Abstract
Objective
Shock heart syndrome (SHS) is associated with lethal arrhythmias (ventricular tachycardia/ventricular fibrillation, VT/VF). We investigated whether liposome-encapsulated human hemoglobin vesicles (HbVs) has comparable persistent efficacy to washed red blood cells (wRBCs) for improving arrhythmogenesis in the subacute to chronic phase of SHS.
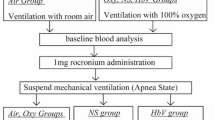
Methods
Optical mapping analysis (OMP), electrophysiological study (EPS), and pathological examinations were performed on blood samples from Sprague-Dawley rats following induction of hemorrhagic shock. After hemorrhagic shock, the rats were immediately resuscitated by transfusing 5% albumin (ALB), HbV, or wRBCs. All rats survived for 1 week. OMP and EPS were performed on Langendorff-perfused hearts. Spontaneous arrhythmias and heart rate variability (HRV) were evaluated using awake 24-h telemetry, cardiac function by echocardiography, and pathological examination of Connexin43.
Results
OMP showed significantly impaired action potential duration dispersion (APDd) in the left ventricle (LV) in the ALB group whereas APDd was substantially preserved in the HbV and wRBCs groups. Sustained VT/VF was easily provoked by EPS in the ALB group. No VT/VF was induced in the HbV and wRBCs groups. HRV, spontaneous arrhythmias, and cardiac function were preserved in the HbV and wRBCs groups. Pathology showed myocardial cell damage and Connexin43 degradation in the ALB group, all of which were attenuated in the HbV and wRBCs groups.
Conclusion
LV remodeling after hemorrhagic shock caused VT/VF in the presence of impaired APDd. Similar to wRBCs, HbV persistently prevented VT/VF by inhibiting persistent electrical remodeling, preserving myocardial structures, and ameliorating arrhythmogenic modifying factors in the subacute to chronic phase of hemorrhagic shock-induced SHS.
Similar content being viewed by others
References
Soliman M. Dimethyl amiloride, a Na+-H+ exchange inhibitor, and its cardioprotective effects in hemorrhagic shock in in vivo resuscitated rats. J Physiol Sci, 2009,59(3):175–180
Miyazaki K, Hori S, Inoue S, et al. Characterization of energy metabolism and blood flow distribution in myocardial ischemia in hemorrhagic shock. Am J Physiol, 1997,273(2 Pt 2):H600–H607
Adachi T, Hori S, Miyazaki K, et al. Inhibition of nitric oxide synthesis aggravates myocardial ischemia in hemorrhagic shock in constant pressure model. Shock, 1998,9(3):204–209
Thacker SA, Robinson P, Abel A, et al. Modulation of the unfolded protein response during hepatocyte and cardiomyocyte apoptosis in trauma/hemorrhagic shock. Sci Rep, 2013,3:1187
Li W, Wang X, He M, et al. Activating Na+-K+ ATPase: a potential cardioprotective therapy during early hemorrhagic shock. Med Hypotheses, 2014,83(6):685–687
Chatpun S, Cabrales P. Cardiac systolic function recovery after hemorrhage determines survivability during shock. J Trauma, 2011,70(4):787–793
McKinley TO, McCarroll T, Metzger C, et al. Shock volume: Patient-specific cumulative hypoperfusion predicts organ dysfunction in a prospective cohort of multiply injured patients. J Trauma Acute Care Surg, 2018,85(1S Suppl 2):S84–S91
Takase B, Higashimura Y, Hashimoto K, et al. Myocardial Electrical Remodeling and the Arrhythmogenic Substrate in Hemorrhagic Shock-Induced Heart: Anti-Arrhythmogenic Effect of Liposome-Encapsulated Hemoglobin (HbV) on the Myocardium. Shock, 2019,52(3):378–386
Sakai H, Masada Y, Horinouchi H, et al. Hemoglobin-vesicles suspended in recombinant human serum albumin for resuscitation from hemorrhagic shock in anesthetized rats. Crit Care Med, 2004,32(2):539–545
Sakai H, Tomiyama K, Masada Y, et al. Pretreatment of serum containing hemoglobin vesicles (oxygen carriers) to prevent their interference in laboratory tests. Clin Chem Lab Med, 2003,41(2):222–231
Sakai H, Tsai AG, Kerger H, et al. Subcutaneous microvascular responses to hemodilution with a red cell substitute consisting of polyethyleneglycol-modified vesicles encapsulating hemoglobin. J Biomed Mater Res, 1998,40(1):66–78
Phillips WT, Klipper RW, Awasthi VD, et al. Polyethylene glycol-modified liposome-encapsulated hemoglobin: a long circulating red cell substitute. J Pharmacol Exp Ther, 1999,288(2):665–670
Zarzoso M, Mironov S, Guerrero-Serna G, et al. Ventricular remodelling in rabbits with sustained high-fat diet. Acta Physiol (Oxf), 2014,211(1):36–47
Cheng Y, Mowrey KA, Nikolski V, et al. Mechanisms of shock-induced arrhythmogenesis during acute global ischemia. Am J Physiol Heart Circ Physiol, 2002,282(6):H2141–H2151
Wilson LD, Jeyaraj D, Wan X, et al. Heart failure enhances susceptibility to arrhythmogenic cardiac alternans. Heart Rhythm, 2009,6(2):251–259
Bloch Thomsen PE, Jons C, et al. Cardiac Arrhythmias and Risk Stratification After Acute Myocardial Infarction (CARISMA) Study Group. Long-term recording of cardiac arrhythmias with an implantable cardiac monitor in patients with reduced ejection fraction after acute myocardial infarction: the Cardiac Arrhythmias and Risk Stratification After Acute Myocardial Infarction (CARISMA) study. Circulation, 2010,122(13):1258–1264
Lee HB, Blaufox MD. Blood volume in rat. J Nucl Med, 1985,26(1):72–76
Cannon JW. Hemorrhagic Shock. N Engl J Med, 2018,378(4):370–379
Seishi Y, Horinouchi H, Sakai H, et al. Effect of the cellular-type artificial oxygen carrier hemoglobin vesicle as a resuscitative fluid for prehospital treatment: experiments in a rat uncontrolled hemorrhagic shock model. Shock, 2012,38(2):153–158
Sakai H, Seishi Y, Obata Y, et al. Fluid resuscitation with artificial oxygen carriers in hemorrhaged rats: profiles of hemoglobin-vesicle degradation and hematopoiesis for 14 days. Shock, 2009,31(2):192–200
Hagisawa K, Kinoshita M, Saitoh D, et al. Intraosseous transfusion of hemoglobin vesicles in the treatment of hemorrhagic shock with collapsed vessels in a rabbit model. Transfusion, 2020,60(7):1400–1409
Dutta S, Mincholé A, Quinn TA, et al. Electrophysiological properties of computational human ventricular cell action potential models under acute ischemic conditions. Prog Biophys Mol Biol, 2017,129:40–52
Glukhov AV, Fedorov VV, Lou Q, et al. Transmural dispersion of repolarization in failing and nonfailing human ventricle. Circ Res, 2010,106(5):981–989
Al-Zaiti SS, Callaway CW, Kozik TM, et al. Clinical Utility of Ventricular Repolarization Dispersion for Real-Time Detection of Non-ST Elevation Myocardial Infarction in Emergency Departments. J Am Heart Assoc, 2014,4(7):e002057
Tanaka Y, Takase B, Yao T, et al. Right ventricular electrical remodeling and arrhythmogenic substrate in rat pulmonary hypertension. Am J Respir Cell Mol Biol, 2013,49(3):426–436
Nogami Y, Takase B, Matsui T, et al. Effect of antiarrhythmic agents on heart rate variability indices after myocardial infarction: comparative experimental study of aprindine and procainamide. Biomed Pharmacother, 2005,59(Suppl 1):S169–173
Malliani A, Pagani M, Lombardi F, et al. Spectral analysis to assess increased sympathetic tone in arterial hypertension. Hypertension, 1991,17(4 Suppl):III36–42
Boluyt MO, Converso K, Hwang HS, et al. Echocardiographic assessment of age-associated changes in systolic and diastolic function of the female F344 rat heart. J Appl Physiol, 2004,96(2):822–828
Moss AJ, Zareba W, Hall WJ, et al. Prophylactic implantation of a defibrillator in patients with myocardial infarction and reduced ejection fraction. N Engl J Med, 2002,346(12):877–883
Bardy GH, Lee KL, Mark DB, et al. Amiodarone or an implantable cardioverter-defibrillator for congestive heart failure. Sudden Cardiac Death in Heart Failure Trial (SCD-HeFT) Investigators. N Engl J Med, 2005,352(3):225–237
Koyak Z, de Groot JR, Bouma BJ, et al. Sudden cardiac death in adult congenital heart disease: can the unpredictable be foreseen? Europace, 2017,19(3):401–406
Kirbas A, Kirbas O, Daglar K, et al. Novel indexes of arrhythmogenesis in preeclampsia: QT dispersion, Tp-e interval, and Tp-e/QT ratio. Pregnancy Hypertens, 2016,6(1):38–41
Meo M, Meste O, Signore S, et al. Reduction in Kv Current Enhances the Temporal Dispersion of the Action Potential in Diabetic Myocytes: Insights From a Novel Repolarization Algorithm. J Am Heart Assoc, 2016,5(2):e003078
Shu C, Huang W, Zeng Z, et al. Connexin 43 is involved in the sympathetic atrial fibrillation in canine and canine atrial myocytes. Anatol J Cardiol, 2017,18(1):3–9
Poelzing S, Rosenbaum DS. Altered connexin43 expression produces arrhythmia substrate in heart failure. Am J Physiol Heart Circ Physiol, 2004,287(4):H1762–H1770
Wit AL, Janse MJ. Reperfusion arrhythmias and sudden cardiac death: a century of progress toward an understanding of the mechanisms. Circ Res, 2001,89(9):741–743
Taguchi K, Miyasato M, Watanabe H, et al. Alteration in the pharmacokinetics of hemoglobin-vesicles in a rat model of chronic liver cirrhosis is associated with Kupffer cell phagocyte activity. J Pharm Sci, 2011,100(2):775–783
Natanson C, Kern SJ, Lurie P, et al. Cell-free hemoglobin-based blood substitutes and risk of myocardial infarction and death: a meta-analysis. JAMA, 2008,299(19):2304–2312
Burhop K, Gordon D, Estep T. Review of hemoglobin-induced myocardial lesions. Artif Cells Blood Substit Immobil Biotechnol, 2004,32(3):353–374
Sakai H. Present situation of the development of cellular-type hemoglobin-based oxygen carrier (hemoglobin-vesicles). Curr Drug Discov Technol, 2012,9(3):188–193
Takeoka S, Teramura Y, Atoji T, et al. Effect of Hb-encapsulation with vesicles on H2O2 reaction and lipid peroxidation. Bioconjug Chem, 2002,13(6):1302–1308
Sakai H, Sou K, Horinouchi H, et al. Hemoglobin-vesicle, a cellular artificial oxygen carrier that fulfils the physiological roles of the red blood cell structure. Adv Exp Med Biol, 2010,662:433–438
Yadav VR, Rao G, Houson H, et al. Nanovesicular liposome-encapsulated hemoglobin (LEH) prevents multi-organ injuries in a rat model of hemorrhagic shock. Eur J Pharm Sci, 2016,93:97–106
Taguchi K, Urata Y, Anraku M, et al. Pharmacokinetic study of enclosed hemoglobin and outer lipid component after the administration of hemoglobin vesicles as an artificial oxygen carrier. Drug Metab Dispos, 2009,37(7):1456–1463
Kaneda S, Ishizuka T, Goto H, et al. Liposome-Encapsulated Hemoglobin, TRM-645: Current Status of the Development and Important Issues for Clinical Application. Artif Organs, 2009,33(2):146–152
Nogami Y, Takase B, Kinoshita M, et al. Liposome-encapsulated hemoglobin attenuates cardiac dysfunction and sympathetic activity during hypohemoglobinemic shock. Shock, 2012,38(2):159–164
Huikuri HV, Raatikainen MJ, Moerch-Joergensen R, et al. Cardiac Arrhythmias and Risk Stratification after Acute Myocardial Infarction study group. Prediction of fatal or near-fatal cardiac arrhythmia events in patients with depressed left ventricular function after an acute myocardial infarction. Eur Heart J, 2009,30:689–698
Chen JY, Scerbo M, Kramer G. A review of blood substitutes: examining the history, clinical trial results, and ethics of hemoglobin-based oxygen carriers. Clinics (Sao Paulo), 2009,64(8):803–813
Jahr JS, Mackenzie C, Pearce LB, et al. HBOC-201 as an Alternative to Blood Transfusion: Efficacy and Safety Evaluation in a Multicenter Phase III Trial in Elective Orthopedic Surgery. J Trauma, 2008,64(6):1484–1497
Gould SA, Moore EE, Hoyt DB, et al. The first randomized trial of human polymerized hemoglobin as a blood substitute in acute trauma and emergent surgery. J Am Coll Surg, 1998,187(2):113–120
Jahr JS, Akha AS, Holtby RJ. Crosslinked, polymerized, and PEG-conjugated hemoglobin-based oxygen carriers: clinical safety and efficacy of recent and current products. Curr Drug Discov Technol, 2012,9(3):158–165
Acknowledgements
The authors express sincere gratitude to Professor Susumu Matsukuma in the Department of Pathology and Laboratory Medicine, National Defense Medical College for his expertise and for supervising and analyzing the pathological findings in this study. In addition, we would like to thank Editage (www.editage.com) for English language editing.
Author information
Authors and Affiliations
Corresponding author
Additional information
Conflict of Interest Statement
The authors declare that they have no competing interests.
This work was supported in part by the Project Promoting Clinical Trials for Development of New Drugs and Medical Devices from the Japan Agency for Medical Research and Development (AMED), Japan.
Rights and permissions
About this article
Cite this article
Takase, B., Higashimura, Y., Asahina, H. et al. Liposome-Encapsulated Hemoglobin Vesicle Improves Persistent Anti-arrhythmogenesis through Improving Myocardial Electrical Remodeling and Modulating Cardiac Autonomic Activity in a Hemorrhagic Shock-Induced Rat Heart Model. CURR MED SCI 43, 232–245 (2023). https://doi.org/10.1007/s11596-023-2706-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11596-023-2706-9