Abstract
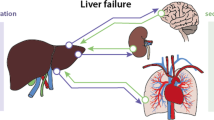
Liver dysfunction may manifest during systemic illness as a consequence of circulatory compromise — inadequate perfusion, passive congestion, intrahepatic redistribution of blood flow — or as a consequence of hepatocellular or fixed tissue macrophage (Kupffer cell) cytotoxicity. It is probable that hepatic dysfunction exacerbates the hemodynamic sequelae and multisystem dysfunction which results from infection. Certainly, underlying hepatocellular disease such as that caused by steatosis, viral hepatitis which results in changes to the cytoarchitecture will predispose to hepatocellular dysfunction in systemic illness.
Some discrete functions of the liver can be measured. However, several key aspects related to immune function are poorly characterized. Liver dysfunction is often inferred from extrahepatic organ dysfunction the severity of which can be quantified and used to characterize the severity of liver dysfunction.
Similar content being viewed by others
References
Pant C, Olyaee M, Gilroy R, Pandya PK, Olson JC, Oropeza-Vail M, Rai T, Deshpande A. Emergency department visits related to cirrhosis: a retrospective study of the nationwide emergency department sample 2006 to 2011. Medicine. 2015;94(1):e308.
Olson JC, Wendon JA, Kramer DJ, Arroyo V, Jalan R, Garcia-Tsao G, Kamath PS. Intensive care of the patient with cirrhosis. Hepatology. 2011;54(5):1864–72.
Kramer L, Jordan B, Druml W, Bauer P, Metnitz PG. Austrian Epidemiologic Study on Intensive Care, ASDI Study Group. Incidence and prognosis of early hepatic dysfunction in critically ill patients—a prospective multicenter study. Crit Care Med. 2007;35(4):1099–104.
Maynard ND, Bihari DJ, Dalton RN, Beale R, Smithies MN, Mason RC. Liver function and splanchnic ischemia in critically ill patients. Chest. 1997;111(1):180–7.
Koch A, Horn A, Duckers H, Yagmur E, Sanson E, Bruensing J, Buendgens L, Voigt S, Trautwein C, Tacke F. Increased liver stiffness denotes hepatic dysfunction and mortality risk in critically ill non-cirrhotic patients at a medical ICU. Crit Care. 2011;15(6):R266.
Ozawa K, Aoyama H, Yasuda K, et al. Metabolic abnormalities associated with postoperative organ failure. A redox theory. Arch Surg. 1983;118:1245–51.
Rolla G, Brussino L, Colagrande P, Dutto L, Polizzi S, Scappaticci E, Bergerone S, Morello M, Marzano A, Martinasso G, Salizzoni M, Bucca C. Exhaled nitric oxide and oxygenation abnormalities in hepatic cirrhosis. Hepatology. 1997;26(4):842–7.
Cremona G, Higenbottam TW, Mayoral V, Alexander G, Demoncheaux E, Borland C, Roe P, Jones GJ. Elevated exhaled nitric oxide in patients with hepatopulmonary syndrome. Eur Respir J. 1995;8(11):1883–5.
Fernandez Del Rio R, O’Hara ME, Holt A, Pemberton P, Shah T, Whitehouse T, Mayhew CA. Volatile biomarkers in breath associated with liver cirrhosis – comparisons of pre- and post-liver transplant breath samples. EBioMedicine. 2015;2(9):1243–50.
Kortgen A, Paxian M, Werth M, Recknagel P, Rauchfuss F, Lupp A, Krenn CG, Muller D, Claus RA, Reinhart K, Settmacher U, Bauer M. Prospective assessment of hepatic function and mechanisms of dysfunction in the critically ill. Shock. 2009;32(4):358–65.
Cieslak KP, Huisman F, Bais T, Bennink RJ, van Lienden KP, Verheij J, Besselink MG, Busch ORC, van Gulik TM. Future remnant liver function as predictive factor for the hypertrophy response after portal vein embolization. Surgery. 2017;162(1):37–47.
Karvellas CJ, Pink F, McPhail M, Austin M, Auzinger G, Bernal W, Sizer E, Kutsogiannis DJ, Eltringham I, Wendon JA. Bacteremia, acute physiology and chronic health evaluation II and modified end stage liver disease are independent predictors of mortality in critically ill nontransplanted patients with acute on chronic liver failure. Crit Care Med. 2010;38(1):121–6.
Karvellas CJ, Bagshaw SM. Advances in management and prognostication in critically ill cirrhotic patients. Curr Opin Crit Care. 2014;20(2):210–7.
Moreau R, Jalan R, Gines P, et al. Acute-on-chronic liver failure is a distinct syndrome that develops in patients with acute decompensation of cirrhosis. Gastro. 2013;144:1426–37.
Boone MD, Celi LA, Ho BG, Pencina M, Curry MP, Lior Y, Talmor D, Novack V. Model for End-Stage Liver Disease score predicts mortality in critically ill cirrhotic patients. J Crit Care 2014; 29(5):881.e7–13.
Schlichtig R, Klions HA, Kramer DJ, Nemoto EM. Hepatic dysoxia commences during O2 supply dependence. J Appl Physiol. 1992;72(4):1499–505.
Weemhoff JL, Woolbright BL, Jenkins RE, McGill MR, Sharpe MR, Olson JC, Antoine DJ, Curry SC, Jaeschke H. Plasma biomarkers to study mechanisms of liver injury in patients with hypoxic hepatitis. Liver Int. 2017;37(3):377–84.
Fuhrmann V, Jäger B, Zubkova A, Drolz A. Hypoxic hepatitis—epidemiology, pathophysiology and clinical management. Wien Klin Wochenschr. 2010;122:129–39.
Matuschak GM, Pinsky MR, Klein EC, Van Thiel DH, Rinaldo JE. Effects of D-galactosamine-induced acute liver injury on mortality and pulmonary responses to Escherichia coli lipopolysaccharide. Modulation by arachidonic acid metabolites. Am Rev Respir Dis. 1990;141(5 Pt 1):1296–306.
Angus DC, Linde-Zwirble WT, Lidicker J, Clermont G, Carcillo J, Pinsky MR. Epidemiology of severe sepsis in the United States: analysis of incidence, outcome, and associated costs of care. Crit Care Med. 2001;29:1303–10.
Brun-Buisson C, Meshaka P, Pinton P, Vallet B. EPISEPSIS: a reappraisal of the epidemiology and outcome of severe sepsis in French intensive care units. Intensive Care Med. 2004;30:580–8.
Vincent JL, Angus DC, Artigas A, Kalil A, Basson BR, Jamal HH, Johnson G, Bernard GR. For the recombinant human activated protein C worldwide evaluation in severe sepsis (PROWESS) study group: effects of drotrecogin alfa (activated) on organ dysfunction in the PROWESS trial. Crit Care Med. 2003;31:834–40.
Whitehead MW, Hainsworth I, Kingham JG. The causes of obvious jaundice in South West Wales: perceptions versus reality. Gut. 2001;48(3):409–13.
Chand N, Sanyal AJ. Sepsis-induced cholestasis. Hepatology. 2007;45(1):230–41.
Bhogal HK, Sanyal AJ. The molecular pathogenesis of cholestasis in sepsis. Front Biosci. 2013;5:87–96.
Singer M, Deutschman CS, Seymour CW, Shankar-Hari M, Annane D, Bauer M, et al. The third international consensus definitions for sepsis and septic shock (sepsis-3). JAMA. 2016;315(8):801–10.
Yan J, Li S, Li S. The role of the liver in sepsis. Int Rev Immunol. 2014;33(6):498–510.
Kobashi H, Toshimori J, Yamamoto K. Sepsis-associated liver injury: incidence, classification and the clinical significance. Hepatol Res. 2013;43(3):255–66.
Srivastava B, Gimson A. Hepatic changes in systemic infection. Best Pract Res Clin Gastroenterol. 2013;27(4):485–95.
Wang D, Yin Y, Yao Y. Advances in sepsis-associated liver dysfunction. Burns Trauma. 2014;2(3):97–105.
Howell MD, Davis AM. Management of sepsis and septic shock. JAMA. 2017;317(8):847–8.
Long CL, Maull KI, Krishnan RS, Laws HL, Geiger JW, Borghesi L, et al. Ascorbic acid dynamics in the seriously ill and injured. J Surg Res. 2003;109(2):144–8.
Marik PE, Khangoora V, Rivera R, Hooper MH, Catravas J. Hydrocortisone, vitamin C and thiamine for the treatment of severe sepsis and septic shock: a retrospective before-after study. Chest. 2017;151(6):1229–38.
May JM, Harrison FE. Role of vitamin C in the function of the vascular endothelium. Antioxid Redox Signal. 2013;19(17):2068–83.
Nesseler N, Launey Y, Aninat C, Morel F, Malledant Y, Seguin P. Clinical review: the liver in sepsis. Crit Care. 2012;16(5):235.
Moreno R, Sprung CL, Annane D, Chevret S, Briegel J, Keh D, Singer M, Weiss YG, Payen D, Cuthbertson BH, Vincent J. Time course of organ failure in patients with septic shock treated with hydrocortisone: results of the CORTICUS study. Intensive Care Med. 2011;37:1765–72.
Kubitz R, Wettstein M, Warskulat U, Häussinger D. Regulation of the multidrug resistance protein 2 in the rat liver by lipopolysaccharide and dexamethasone. Gastroenterology. 1999;116:401–10.
Harry R, Auzinger G, Wendon J. The clinical importance of adrenal insufficiency in acute hepatic dysfunction. Hepatology. 2002;36:395–402.
Tsai MH, Peng YS, Chen YC, Liu NJ, Ho YP, Fang JT, et al. Adrenal insufficiency in patients with cirrhosis, severe sepsis and septic shock. Hepatology. 2006;43:673–81.
Marik PE. Tight glycemic control in acutely ill patients: low evidence of benefit, high evidence of harm! Intensive Care Med. 2016;42(9):1475–7.
Mesotten D, Wauters J, Van den Berghe G, Wouters PJ, Milants I, Wilmer A. The effect of strict blood glucose control on biliary sludge and cholestasis in critically ill patients. J Clin Endocrinol Metab. 2009;94:2345–52.
Portella AO, Montero EF, deFigueiredo P. Effects of N-acetylcysteine in hepatic ischemia-reperfusion injury during hemorrhagic shock. Transplant Proc. 2004;39:846–8.
Farrell SJ, Aldag E, Pedersen R, Sahajpal A, Clendenon J, Gunabushanam V, Kramer DJ. Evaluation of the effects of N-Acetylcysteine treatment in adult liver transplant recipients. J Pharm Soc Wis. 2016;19(6):49–52.
Bañares R, Nevens F, Larsen FS, Jalan R, Albillos A, Dollinger M, et al. On behalf of the RELIEF study group. Extracorporeal albumin dialysis with the molecular adsorbent recirculating system in acute-on-chronic liver failure: the RELIEF trial. Hepatology. 2013;57:1153–62.
Dunn GD, Hayes P, Breen KJ, Schenker S. The liver in congestive heart failure: a review. Am J Med Sci. 1973;265(3):174–89.
Sherlock S. The liver in heart failure; relation of anatomical, functional, and circulatory changes. Br Heart J. 1951;13(3):273–93.
Lau GT, Tan HC, Krithrades L. Type of liver dysfunction in heart failure and its relation to the severity of tricuspid regurgitation. Am J Cardiol. 2002;90:1405–9.
Allen LA, Felker GM, Pocock S, et al. CHARM investigators. Liver function abnormalities and outcome in patients with chronic heart failure: data from the candesartan in heart failure: assessment of reduction in mortality and morbidity (CHARM) program. Eur J Heart Fail. 2009;11(2):170–7.
Van Deursen VM, Damman K, Hillege HL, et al. Abnormal liver function in relation to hemodynamic profile in heart failure patients. J Card Fail. 2010;16:84–90.
Henrion J, Schapira M, Luwaert R, et al. Hypoxic hepatitis. Medicine. 2003;82(6):392–406.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2018 Springer International Publishing AG
About this chapter
Cite this chapter
Damm, T.W., Dagar, G., Kramer, D.J. (2018). The Liver in Systemic Critical Illness. In: Nanchal, R., Subramanian, R. (eds) Hepatic Critical Care . Springer, Cham. https://doi.org/10.1007/978-3-319-66432-3_16
Download citation
DOI: https://doi.org/10.1007/978-3-319-66432-3_16
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-66431-6
Online ISBN: 978-3-319-66432-3
eBook Packages: MedicineMedicine (R0)