Abstract
Purpose
Severe mental illness (SMI) may interfere with parental caregiving practices and offspring development. Adhering to preventive well-child visits and maintaining good oral hygiene during early childhood requires parental involvement. Whether these activities are affected by parental SMI is unclear. The purpose of the present study was to determine whether children exposed to parental SMI are at increased risk of non-attendance to preventive well-child visits and vaccinations at age 0–5 years and of child dental caries experience at age 5 years. Furthermore, interactions between maternal psychiatric and sociodemographic variables in relation to an adverse child outcome were assessed.
Methods
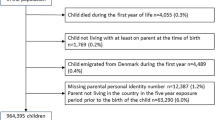
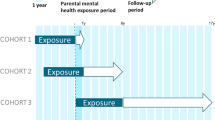
Data were obtained from national Danish health registers. All children born in Denmark between January 1997 and December 2010 were followed from birth until their 6th birthday.
Results
679,339 children were included in the study (51% male). Of these, 49,059 children (7.8%) had at least one parent with a lifetime SMI diagnosis. Children of parents with SMI had elevated odds of missing well-child visits and vaccinations (OR 1.41; 95% CI 1.39–1.44, p < 0.0001), and of child dental caries (OR 1.58; 95% CI 1.55–1.62, p < 0.0001). In the presence of maternal SMI, low socioeconomic classification and single-mother status added more to the elevated risk than specific maternal diagnosis or timing of last psychiatric contact.
Conclusion
Parents with SMI are less compliant with preventive child healthcare activities than parents without SMI. This indicates a need for practical support to these families in order to prevent inequality in health among their offspring.

Similar content being viewed by others
Data availability
Data can be obtained from Danish national health registers with obtained permissions.
References
Maybery DJ, Reupert AE, Patrick K, Goodyear M, Crase L (2018) Prevalence of parental mental illness in Australian families. Psychiatr Bull 33(1):22–26
Yang SW, Kernic MA, Mueller BA, Simon GE, Chan KCG, Vander Stoep A (2020) Association of parental mental illness with child injury occurrence, hospitalization, and death during early childhood. JAMA Pediatr 174:e201749
Ranning A, Munk Laursen T, Thorup A, Hjorthoj C, Nordentoft M (2016) Children of parents with serious mental illness: with whom do they grow up? A prospective, population-based study. J Am Acad Child Adolesc Psychiatry 55(11):953–961
Davidsen KA, Harder S, MacBeth A, Lundy JM, Gumley A (2015) Mother-infant interaction in schizophrenia: transmitting risk or resilience? A systematic review of the literature. Soc Psychiatry Psychiatr Epidemiol 50(12):1785–1798
Bernard K, Nissim G, Vaccaro S, Harris JL, Lindhiem O (2018) Association between maternal depression and maternal sensitivity from birth to 12 months: a meta-analysis. Attach Hum Dev 20(6):578–599
Goldman SL, Owen MT (1994) The impact of parental trait anxiety on the utilization of health care services in infancy: a prospective study. J Pediatr Psychol 19(3):369–381
Chung EK, McCollum KF, Elo IT, Lee HJ, Culhane JF (2004) Maternal depressive symptoms and infant health practices among low-income women. Pediatrics 113(6):e523–e529
Minkovitz CS, Strobino D, Scharfstein D, Hou W, Miller T, Mistry KB, Swartz K (2005) Maternal depressive symptoms and children’s receipt of health care in the first 3 years of life. Pediatrics 115(2):306–314
Farr SL, Dietz PM, Rizzo JH, Vesco KK, Callaghan WM, Bruce FC, Bulkley JE, Hornbrook MC, Berg CJ (2013) Health care utilisation in the first year of life among infants of mothers with perinatal depression or anxiety. Paediatr Perinat Epidemiol 27(1):81–88
Turner C, Boyle F, O’Rourke P (2003) Mothers’ health post-partum and their patterns of seeking vaccination for their infants. Int J Nurs Pract 9:120–126
Lyngsoe BK, Vestergaard CH, Rytter D, Vestergaard M, Munk-Olsen T, Bech BH (2018) Attendance of routine childcare visits in primary care for children of mothers with depression: a nationwide population-based cohort study. Br J Gen Pract 68(667):e97–e104
Watson JM, Kemper KJ (1995) Maternal factors and child’s health care use. Social Sci Med 40(5):623–628
Anderson LN, Campbell MK, DaSilva O, Freeman T, Xie B (2008) Effect of maternal depression and anxiety on use of health services for infants. Can Fam Physician 54:1718–1719.e4
dos Santos Pinto G, de Ávila Quevedo L, Britto Correa M, Sousa Azevedo M, Leão Goettems M, Tavares Pinheiro R, Demarco FF (2017) Maternal depression increases childhood dental caries: a cohort study in Brazil. Caries Res 51(1):17–25
Pedersen CB (2011) The Danish civil registration system. Scand J Public Health 39(7 Suppl):22–25
Mors O, Perto GP, Mortensen PB (2011) The Danish psychiatric central research register. Scand J Public Health 39(7 Suppl):54–57
Thygesen L (1995) The register-based system of demographic and social statistics in Denmark. Stat J U N Econ Comm Eur 12:49–55
Andersen JS, Olivarius Nde F, Krasnik A (2011) The Danish national health service register. Scand J Public Health 39(7 Suppl):34–37
Helm S (1973) Recording system for the Danish child dental health services. Commun Dent Oral Epidemiol 1:3–8
Sondergaard G, Biering-Sorensen S, Michelsen SI, Schnor O, Andersen AM (2008) Non-participation in preventive child health examinations at the general practitioner in Denmark: a register-based study. Scand J Prim Health Care 26(1):5–11
Christensen LB, Petersen PE, Hede B (2010) Oral health in children in Denmark under different public dental health care schemes. Community Dent Health 27:94–101
Frølich A (ed) (2011) Hvad kan det danske sundhedsvæsen lære af Kaiser Permanente? En sammenligning mellem den amerikanske forsikringsinstitution Kaiser Permanente og det danske sundhedsvæsen [What can the Danish healthcare system learn from Kaiser Permanente? A comparison between the American health consortium Kaiser Permanente and the Danish healthcare system]. University Press of Southern Denmark, Odense
Seow WK, Clifford H, Battistutta D, Morawska A, Holcombe T (2009) Case-control study of early childhood caries in Australia. Caries Res 43(1):25–35
Al-Jewair TS, Leake JL (2010) The prevalence and risks of early childhood cariec (ECC) in Toronto Canada. J Contemp Dental Pract 11(5):1–9
Kisely S, Baghaie H, Lalloo R, Siskind D, Johnson NW (2015) A systematic review and meta-analysis of the association between poor oral health and severe mental illness. Psychosom Med 77(1):83–92
De Hert M, Corell CU, Bobes J, Cetkovich-Bakmas M, Cohen D, Asai I, Detraux J, Gautam S, Möller H-J, Ndetei DM, Newcomer JW, Uwakwe R, Leucht S (2011) Physical illness in patients with severe mental disorders. I. Prevalence, impact of medications and disparities in health care. World Psychiatry 10:52–77
Thorup AAE, Laursen TM, Munk-Olsen T, Ranning A, Mortensen PB, Plessen KJ, Nordentoft M (2018) Incidence of child and adolescent mental disorders in children aged 0–17 with familial high risk for severe mental illness—a Danish register study. Schizophr Res 197:298
Ranning A, Benros ME, Thorup AAE, Davidsen KA, Hjorthoj C, Nordentoft M, Laursen TM, Sørensen H (2019) Morbidity and mortality in the children and young adult offspring of parents with schizophrenia or affective disorders—a nationwide register-based cohort study in 2 million individuals. Schizophr Bull. https://doi.org/10.1093/schbul/sbz040
Gibb S, Milne B, Shackleton N, Taylor BJ, Audas R (2019) How universal are universal preschool health checks? An observational study using routine data from New Zealand’s B4 School Check. BMJ Open 9(4):e025535
Clausen W, Watanabe-Galloway S, Bill Baerentzen M, Britigan DH (2016) Health literacy among people with serious mental illness. Comm Ment Health J 52(4):399–405
Bo A, Friis K, Osborne RH, Maindal HT (2014) National indicators of health literacy: ability to understand health information and to engage activelly with healthcare providers—a population based survey among Danish adults. BMC Public Health 14:1095–1107
Galletly C, Neaves A, Burton C, Liu D, Denson LA (2012) Evaluating health literacy in people with mental illness using the test of functional health literacy in adults. Nurs Outlook 60(5):316–321
Americano GC, Jacobsen PE, Soviero VM, Haubek D (2017) A systematic review on the association between molar incisor hypomineralization and dental caries. Int J Paediatr Dent 27(1):11–21
Nørrisgaard PE, Haubek D, Kühnisch J, Chawes BL, Stokholm J, Bønnelykke K, Bisgaard H (2019) Association of high-dose vitamin D supplementation during pregnancy with the risk of enamel defects in offspring: a 6-year follow-up of a randomized clinical trial. JAMA Pediatrics. https://doi.org/10.1001/jamapediatrics.2019.2545
Funding
The study was funded by the Mental Health Research Foundation in the Region of Southern Denmark.
Author information
Authors and Affiliations
Contributions
All authors contributed to the conception and design of the study, KAD and NB extracted data. EC conducted the statistical analysis and all authors contributed to the interpretation of data. KAD and EC drafted the first version of the manuscript, and all authors revised the manuscript critically for important content. All authors approved the final version and agreed to be accountable for all aspects of the work. KAD and AC had full access to all the data in the study and take full responsibility for the integrity of the data and accuracy of the data analysis. The corresponding author attests that all listed authors meet authorship criteria and that no others meeting the criteria have been omitted.
Corresponding author
Ethics declarations
Conflict of interest
All authors have completed the Unified Competing Interest form (available on request from the corresponding author) and declare no conflict of interest.
Ethical approval
Danish register based studies that do not comprise human biological material do not need to be approved by the ethical committee.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Davidsen, K.A., Christiansen, E., Haubek, D. et al. Parental mental illness, attendance at preventive child healthcare and dental caries in the offspring: a nation-wide population-based cohort study. Soc Psychiatry Psychiatr Epidemiol 56, 583–592 (2021). https://doi.org/10.1007/s00127-020-01936-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00127-020-01936-3