Abstract
Purpose
A safe and effective insulin infusion algorithm that achieves rigorous intraoperative glycemic control in noncardiac surgery has yet to be formally characterized and evaluated. We therefore report the validation of the DeLit Trial insulin infusion algorithm.
Methods
Patients scheduled for major noncardiac surgery were randomized to a target intraoperative blood glucose concentration of 4.4-6.1 mmoL·L−1 (80-110 mg·dL−1) intensive group or 10-11.1 mmoL·L−1 (180-200 mg·dL−1) conventional group. Glucose was managed with a dynamic intravenous insulin infusion algorithm. We compared the randomized groups on glucose time-weighted average (TWA), proportion of time spent within target, number of severe (< 2.2 mmoL·L−1 or < 40 mg·dL−1) or moderate (< 2.8 mmoL·L−1or < 50 mg·dL−1) hypoglycemic episodes, and within-patient variability in glucose concentrations expressed as standard deviation from the patient mean.
Results
One hundred eighty-seven patients were assigned to intensive glucose control, and 177 patients were assigned to conventional glucose control. Median (lower quartile value [Q1], upper quartile value [Q3]) of intraoperative TWA for the intensive vs conventional groups was 6 [5.6, 6.7] mmoL·L−1 vs 7.7 [6.9, 9.2] mmoL·L−1, respectively; P < 0.001. The intensive group spent 49% (29, 71) of the time within target, substantially more time than the conventional group spent either within the intensive target or within its own target (both P < 0.001). The intensive group had slightly lower within-patient glucose variability than the conventional group (0.9 [0.7, 1.3] mmoL·L−1 vs 1.3 [0.8, 1.8] mmoL·L−1, respectively; P < 0.001). Three patients had moderate hypoglycemia (intensive group), but none experienced severe episodes.
Conclusion
Tight intraoperative glucose control in noncardiac surgery can be maintained successfully without serious hypoglycemic episodes. (ClinicalTrials.gov number, NCT00433251).
Résumé
Objectif
Nous ne disposons pas encore d’un algorithme de perfusion d’insuline formellement caractérisé et évalué, qui soit à la fois sécuritaire et efficace, et qui permette de maintenir un contrôle glycémique peropératoire rigoureux en chirurgie non cardiaque. C’est pourquoi nous rapportons la validation de notre algorithme de perfusion de l’insuline.
Méthode
Des patients devant subir une chirurgie non cardiaque majeure ont été randomisés à une concentration glycémique peropératoire cible de 4,4-6,1 mmoL·L−1 (80-110 mg·dL−1) dans le groupe intensif ou à une concentration de 10-11,1 mmoL·L−1 (180-200 mg·dL−1) dans le groupe conventionnel. La glycémie a été contrôlée à l’aide d’un algorithme dynamique de perfusion intraveineuse d’insuline. Nous avons comparé les groupes randomisés en matière de moyenne pondérée dans le temps, de la proportion de temps passé à la concentration cible, du nombre d’épisodes d’hypoglycémie grave (< 2,2 mmoL·L−1 ou < 40 mg·dL−1) ou modérée (< 2,8 mmoL·L−1 ou < 50 mg·dL−1), ainsi que de la variabilité chez un même patient des concentrations glycémiques, exprimée en tant qu’écart type de la moyenne du patient.
Résultats
Cent quatre-vingt-sept patients ont été attribués au groupe contrôle glycémique intensif, et 177 au groupe contrôle glycémique conventionnel. La médiane (valeur du quartile inférieur [Q1], valeur du quartile supérieur [Q3]) de la moyenne pondérée dans le temps pour les groupes intensif vs conventionnel était de 6 (5,6, 6,7) mmoL·L−1 vs 7,7 (6,9, 9,2), respectivement; P < 0,001. Le groupe intensif a passé 49 % (29, 71) du temps dans la zone cible, soit considérablement plus de temps que le groupe conventionnel n’a passé dans la zone cible intensive ou dans sa propre zone cible (tous deux P < 0,001). Le groupe intensif a présenté une variabilité chez un même patient légèrement plus basse que le groupe conventionnel (0,9 [0,7, 1,3] mmoL·L−1 vs 1,3 [0,8, 1,8] mmoL·L−1, respectivement; P < 0,001). Trois patients ont présenté une hypoglycémie modérée (groupe intensif), mais aucun patient n’a manifesté d’épisode grave.
Conclusion
Un contrôle glycémique peropératoire rigoureux peut être maintenu en chirurgie non cardiaque sans épisode hypoglycémique grave. (Numéro de ClinicalTrials.gov, NCT00433251).





Similar content being viewed by others
References
The Action to Control Cardiovascular Risk in Diabetes Study Group; Gerstein HC, Miller ME, et al. Effects of intensive glucose lowering in type 2 diabetes. N Engl J Med 2008 358: 2545-59.
van den Berghe G, Wouters P, Weekers F, et al. Intensive insulin therapy in the critically ill patients. N Engl J Med 2001; 345: 1359-67.
Chant C, Wilson G, Friedrich JO. Validation of an insulin infusion nomogram for intensive glucose control in critically ill patients. Pharmacotherapy 2005; 25: 352-9.
Gandhi GY, Nuttall GA, Abel MD, et al. Intensive intraoperative insulin therapy versus conventional glucose management during cardiac surgery: a randomized trial. Ann Intern Med 2007; 146: 233-43.
Abdelmalak B, Maheshwari A, Mascha E, et al. Design and Organization of the Dexamethasone, Light Anesthesia and Tight Glucose Control (DeLiT) Trial: a factorial trial evaluating the effects of corticosteroids, glucose control, and depth-of-anesthesia on perioperative inflammation and morbidity from major non-cardiac surgery. BMC Anesthesiol 2010; 10: 11.
Subramaniam B, Panzica PJ, Novack V, et al. Continuous perioperative insulin infusion decreases major cardiovascular events in patients undergoing vascular surgery: a prospective, randomized trial. Anesthesiology 2009; 110: 970-7.
Van den Berghe G, Wilmer A, Hermans G, et al. Intensive insulin therapy in the medical ICU. N Engl J Med 2006; 354: 449-61.
Preiser JC, Devos P, Ruiz-Santana S, et al. A prospective randomised multi-centre controlled trial on tight glucose control by intensive insulin therapy in adult intensive care units: the Glucontrol study. Intensive Care Med 2009; 35: 1738-48.
Brunkhorst FM, Engel C, Bloos F, et al. Intensive insulin therapy and pentastarch resuscitation in severe sepsis. N Engl J Med 2008; 358: 125-39.
NICE-SUGAR Study Investigators, Finfer S, Chittock DR, et al. Intensive versus conventional glucose control in critically ill patients. N Engl J Med 2009; 360: 1283-97.
Moghissi ES, Korytkowski MT, DiNardo M, et al. American Association of Clinical Endocrinologists and American Diabetes Association consensus statement on inpatient glycemic control. Endocr Pract 2009; 15: 353-69.
Arabi YM, Dabbagh OC, Tamim HM, et al. Intensive versus conventional insulin therapy: a randomized controlled trial in medical and surgical critically ill patients. Crit Care Med 2008; 36: 3190-7.
Van den Berghe G, Wilmer A, Milants I, et al. Intensive insulin therapy in mixed medical/surgical intensive care units: benefit versus harm. Diabetes 2006; 55: 3151-9.
Girard M, Schricker T. Perioperative glucose control: living in uncertain times -continuing professional development. Can J Anesth 2011; 58: 312-29.
Akhtar S, Barash PG, Inzucchi SE. Scientific principles and clinical implications of perioperative glucose regulation and control. Anesth Analg 2010; 110: 478-97.
Gerstein HC, Riddle MC, Kendall DM, et al. Glycemia treatment strategies in the Action to Control Cardiovascular Risk in Diabetes (ACCORD) trial. Am J Cardiol 2007; 99: 34i-43i.
Preiser JC, Devos P. Clinical experience with tight glucose control by intensive insulin therapy. Crit Care Med 2007; 35: S503-7.
Bilotta F, Caramia R, Paoloni FP, Delfini R, Rosa G. Safety and efficacy of intensive insulin therapy in critical neurosurgical patients. Anesthesiology 2009; 110: 611-9.
Zoungas S, Patel A, Chalmers J, et al. Severe hypoglycemia and risks of vascular events and death. N Engl J Med 2010; 363: 1410-8.
Vogelzang M, Loef BG, Regtien JG, et al. Computer-assisted glucose control in critically ill patients. Intensive Care Med 2008; 34: 1421-7.
Ryan EA, Shandro T, Green K, et al. Assessment of the severity of hypoglycemia and glycemic lability in type 1 diabetic subjects undergoing islet transplantation. Diabetes 2004; 53: 955-62.
Saager L, Collins GL, Burnside B, et al. A randomized study in diabetic patients undergoing cardiac surgery comparing computer-guided glucose management with a standard sliding scale protocol. J Cardiothorac Vasc Anesth 2008; 22: 377-82.
Blaha J, Kopecky P, Matias M, et al. Comparison of three protocols for tight glycemic control in cardiac surgery patients. Diabetes Care 2009; 32: 757-61.
Kremen J, Blaha J, Kopecky P, et al. The treatment of hyperglycaemia in critically ill patients: comparison of standard protocol and computer algorithm (Czech). Vnitr Lek 2007; 53: 1269-73.
Amrein K, Ellmerer M, Hovorka R, et al. Hospital glucose control: safe and reliable glycemic control using enhanced model predictive control algorithm in medical intensive care unit patients. Diabetes Technol Ther 2010; 12: 405-12.
Zimmerman CR, Mlynarek ME, Jordan JA, Rajda CA, Horst HM. An insulin infusion protocol in critically ill cardiothoracic surgery patients. Ann Pharmacother 2004; 38: 1123-9.
Tamaki M, Shimizu T, Kanazawa A, et al. Efficacy and safety of modified Yale insulin infusion protocol in Japanese diabetic patients after open-heart surgery. Diabetes Res Clin Pract 2008; 81: 296-302.
Fahy BG, Sheehy AM, Coursin DB. Perioperative glucose control: what is enough? Anesthesiology 2009; 110: 204-6.
Egi M, Bellomo R, Stachowski E, French CJ, Hart G. Variability of blood glucose concentration and short-term mortality in critically ill patients. Anesthesiology 2006; 105: 244-52.
Krinsley JS. Glycemic control, diabetic status, and mortality in a heterogeneous population of critically ill patients before and during the era of intensive glycemic management: six and one-half years experience at a university-affiliated community hospital. Semin Thorac Cardiovasc Surg 2006; 18: 317-25.
Ali NA, O’Brien JM Jr, Dungan K, et al. Glucose variability and mortality in patients with sepsis. Crit Care Med 2008; 36: 2316-21.
Monnier L, Mas E, Ginet C, et al. Activation of oxidative stress by acute glucose fluctuations compared with sustained chronic hyperglycemia in patients with type 2 diabetes. JAMA 2006; 295: 1681-7.
Furnary AP, Cheek DB, Holmes SC, Howell WL, Kelly SP. Achieving tight glycemic control in the operating room: lessons learned from 12 years in the trenches of a paradigm shift in anesthetic care. Semin Thorac Cardiovasc Surg 2006; 18: 339-45.
Apfel CC, Korttila K, Abdalla M, et al. A factorial trial of six interventions for the prevention of postoperative nausea and vomiting. N Engl J Med 2004; 350: 2441-51.
Weber CR, Griffin JM. Evaluation of dexamethasone for reducing postoperative edema and inflammatory response after orthognathic surgery. J Oral Maxillofac Surg 1994; 52: 35-9.
Bisgaard T, Klarskov B, Kehlet H, Rosenberg J. Preoperative dexamethasone improves surgical outcome after laparoscopic cholecystectomy: a randomized double-blind placebo-controlled trial. Ann Surg 2003; 238: 651-60.
Acknowledgement
The DeLiT Trial is supported by Aspect Medical (Newton, MA) and the Cleveland Clinic Research Project Committee. Aspect Medical was purchased recently by Covidien (Dublin, Ireland). None of the authors has a personal financial interest in this research.
Competing interests
None declared.
Author information
Authors and Affiliations
Corresponding author
Appendices
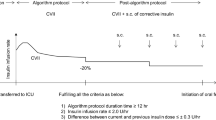
Appendix 1: Intensive glucose control
Target: 4.4-6.1 mmoL·L−1 (80-110 mg·dL−1)
Initiation of insulin infusion
Blood Glucose mmoL.L−1 (mg.dL−1) | Intravenous Bolus | Start Infusion At |
|---|---|---|
6.1-7.2 (110-130) | 2 units | 2 units/hr, recheck in 1/2 hr |
7.3-8.3 (131-150) | 2 units | 3 units/hr, recheck in 1/2 hr |
8.4-11.1 (151-200) | 3 units | 3 units/hr, recheck in 1/2 hr |
11.2-13.9 (201-250) | 5 units | 4 units/hr, recheck in 1/2 hr |
13.94-16.7 (251-300) | 5 units | 6 units/hr, recheck in 1/2 hr |
>16.7 (300) | 7 units | 8 units/hr, recheck in 1/2 hr |
Infusion adjustment
Blood Glucose mmoL·L−1 (mg·dL−1) | Decreasing Blood Glucose (↓ by more than 1.1 mmoL·L−1(20 mg·dL−1) | Stable Blood Glucose (No more than 1.1 mmoL·L−1(20 mg·dL−1) ↓ or ↑) | Increasing Blood Glucose (↑ by more than 1.1 mmoL·L−1(20 mg·dL−1) | Recheck in |
|---|---|---|---|---|
3.3 (< 60) | Hold infusion; give 50% dextrose 10-50 mL. | Hold infusion; give 50% dextrose 10-50 mL. | Hold infusion; give 50% dextrose 10-50 mL. | Immediately |
Notify staff anesthesiologist | Notify staff anesthesiologist | Notify staff anesthesiologist | ||
3.4-4.4 (61-80) | Stop infusion | Stop infusion | Continue same rate | ½ hr |
4.5-6.1 (81-110) | Decrease rate by 50% | Continue same rate | Increase rate by 25% | ½ hr |
Max. increase = 10 units/hr | ||||
6.2-7.2 (111-130) | Decrease rate by 25% | Bolus 2 units iv and maintain the current rate | Bolus 2 units iv and increase rate by 25% | ½ hr |
Max. increase = 10 units/hr | ||||
7.3-8.3 (131-150) | Decrease rate by 25% | Bolus 2 units iv and increase rate by 50% | Bolus 2 units iv and increase rate by 50% | ½ hr |
Max. increase = 10 units/hr | Max. increase = 10 units/hr | |||
8.4-11.1 (151-200) | Continue same rate | Bolus 3 units iv and increase rate by 50% | Bolus 3 units iv and increase rate by 50% | ½ hr |
Max. increase = 10 units/hr | New rate = current rate x 2 | |||
Max. increase = 10 units/hr | ||||
11.2-13.9 (201-250) | Bolus 3 units iv and continue same rate | Bolus 3 units iv and increase rate by 50% | Bolus 4 units iv and increase rate by 50% | ½ hr |
Max. increase = 10 units/hr | Max. increase = 10 units/hr | |||
13.94-16.7 (251-300) | Bolus 4 units iv and continue same rate | Bolus 4 units iv and increase rate by 50% | Bolus 5 units iv and increase rate by 50% | ½ hr |
Max. increase = 10 units/hr | Max. increase = 10 units/hr | |||
16.72-19.4 (301-350) | Bolus 5 units iv and continue same rate | Bolus 5 units iv and increase rate by 50% | Bolus 7 units iv and increase rate by 50% | ½ hr |
Max. increase = 10 units/hr | Max. increase = 10 units/hr | |||
19.5-22.2 (351-400) | Bolus 7 units iv and continue same rate | Bolus 7units iv and increase rate by 50% | Bolus 7 units iv and increase rate by 50% | ½ hr |
Max. increase = 10 units/hr | Max. increase = 10 units/hr | |||
> 22.2 (400) | Bolus 8 units iv and continue same rate Notify staff anesthesiologist | Bolus 8 units iv and increase rate by 50% | Bolus 10 units iv and increase rate by 50% | ½ hr |
Max. increase = 10 units/hr | Max. increase = 10 units/hr | |||
Notify staff anesthesiologist | Notify staff anesthesiologist |
1. Blood glucose may be checked via arterial blood gas analyzer or bedside glucose monitor;
2. The above are guidelines only. Insulin infusions may need modification for certain individuals based on clinical judgement and different clinical situations;
3. Round infusion rates to nearest 0.5 mL·hr−1.
Appendix 2: Conventional glucose control
Target: 10-11.1 mmoL·L−1 (180-200 mg·dL−1)
Initiation of insulin infusion
Blood Glucose mmoL·L−1 (mg·dL−1) | Intravenous Bolus | Start Infusion At |
|---|---|---|
11.9-13.9 (215-250) | 2 units | 2 units/hr, recheck in 1/2 hr |
13.94-16.7 (251-300) | 3 units | 3 units/hr, recheck in 1/2 hr |
16.72-19.4 (301-350) | 4 units | 4 units/hr, recheck in 1/2 hr |
19.5-22.2 (351-400) | 6 units | 6 units/hr, recheck in 1/2 hr |
>22.2 (400) | 7 units | 8 units/hr, recheck in 1/2 hr |
Infusion adjustment
Blood Glucose mmoL·L−1 (mg·dL−1) | Decreasing Blood Glucose (↓ by more than 1.7 mmoL·L−1(30 mg·dL−1) | Stable Blood Glucose (No more than 1.7 mmoL·L−1(30 mg·dL−1) ↓ or ↑) | Increasing Blood Glucose (↑ by more than 1.7 mmoL·L−1(mg·dL−1) | Recheck in |
|---|---|---|---|---|
< 3.3 (60) | Hold infusion; give 50% dextrose 10-50 mL. Notify staff anesthesiologist | Hold infusion; give 50% dextrose 10-50 mL. | Hold infusion; give 50% dextrose 10-50 mL. | Immediately |
Notify staff anesthesiologist | Notify staff anesthesiologist | |||
3.4-8.3 (61-150) | Stop infusion | Stop infusion | Stop infusion | ½ hr |
8.4-10.0 (151-180) | Stop infusion | Decrease infusion by 50% | Continue same rate increase rate by 25% | ½ hr |
10.1-11.9 (181-215) | Stop infusion | Continue same rate | Max. increase = 10 units/hr | ½ hr |
12-12.8 (216-230) | Decrease rate by 25% | Bolus 2 units iv and increase rate by 25% | Bolus 2 units iv and increase rate by 25% | ½ hr |
Max. increase = 10 units/hr | Max. increase = 10 units/hr | |||
12.83-13.9 (231-250) | Continue same rate | Bolus 3 units iv and increase rate by 50% | Bolus 3 units iv and increase rate by 50% | ½ hr |
Max. increase = 10 units/hr | New rate = current rate x 2 | |||
Max. increase = 10 units/hr | ||||
13.94-16.7 (251-300) | Bolus 3 units iv and continue same rate | Bolus 3 units iv and increase rate by 50% | Bolus 4 units iv and increase rate by 50% | ½ hr |
Max. increase = 10 units/hr | Max. increase = 10 units/hr | |||
16.72-19.4 (301-350) | Bolus 4 units iv and continue same rate | Bolus 4 units iv and increase rate by 50% | Bolus 5 units iv and increase rate by 50% | ½ hr |
Max. increase = 10 units/hr | Max. increase = 10 units/hr | |||
19.5-22.2 (351-400) | Bolus 5 units iv and continue same rate | Bolus 5 units iv and increase rate by 50% | Bolus 7 units iv and increase rate by 50% | ½ hr |
Max. increase = 10 units/hr | Max. increase = 10 units/hr | |||
22.3-25 (401-450) | Bolus 7 units iv and continue same rate | Bolus 7 units iv and increase rate by 50% | Bolus 7 units iv and increase rate by 50% | ½ hr |
Max. increase = 10 units/hr | Max. increase = 10 units/hr | |||
>25 (450) | Bolus 8 units iv and continue same rate | Bolus 8 units iv and increase rate by 50% | Bolus 10 units iv and increase rate by 50% | ½ hr |
Notify staff anesthesiologist | ||||
Max. increase = 10 units/hr | Max. increase = 10 units/hr | |||
Notify staff anesthesiologist | Notify staff anesthesiologist |
1. Blood glucose may be checked via arterial blood gas analyzer or bedside glucose monitor;
2. The above are guidelines only. Insulin infusions may need modification for certain individuals based on clinical judgement and different clinical situations;
3. Round infusion rates to nearest 0.5 mL·hr−1;
4. Blood glucose may be checked at longer intervals (e.g., 60 min) if there was no intervention in the term of an insulin bolus or change of infusion rate and if the concentration has been stable for two readings.
Rights and permissions
About this article
Cite this article
Abdelmalak, B., Maheshwari, A., Kovaci, B. et al. Validation of the DeLiT Trial intravenous insulin infusion algorithm for intraoperative glucose control in noncardiac surgery: a randomized controlled trial. Can J Anesth/J Can Anesth 58, 606–616 (2011). https://doi.org/10.1007/s12630-011-9509-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12630-011-9509-3