai, Asako Hatano, Tetsukuni Kogure, and Tadaaki Morotomi have no conflict of interest.
Ethics approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards. The Human Investigation Committee (IRB) of Kagawa University approved this study (Approval #2019-138).
Informed consent
Informed consent was obtained from all individual participants included in the study. Patients signed informed consent regarding publishing their data and photographs.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Nagasao, T., Miyanagi, T., Tamai, M. et al. Evaluation of fat thickness in the intramammary groove of adult female patients with pectus excavatum. Eur J Plast Surg 45, 89–94 (2022). https://doi.org/10.1007/s00238-020-01777-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00238-020-01777-y