Abstract
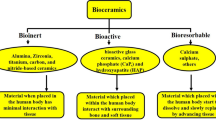
Current strategies in the field of tissue engineering are bringing functional biomaterials with required structural, mechanical, and biological performance able to endorse the repair and regeneration of injured or diseased tissues. Biocomposites formed by biodegradable polymers matrix and bioceramics have proved their effectiveness in clinics, namely in orthopedics and dental medicine. They are being used as suture anchors and interference screws, while bioceramics are indicated as cements, blocks, granules, or as coatings for metal implants. The biocompatibility and osteoconductivity of the bioceramics together with the high mechanical properties provided by the polymers make them ideal candidates towards the designing of advanced scaffolds and implants. A comprehensive overview of recent research on bioceramics and bioceramics-related biocomposites for several tissue engineering purposes are herein presented. Bioceramics and biocomposites comprising bioinert, bioactive and bioresorbable ceramics, and natural and synthetic biodegradable polymers for scaffolds processing, and respective properties are demonstrated. Interest is given to advanced manufacturing as an emergent technology for complex personalized structures fabrication. Commercial bioceramics and biocomposites available for biomedical use are also summarized.
Access this chapter
Tax calculation will be finalised at checkout
Purchases are for personal use only
Similar content being viewed by others
References
Bijukumar DR, McGeehan C, Mathew MT (2018) Regenerative medicine strategies in biomedical implants. Curr Osteoporos Rep 16:236–245
Mohamad Yunos D, Bretcanu O, Boccaccini AR (2008) Polymer-bioceramic composites for tissue engineering scaffolds. J Mater Sci 43:4433–4442
Raquel Maia F, Correlo VM, Oliveira JM et al (2019) Natural origin materials for bone tissue engineering: properties, processing, and performance. In: Atala A, Lanza R, Mikos AG et al (eds) Principles of regenerative medicine, 3rd edn. Academic Press, Boston, pp 535–558
Hasan MS, Ahmed I, Parsons AJ et al (2013) Investigating the use of coupling agents to improve the interfacial properties between a resorbable phosphate glass and polylactic acid matrix. J Biomater Appl 28:354–366
Bochicchio B, Barbaro K, De Bonis A et al (2020) Electrospun poly(d, l-lactide)/gelatin/glass-ceramics tricomponent nanofibrous scaffold for bone tissue engineering. J Biomed Mater Res A 108:1064–1076
Nie L, Wu Q, Long H et al (2019) Development of chitosan/gelatin hydrogels incorporation of biphasic calcium phosphate nanoparticles for bone tissue engineering. J Biomater Sci Polym Ed 30:1636–1657
Ribeiro VP, Pina S, Costa JB et al (2019) Enzymatically cross-linked silk fibroin-based hierarchical scaffolds for osteochondral regeneration. ACS Appl Mater Interfaces 11:3781–3799
Pina S, Oliveira JM, Reis RL (2015) Natural-based nanocomposites for bone tissue engineering and regenerative medicine: a review. Adv Mater 27:1143–1169
Yan LP, Silva-Correia J, Oliveira MB et al (2015) Bilayered silk/silk-nanoCaP scaffolds for osteochondral tissue engineering: in vitro and in vivo assessment of biological performance. Acta Biomater 12:227–241
Yun PY, Kim YK, Jeong KI et al (2014) Influence of bone morphogenetic protein and proportion of hydroxyapatite on new bone formation in biphasic calcium phosphate graft: two pilot studies in animal bony defect model. J Craniomaxillofac Surg 42:1909–1917
Yan LP, Silva-Correia J, Correia C et al (2013) Bioactive macro/micro porous silk fibroin/nano-sized calcium phosphate scaffolds with potential for bone-tissue-engineering applications. Nanomedicine 8:359–378
Canadas R, Pereira D, Silva-Correia J et al (2012) Novel bilayered Gellan gum/Gellan gum hydroxyapatite scaffolds for osteochondral tissue engineering applications. J Tissue Eng Regen Med 6:8–39
Oliveira JM, Rodrigues MT, Silva SS et al (2006) Novel hydroxyapatite/chitosan bilayered scaffold for osteochondral tissue-engineering applications: scaffold design and its performance when seeded with goat bone marrow stromal cells. Biomaterials 27:6123–6137
Stockmann P, Böhm H, Driemel O et al (2010) Resorbable versus titanium osteosynthesis devices in bilateral sagittal split ramus osteotomy of the mandible—the results of a two centre randomised clinical study with an eight-year follow-up. J Craniomaxillofac Surg 38:522–528
Kukk A, Nurmi JT (2009) A retrospective follow-up of ankle fracture patients treated with a biodegradable plate and screws. Foot Ankle Surg 15:192–197
Mittal R, Morley J, Dinopoulos H et al (2005) Use of bio-resorbable implants for stabilisation of distal radius fractures: the United Kingdom patients’ perspective. Injury 36:333–338
Pietrzak WS (2000) Principles of development and use of absorbable internal fixation. Tissue Eng 6:425–433
Kim YK, Yeo HH, Lim SC (1997) Tissue response to titanium plates: a transmitted electron microscopic study. J Oral Maxillofac Surg 55:322–326
Alpert B, Seligson D (1996) Removal of asymptomatic bone plates used for orthognathic surgery and facial fractures. J Oral Maxillofac Surg 54:618–621
Agins HJ, Alcock NW, Bansal M et al (1988) Metallic wear in failed titanium-alloy total hip replacements. A histological and quantitative analysis. J Bone Joint Surg Am 70:347–356
Causa F, Netti PA, Ambrosio L et al (2006) Poly-epsilon-caprolactone/hydroxyapatite composites for bone regeneration: in vitro characterization and human osteoblast response. J Biomed Mater Res A 76:151–162
Blasier RD, Bucholz R, Cole W et al (1997) Bioresorbable implants: applications in orthopaedic surgery. Instr Course Lect 46:531–546
Bucholz RW, Henry S, Henley MB (1994) Fixation with bioabsorbable screws for the treatment of fractures of the ankle. J Bone Joint Surg Am 76:319–324
Peltoniemi H (2000) Biocompatibility and fixation properties of absorbable miniplates and screws in growing calvarium. Dissertation, University of Helsinki
Hubbell JA (1995) Biomaterials in tissue engineering. Biotechnology 13:565–576
Sola A, Bertacchini J, D’Avella D et al (2019) Development of solvent-casting particulate leaching (SCPL) polymer scaffolds as improved three-dimensional supports to mimic the bone marrow niche. Mater Sci Eng C Mater Biol Appl 96:153–165
Gay S, Lefebvre G, Bonnin M et al (2018) PLA scaffolds production from thermally induced phase separation: effect of process parameters and development of an environmentally improved route assisted by supercritical carbon dioxide. J Supercrit Fluids 136:123–135
Song P, Zhou C, Fan H et al (2018) Novel 3D porous biocomposite scaffolds fabricated by fused deposition modeling and gas foaming combined technology. Compos B Eng 152:151–159
Brougham CM, Levingstone TJ, Shen N et al (2017) Freeze-drying as a novel biofabrication method for achieving a controlled microarchitecture within large, complex natural biomaterial scaffolds. Adv Healthc Mater. https://doi.org/10.1002/adhm.201700598
Costa JB, Silva-Correia J, Pina S et al (2019) Indirect printing of hierarchical patient-specific scaffolds for meniscus tissue engineering. Bio-des Manuf 2:225–241
Kim WJ, Yun HS, Kim GH (2017) An innovative cell-laden α-TCP/collagen scaffold fabricated using a two-step printing process for potential application in regenerating hard tissues. Sci Rep 7:3181
Gu BK, Choi DJ, Park SJ et al (2016) 3-dimensional bioprinting for tissue engineering applications. Biomater Res 20:12
Meininger S, Mandal S, Kumar A et al (2016) Strength reliability and in vitro degradation of three-dimensional powder printed strontium-substituted magnesium phosphate scaffolds. Acta Biomater 31:401–411
Ben-Nissan B, Cazalbou S, Choi AH (2019) Bioceramics. In: Narayan R (ed) Encyclopedia of biomedical engineering. Elsevier, Amsterdam, pp 16–33
Silva TH, Alves A, Ferreira BM et al (2012) Materials of marine origin: a review on polymers and ceramics of biomedical interest. Int Mater Rev 57:276–306
Correlo VM, Oliveira JM, Mano JF et al (2011) Natural origin materials for bone tissue engineering—properties, processing, and performance. In: Atalas A, Lanza R, Thomson JA et al (eds) Principles of regenerative medicine, 2nd edn. Academic Press, San Diego, pp 557–586
Oliveira JM, Grech JMR, Leonor IB et al (2007) Calcium-phosphate derived from mineralized algae for bone tissue engineering applications. Mater Lett 61:3495–3499
Zhuang H, Lin R, Liu Y et al (2019) Three-dimensional-printed bioceramic scaffolds with osteogenic activity for simultaneous photo/magnetothermal therapy of bone tumors. ACS Biomater Sci Eng 5:6725–6734
Adel-Khattab D, Giacomini F, Gildenhaar R et al (2018) Development of a synthetic tissue engineered three-dimensional printed bioceramic-based bone graft with homogenously distributed osteoblasts and mineralizing bone matrix in vitro. J Tissue Eng Regen Med 12:44–58
Kim H, Mondal S, Bharathiraja S et al (2018) Optimized Zn-doped hydroxyapatite/doxorubicin bioceramics system for efficient drug delivery and tissue engineering application. Ceram Int 44:6062–6071
Wang X, Li T, Ma H et al (2017) A 3D-printed scaffold with MoS2 nanosheets for tumor therapy and tissue regeneration. NPG Asia Mater 9:e376. https://doi.org/10.1038/am.2017.47
Ma L, Cheng S, Ji X et al (2020) Immobilizing magnesium ions on 3D printed porous tantalum scaffolds with polydopamine for improved vascularization and osteogenesis. Mater Sci Eng C Mater Biol Appl 117:111303
Xu Z, Xu Y, Basuthakur P et al (2020) Fibro-porous PLLA/gelatin composite membrane doped with cerium oxide nanoparticles as bioactive scaffolds for future angiogenesis. J Mater Chem B. https://doi.org/10.1039/d0tb01715a
Gu Y, Zhang J, Zhang X et al (2019) Three-dimensional printed Mg-doped β-TCP bone tissue engineering scaffolds: effects of magnesium ion concentration on osteogenesis and angiogenesis in vitro. Tissue Eng Regen Med 16:415–429
Stähli C, James-Bhasin M, Hoppe A et al (2015) Effect of ion release from Cu-doped 45S5 Bioglass® on 3D endothelial cell morphogenesis. Acta Biomater 19:15–22
Rath SN, Brandl A, Hiller D et al (2014) Bioactive copper-doped glass scaffolds can stimulate endothelial cells in co-culture in combination with mesenchymal stem cells. PLoS One 9:e113319
Amudha S, Ramana Ramya J, Thanigai Arul K et al (2020) Enhanced mechanical and biocompatible properties of strontium ions doped mesoporous bioactive glass. Compos B Eng 196:108099
Köse N, Asfuroğlu ZM, Köse A et al (2020) Silver ion-doped calcium phosphate-based bone-graft substitute eliminates chronic osteomyelitis: an experimental study in animals. J Orthop Res. https://doi.org/10.1002/jor.24946
Lin Z, Cao Y, Zou J et al (2020) Improved osteogenesis and angiogenesis of a novel copper ions doped calcium phosphate cement. Mater Sci Eng C Mater Biol Appl 114:111032
Motameni A, Alshemary AZ, Dalgic AD et al (2020) Lanthanum doped dicalcium phosphate bone cements for potential use as filler for bone defects. Mater Today Commun. https://doi.org/10.1016/j.mtcomm.2020.101774
Sayahi M, Santos J, El-Feki H et al (2020) Brushite (Ca,M)HPO4, 2H2O doping with bioactive ions (M = Mg2+, Sr2+, Zn2+, Cu2+, and Ag+): a new path to functional biomaterials? Mater Today Chem 16:100230
Sikder P, Coomar PP, Mewborn JM et al (2020) Antibacterial calcium phosphate composite cements reinforced with silver-doped magnesium phosphate (newberyite) micro-platelets. J Mech Behav Biomed Mater 110:103934
Bolaños RV, Castilho M, de Grauw J et al (2020) Long-Term in vivo performance of low-temperature 3d-printed bioceramics in an equine model. ACS Biomater Sci Eng 6:1681–1689
Liu Y, Li T, Ma H et al (2018) 3D-printed scaffolds with bioactive elements-induced photothermal effect for bone tumor therapy. Acta Biomater 73:531–546
Zhai D, Chen L, Chen Y et al (2020) Lithium silicate-based bioceramics promoting chondrocyte maturation by immunomodulating M2 macrophage polarization. Biomater Sci 8:4521–4534
Humbert P, Brennan MÁ, Davison N et al (2019) Immune modulation by transplanted calcium phosphate biomaterials and human mesenchymal stromal cells in bone regeneration. Front Immunol 10:663
Mansour A, Abu-Nada L, Al-Waeli H et al (2019) Bone extracts immunomodulate and enhance the regenerative performance of dicalcium phosphates bioceramics. Acta Biomater 89:343–358
Sadowska JM, Wei F, Guo J et al (2019) The effect of biomimetic calcium deficient hydroxyapatite and sintered β-tricalcium phosphate on osteoimmune reaction and osteogenesis. Acta Biomater 96:605–618
Kurzina I, Churina Y, Shapovalova Y et al (2018) Immunomodulatory properties of composite materials basedon polylactide and hydroxyapatite. Bioceram Dev Appl 8:109
Li T, Peng M, Yang Z et al (2018) 3D-printed IFN-γ-loading calcium silicate-β-tricalcium phosphate scaffold sequentially activates M1 and M2 polarization of macrophages to promote vascularization of tissue engineering bone. Acta Biomater 71:96–107
Sadowska JM, Wei F, Guo J et al (2018) Effect of nano-structural properties of biomimetic hydroxyapatite on osteoimmunomodulation. Biomaterials 181:318–332
Moonesi Rad R, Alshemary AZ, Evis Z et al (2020) Cellulose acetate-gelatin-coated boron-bioactive glass biocomposite scaffolds for bone tissue engineering. Biomed Mater 15:065009
Wu S, Ma S, Zhang C et al (2020) Cryogel biocomposite containing chitosan-gelatin/cerium-zinc doped hydroxyapatite for bone tissue engineering. Saudi J Biol Sci 27:2638–2644
Pina S, Canadas RF, Jiménez G et al (2017) Biofunctional ionic-doped calcium phosphates: silk fibroin composites for bone tissue engineering scaffolding. Cells Tissues Organs 204:150–163
Ribeiro VP, da Silva MA, Maia FR et al (2018) Combinatory approach for developing silk fibroin scaffolds for cartilage regeneration. Acta Biomater 72:167–181
Ribeiro VP, Pina S, Canadas RF et al (2019) In vivo performance of hierarchical HRP-crosslinked silk fibroin/β-TCP scaffolds for osteochondral tissue regeneration. Regen Med Front 1:e190007. https://doi.org/10.20900/rmf20190007
Wang L, Pathak JL, Liang D et al (2020) Fabrication and characterization of strontium-hydroxyapatite/silk fibroin biocomposite nanospheres for bone-tissue engineering applications. Int J Biol Macromol 142:366–375
Elomaa L, Keshi E, Sauer IM et al (2020) Development of GelMA/PCL and dECM/PCL resins for 3D printing of acellular in vitro tissue scaffolds by stereolithography. Mater Sci Eng C Mater Biol Appl 112:110958
Nokhbatolfoghahaei H, Paknejad Z, Bohlouli M et al (2020) Fabrication of decellularized engineered extracellular matrix through bioreactor-based environment for bone tissue engineering. ACS Omega 5:31943–31956
Parmaksiz M, Elçin AE, Elçin YM (2019) Decellularized bovine small intestinal submucosa-PCL/hydroxyapatite-based multilayer composite scaffold for hard tissue repair. Mater Sci Eng C Mater Biol Appl 94:788–797
Kim YS, Majid M, Melchiorri AJ et al (2018) Applications of decellularized extracellular matrix in bone and cartilage tissue engineering. Bioeng Transl Med 4:83–95
Taylor DA, Sampaio LC, Ferdous Z et al (2018) Decellularized matrices in regenerative medicine. Acta Biomater 74:74–89
Custodio CL, Broñola PJM, Cayabyab SR et al (2021) Powder loading effects on the physicochemical and mechanical properties of 3D printed poly lactic acid/hydroxyapatite biocomposites. Int J Bioprint 7:326
Oladapo BI, Zahedi SA, Ismail SO et al (2021) 3D printing of PEEK-cHAp scaffold for medical bone implant. Bio-des Manuf 4:44–59
Wang Q, Ma Z, Wang Y et al (2021) Fabrication and characterization of 3D printed biocomposite scaffolds based on PCL and zirconia nanoparticles. Bio-des Manuf 4:60–71
Backes EH, de Nóbile Pires L, Selistre‐de‐Araujo HS et al (2020) Development and characterization of printable PLA/β‐TCP bioactive composites for bone tissue applications. J Appl Polym Sci 138:e49759
Kim D, Lee J, Kim G (2020) Biomimetic gelatin/HA biocomposites with effective elastic properties and 3D-structural flexibility using a 3D-printing process. Addit Manuf 36:101616
Zhao G, Cui R, Chen Y et al (2020) 3D Printing of well dispersed electrospun PLGA fiber toughened calcium phosphate scaffolds for osteoanagenesis. J Bionic Eng 17:652–668
Wang JQ, Jiang BJ, Guo WJ (2019) Indirect 3D printing technology for the fabrication of customised β-TCP/chitosan scaffold with the shape of rabbit radial head-an in vitro study. J Orthop Surg Res 14:102
Houben A, Van Hoorick J, Van Erps J et al (2017) Indirect rapid prototyping: opening up unprecedented opportunities in scaffold design and applications. Ann Biomed Eng 45:58–83
Acknowledgements
The authors thank the financial support from the Portuguese Foundation for Science and Technology for the funds provided under the distinctions attributed to JMO (IF/01285/2015) and SP (CEECIND/03673/2017).
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2022 The Author(s), under exclusive license to Springer Nature Singapore Pte Ltd.
About this chapter
Cite this chapter
Pina, S., Kwon, I.K., Reis, R.L., Oliveira, J.M. (2022). Biocomposites and Bioceramics in Tissue Engineering: Beyond the Next Decade. In: Choi, A.H., Ben-Nissan, B. (eds) Innovative Bioceramics in Translational Medicine I. Springer Series in Biomaterials Science and Engineering, vol 17. Springer, Singapore. https://doi.org/10.1007/978-981-16-7435-8_11
Download citation
DOI: https://doi.org/10.1007/978-981-16-7435-8_11
Published:
Publisher Name: Springer, Singapore
Print ISBN: 978-981-16-7434-1
Online ISBN: 978-981-16-7435-8
eBook Packages: Chemistry and Materials ScienceChemistry and Material Science (R0)