Abstract
Upon initial presentation, most COVID-19 patients are in a stable haemodynamic state and typically do not require intravenous (IV) fluid resuscitation. The virus primarily affects the lungs, thus the initial focus is on providing oxygen and respiratory support to the patient. Although there is limited direct research on IV fluid management for COVID-19 patients, data from observational studies suggest that patients with COVID-19-related acute respiratory distress syndrome (ARDS) exhibit higher levels of extravascular lung water and require longer periods of mechanical ventilation the more positive the cumulative fluid balance. As a result, this chapter draws on evidence from studies on fluid management for non-COVID-19 ARDS patients and pathophysiology research on COVID-19 ARDS.
You have full access to this open access chapter, Download chapter PDF
Similar content being viewed by others
Keywords
FormalPara IFA CommentaryThe outbreak of COVID-19 has contributed to our comprehension of acute respiratory distress syndrome (ARDS). As the lung is the primary target organ of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) invasion, there has been a discussion on the optimal respiratory support for such patients since the beginning of the pandemic. Additionally, COVID-19 patients frequently experience acute kidney injury, and adequate intravascular hydration is necessary for their initial care. Worse clinical outcomes have been associated with increased extravascular lung water (EVLW) in patients with ARDS. Fluid therapy is an important aspect of the management of critically ill patients with COVID-19. These patients often present with a range of clinical features that require careful assessment of their fluid status and electrolyte balance. The use of conservative or restrictive fluid management strategies has been reported in some studies, with the aim of avoiding fluid overload and associated complications, such as acute respiratory distress syndrome (ARDS) and multiple organ failure. On the other hand, liberal fluid management has also been reported to maintain organ perfusion and prevent organ failure in critically ill patients with COVID-19. The choice of fluid type is also an important consideration, with balanced crystalloid solutions such as lactated Ringer’s or Plasma-Lyte A recommended over normal saline due to their lower chloride content and potential benefits for acid-base balance. In addition, the timing and amount of fluid therapy should be individualized based on the patient’s hemodynamic status, fluid losses, and comorbidities, with frequent reassessment and adjustment as necessary. Close monitoring of fluid balance, electrolyte levels, and renal function is also important to prevent adverse events. Overall, the optimal fluid management strategy in critically ill patients with COVID-19 remains an area of active research, and a personalized approach is recommended based on the individual patient’s clinical status and response to treatment. In patients with COVID-19, as with other critically ill patients in the ICU, it is recommended to practice fluid stewardship. The conventional approach for patients with ARDS is fluid de-escalation and restriction, and a cautious strategy for intravenous fluid should be employed by considering the 4Ds (drug, dosing, duration, and de-escalation). In some cases of fluid accumulation syndrome where spontaneous egress from the ebb to flow phase does not occur, de-resuscitation using pharmacological or mechanical methods might be considered.
FormalPara Learning ObjectivesThrough this chapter, readers will learn about:
-
1.
The available evidence on the impact of extravascular lung water and fluid balance on the outcomes of coronavirus disease (COVID-19) associated acute respiratory distress syndrome (ARDS).
-
2.
The impact of fluid therapy on patient outcomes in critically ill patients with COVID-19.
-
3.
The key principles and importance of fluid stewardship and judicious intravenous (IV) fluid administration in patients of COVID-19.
-
4.
The potential benefits of critical care ultrasound in monitoring and guiding fluid therapy in COVID-19 patients and different ARDS phenotypes.
-
5.
The use of dynamic parameters in assessing fluid responsiveness in COVID-19 patients.
-
6.
The preferred types of fluids for resuscitation of COVID-19 patients.
-
7.
The current guidelines and recommendations for fluid management in COVID-19 patients, and the limitations of the available evidence.
-
8.
Need for future research on the impact of restrictive fluid strategy in the management of COVID-19 patients.
A 42-year-old male was admitted to the hospital due to cough and shortness of breath. On room air, his peripheral oxygen saturation (SpO2) was 78%, and an arterial blood gas test revealed severe hypoxemia (PaO2/FiO2 = 158). Oxygen was administered via a high-flow nasal cannula at 80% FiO2 and 60 L/min flow. Lab results showed a positive SARS-CoV-2 PCR, procalcitonin level of 0.2 ng/mL, CRP level of 78 mg/L, and serum creatinine level of 134 μmol/L. The patient’s respiratory distress worsened, necessitating invasive mechanical ventilation. After intubation, the patient’s hemodynamic status deteriorated, with a mean arterial pressure of 56 mmHg, a heart rate of 121/min, and a lactate level of 3.1 mg/dL.
Questions
-
Q1. How will you manage the hemodynamic instability of this patient?
-
Q2. How will you manage intravenous fluid status for this patient post-resuscitation?
Introduction
The global COVID-19 pandemic has sharply focused the attention of the world on critical care as a specialty. At the moment, there are no proven treatments for COVID-19, although several trials and case series extolling the merits of various agents have been published. As always, good intensive care practice is founded on a strong understanding of physiology and doing the basics well.
While issues such as staffing, resources, and ventilation strategies are undoubtedly important when considering a holistic approach to treating COVID-19, fluid management remains a cornerstone of intensive care.
Unsurprisingly, given that it is a novel virus and illness course, published data and guidelines on how best to treat patients with COVID-19 are continually evolving. In this paper, we summarize what has been published on fluid strategies in COVID-19, guidelines available, and provide some reflections on personal practice. Importantly we ask colleagues to rally around this important issue and review their own practice with regards to fluid therapy.
However, a meticulous fluid assessment using volume status, intake and output, and laboratory investigations like serum electrolytes.
What Do We Know?
It is widely recognized that the administration of fluids, whether excessive or inadequate, can have a negative impact on patient outcomes [1]. Although COVID-19 is a new disease, the fundamental principles of fluid management in critical care serve as the basis for fluid therapy in COVID-19. Additionally, insights from colleagues who have treated COVID-19 patients further enhance and refine these principles. As a result, the objectives of resuscitation and management are continually evolving.
As an example, during the early stages of the COVID-19 pandemic, it was common advice to aim for a negative fluid balance. More recently, a higher-than-expected occurrence of acute kidney injury requiring renal replacement therapy has been observed, prompting calls for a more liberal fluid strategy.
The lungs are the primary organ of involvement in patients with COVID-19. Most patients with coronavirus disease 2019 (COVID-19) are haemodynamically stable on initial presentation and do not require resuscitation. However, some patients presenting to the emergency room are dehydrated, because of fever and decreased oral intake of food and fluids at home.
A particular challenge is the fact that patients are presenting at different stages of their illness. Those that are admitted to the hospital later in the illness may be hypovolaemic due to increased losses from fever and tachypnoea. While most cases primarily present with respiratory symptoms, gastrointestinal symptoms such as vomiting and diarrhoea are not uncommon. Hence, it is important to take a concise history (paying particular attention to symptom onset), clinically assess the patient, and individualize therapy. Additionally, SARS-CoV-2 infection can involve kidneys, with the estimated prevalence of acute kidney injury (AKI) varies widely from 1% to 46%. Around 1.5–9.0% of these patients may require renal replacement therapy, with a higher incidence seen in patients with severe disease [2, 3]. The mechanisms proposed for AKI in COVID-19 are multifactorial, like, thromboses, part of systemic inflammation, drug-induced nephrotoxicity, direct viral cytotoxicity, and hypotension [3, 4]. Hence, initial fluid management in patients should assess signs of dehydration.
Extravascular lung water (EVLW) and pulmonary vascular permeability index (PVPI) are surrogates of lung injury in patients with acute respiratory distress syndrome (ARDS). The PiCCOVID study found a higher amount of EVLW and PVPI and less hemodynamic disturbances in patients with COVID-19-associated ARDS compared to non-COVID-19 ARDS with similar lung mechanics. This translates to greater hypoxemia and a more frequent requirement of prone positioning and ECMO [5].
An insight from the PRoVENT-COVID study showed a cumulative fluid balance was associated with a longer duration of mechanical ventilation in patients with COVID-19 ARDS [6]. In another retrospective study, every extra litre of IV fluid administered within the first 24 h is independently associated with the need for RRT [7].
A judicious fluid administration is thus advocated for the management of patients with COVID-19.
In general, a judicious fluid strategy whereby fluid is cautiously administered only after pre-load responsiveness has been assessed is preferable [8]. Given the incidence of myocardial dysfunction in a subset of patients [9], early use of vasopressors/inotropes alongside regular assessment via echocardiography would be prudent.
What Guidelines Are Available?
Numerous professional societies and organizations have released guidelines for the management of COVID-19 patients. Regarding fluid therapy, the primary recommendations are derived from the original Surviving Sepsis Campaign guidelines and its COVID-19-specific revision [10]. However, there is currently a lack of direct evidence for patients with COVID-19 and shock, so the guidelines were formulated based on indirect evidence from critically ill patients with sepsis and ARDS. A selection of these guidelines with an emphasis on fluid management is summarized below.
Surviving Sepsis Campaign
The Surviving Sepsis Campaign group has suggested the following in their COVID-19-specific guidelines for acute resuscitation of adults with shock [10]:
-
Use dynamic parameters to assess fluid responsiveness (weak recommendation; low quality of evidence (QE)),
-
Using a conservative over liberal fluid administration strategy (weak recommendation; very low QE),
-
Using crystalloids in preference to colloids (strong recommendation; moderate QE),
-
Balanced crystalloids are preferred over unbalanced crystalloids (weak recommendation; moderate QE).
As shown, these recommendations are based on low-quality evidence.
World Health Organization
World Health Organization guidelines recommend that patients with COVID-19 respiratory failure should be treated cautiously with intravenous fluids, especially in settings with limited availability of mechanical ventilation [11].
-
Use a conservative fluid management strategy for ARDS patients without tissue hypoperfusion.
-
In resuscitation for septic shock in adults, give 250–500 mL crystalloid fluid as a rapid bolus in the first 15–30 min and reassess for signs of fluid overload after each bolus.
-
If there is no response to fluid loading or if signs of volume overload appear, reduce, or discontinue fluid administration.
-
Consider dynamic indices of volume responsiveness to guide volume administration beyond initial resuscitation based on local resources and experience. These indices include passive leg raises, fluid challenges with serial stroke volume measurements, or variations in systolic pressure, pulse pressure, inferior vena cava size, or stroke volume in response to changes in intrathoracic pressure during mechanical ventilation.
-
Starches are associated with an increased risk of death and acute kidney injury compared to crystalloids. The effects of gelatins are less clear, but they are more expensive than crystalloids. Hypotonic (vs isotonic) solutions are less effective at increasing intravascular volume. Surviving Sepsis also suggests albumin for resuscitation when patients require substantial amounts of crystalloids; however, this conditional recommendation is based on low-quality evidence.
UK Joint Anaesthetic and Intensive Care Guidelines
The UK joint anaesthetic and intensive care guidelines advocate the following [12]:
-
Conservative fluid management strategy in ARDS.
-
In cases of significant hypotension or circulatory shock, standard circulatory assessment (fluid responsiveness, cardiac output assessment) and administration of an appropriate fluid and/or pressor (where appropriate) should occur.
-
Balanced electrolyte solutions are preferred to 0.9% saline and colloids.
-
While fluid overload should be avoided and more conservative administration may help improve respiratory function, this should be carefully balanced against the risk of inducing acute renal impairment.
-
Care should be exercised in ‘running patients too dry’ in an effort to spare the lungs, as there are increased insensible fluid losses.
Guidance and Recommendations from the International Fluid Academy
The following are some suggestions and best practice recommendations taking into account those mentioned above [13].
Assessment and Monitoring
-
The patient’s fluid balance is assessed on admission in the hospital and on a daily basis with cumulative fluid balance calculated. Whenever available daily body weight is measured.
-
Assessment of fluid as part of every clinical review using a combination of clinical judgement, vital signs, and chart records.
-
Recent laboratory results with urea and electrolytes (at least once every 24 h of fluid prescription).
-
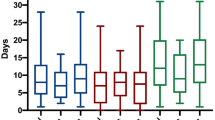
The use of cardiac output monitors to assess fluid responsiveness, e.g. ultrasound (see below) and bioimpedance monitoring (Fig. 26.1).
Sample screenshot with results obtained via the full body, multifrequency bioelectrical impedance analysis (BIA) with touch i8 device (Maltron, UK) showing a volume excess of 2.6 L and an increased ECW: ICW ratio of 0.943 indicating capillary leak. The patient’s fluid composition is monitored with BIA separating intra- and extracellular water and estimating the volume excess. (Adapted with permission from Myatchin et al. [14])
Resuscitation
-
Use balanced crystalloids (e.g. Plasmalyte).
-
Do not use starch solutions or gelatins.
-
Do not use albumin in the early stages.
-
For patients in need of fluid resuscitation:
-
Identify the cause of fluid deficit.
-
Assess for the presence of shock or hypoperfusion.
-
Assess fluid responsiveness (see further).
-
Give a bolus of 4 mL/kg of balanced crystalloids over 10–15 min.
-
-
Fluid responsiveness is assessed before and after fluid administration with functional haemodynamics, e.g. pulse pressure variation (PPV) or other tests, e.g. passive leg raise test or end-expiratory occlusion test, or a combination.
-
Mean arterial pressure and cardiac output are continuously monitored.
-
Early initiation of vasopressors: noradrenaline at a low dose 0.05 μg/kg/min.
-
Consider the addition of vasopressin/argipressin when noradrenaline dose exceeds 0.5 μg/kg/min.
-
-
Assess for the presence of fluid overload (i.e. 10% increase in body weight or volume excess from baseline).
-
Start de-resuscitation whenever possible.
-
Replace serum albumin to approximately 30 g/L with albumin 20%.
-
Use combination therapy of diuretics: loop + spironolactone + acetazolamide (when BE >5) + indapamide (in cases of hypernatraemia).
-
Consider ultrafiltration (even in the absence of acute kidney injury) when diuretics fail to achieve zero fluid balance.
-
Maintenance Fluids
-
Do not administer maintenance fluids to patients who are eating and drinking sufficiently.
-
Use hypotonic balanced solutions (e.g. Glucion 5% or Maintelyte).
-
In patients requiring IV fluids for routine maintenance alone, the initial prescription should be restricted to:
-
25–30 mL/kg/day (1 mL/kg/h) of water.
-
approximately 1 mmol/kg/day of potassium (K+).
-
approximately 1–1.5 mmol/kg/day of sodium (Na+).
-
approximately 1 mmol/kg/day of chloride (Cl−).
-
approximately 50–100 g/day (1–1.5 g/kg/day) of glucose to limit starvation ketosis.
-
-
The amount of fluid intake via other sources should be subtracted from the basic maintenance need of 1 mL/kg/h. e.g. nutrition and fluid creep (see below).
Fluid Creep
-
All sources of fluids administered need to be detailed: crystalloids, colloids, blood products, enteral and parenteral nutritional products, intravenous medication, and oral intake (water, tea, soup, etc.)
-
Precise data on the concentrated electrolytes added to these fluids or administered separately need to be documented.
-
Fluid creep is defined as the sum of the volumes of these electrolytes, the small volumes to keep venous lines open (saline or glucose 5%), and the total volume used as a vehicle for medication.
The Role of Ultrasound
In critical care, there are many different tools available to clinicians for monitoring and diagnosing patients. However, among these tools, ultrasound stands out as one of the most versatile and valuable devices, especially in the context of fluid therapy. Unlike many other monitoring devices, ultrasound is highly portable, which allows clinicians to easily use it at the patient’s bedside, even in situations with strict infection control measures in place.
What makes ultrasound particularly valuable for fluid therapy is its ability to non-invasively evaluate and assess the response to therapy for multiple physiological systems, including the cardiovascular, respiratory, and renal systems. No other singular device is able to provide such a comprehensive and integrated approach to patient care.
While critical care ultrasound has always been an important tool for clinicians, the COVID-19 pandemic has made it even more essential. The pandemic has placed tremendous pressure on healthcare systems, making it more important than ever to have access to tools that can provide timely and accurate diagnostic information. Ultrasound’s versatility and portability make it an ideal device for use in critical care settings, particularly in the context of fluid therapy. By using ultrasound to guide fluid therapy, clinicians can ensure that their patients are receiving the appropriate treatment to optimize their outcomes.
A non-exhaustive summary of the potential ultrasonographic assessments that can be performed is listed below (Table 26.1).
Fluid Stewardship: Knowing What We Are Doing
As with antibiotic stewardship, fluid stewardship can improve the quality of clinical care. Typically, this would involve a stepwise approach in assessing current practice and outcomes—a clear view of current practice will highlight the areas where we are performing well, and those that are lacking, so as to provide a basis for meaningful change [15].
Patients should have an IV fluid management plan, including a fluid and electrolyte prescription over the next 24 h agreed by the intensive care team, taking into account clinical and laboratory findings, supplemented by the appropriate imaging, e.g. ultrasound. These can be summarized by the ‘Rules of Fours’ in Table 26.2.
It is possible that some colleagues may argue that attempting to collect data on fluid prescriptions during a global pandemic is meaningless or inconvenient. However, we disagree and offer several reasons in support of our stance [16,17,18,19].
Firstly, it is undeniable that our clinical practice has undergone significant changes due to modifications in the logistics of critical care delivery. New clinical areas have been established or converted to provide care for critically ill patients, requiring healthcare professionals from non-critical care backgrounds to be redeployed and receive training and education. While collecting data requires time and effort, this time of upheaval underscores the importance of accurate documentation and data analysis to ensure that various aspects of patient care can be evaluated on a larger scale.
In addition, the current situation has made us more aware than ever of the limitations of medical resources, including healthcare professionals, personal protective equipment, machines for mechanical ventilation and haemofiltration, and essential drugs for critical care. Understanding the processes of illness and patient outcomes, as well as how our interventions affect them, will enable us to optimize the use of scarce resources for the benefit of our patients and prevent unnecessary harm.
Moreover, as COVID-19 has spread extensively, many hospitals have seen a predominance of cases. This presents an opportunity to learn valuable lessons quickly about the management of these patients, which can inform treatment plans for future waves of infection and even other epidemics.
Ultimately, when the pandemic subsides, analysing such data would allow us to reflect, review, and improve clinical practice.
Case Vignette
Questions and Answers
-
Q1. How will you manage the hemodynamic instability of this patient?
-
A1. This patient needs resuscitation. Balanced crystalloids like Plasmalyte or Ringer’s Lactate at 4 mL/kg fluid bolus should be given and followed by need of reassessment for other IV fluid. Dynamic resuscitation measures like SVV/PPV, IVC collapsibility, PLR can be used to assess fluid responsiveness. The goals of resuscitation are to improve tissue perfusion. Resuscitation can target Serum lactates.
-
Q2. How will you manage intravenous fluid status for this patient post-resuscitation?
-
A2. The fluid status of this management should be similar to the patients with ARDS. Fluid restriction (target of net negative fluid balance) with close monitoring of organ perfusion Use balanced IV fluids like Glucion 5% for maintenance. Early enteral nutrition after initial resuscitation and haemodynamic stability. Calculation of maintenance IV fluids must consider feeding and fluid creep.
Conclusion
Fluid administration and management represent fundamental practices in intensive care, and their principles are grounded in a thorough comprehension of the underlying pathophysiological processes. However, COVID-19 is a novel illness that presents unique challenges to both clinical practice and the healthcare system as a whole.
In this context, we contend that the principles of fluid stewardship have never been more critical in clinical practice than they are now. The unique challenges presented by this pandemic offer an opportunity to improve the quality of care delivered, not just for the current outbreak, but for future ones as well.
Despite the difficulties inherent in such an undertaking, it is crucial to recognize that this is an unprecedented healthcare event in modern times, with mind-boggling technology and the ability to disseminate information quickly at our disposal. Whether we opt to manage it ‘the old way’ or embrace all the tools and collaborative opportunities available to us may well determine how this pandemic is remembered in history. We firmly believe in the latter approach, which entails leveraging all available resources and working together to deliver the best possible care to our patients.
Take Home Messages
Fluid administration and management represent critical aspects of care for critically ill COVID-19 patients, particularly those with ARDS. Several key take-home messages can guide optimal fluid therapy and stewardship in these patients, including:
-
Increased extravascular lung water and cumulative fluid balance are associated with worse clinical outcomes in COVID-19 patients with ARDS.
-
Dynamic parameters should be used over static parameters to assess fluid responsiveness in COVID-19 patients.
-
Conservative/restrictive fluid strategies should be used in COVID-19 patients with ARDS.
-
Crystalloids are preferred over colloids for resuscitation of COVID-19 patients.
-
Balanced/buffered crystalloids are preferred over unbalanced crystalloids for resuscitation of COVID-19 patients.
-
When calculating maintenance fluids, consider fluid creep and feeding.
Overall, the general principles of fluid stewardship are critical to improve outcomes and optimize the use of resources in critically ill COVID-19 patients.
About the IFA
The International Fluid Academy was founded in 2011 with the goals of foster education and promote research on fluid management and monitoring in critically ill patients, thereby improving the survival of critically ill patients by bringing together physicians, nurses, and others from a variety of clinical disciplines. It aimed to improve and standardize care and outcome of critically ill patients with an emphasis on fluids, fluid management, monitoring, and organ support by collaborative research projects, surveys, guideline development, joint data registration, and international exchange of health care workers and researchers. We invite the reader to follow @Fluid_Academy and to check this website (www.fluidacademy.org and https://fluidacademy.mn.co) for more information on fluid management and haemodynamic monitoring (under FOAM resources).
References
Malbrain MLNG, Van Regenmortel N, Saugel B, et al. Principles of fluid management and stewardship in septic shock: it is time to consider the four D’s and the four phases of fluid therapy. Ann Intensive Care. 2018;8(1):66. https://doi.org/10.1186/s13613-018-0402-x.
Farouk SS, Fiaccadori E, Cravedi P, Campbell KN. COVID-19 and the kidney: what we think we know so far and what we don't. J Nephrol. 2020;33(6):1213–8. https://doi.org/10.1007/s40620-020-00789-y.
Ostermann M, Lumlertgul N, Forni LG, Hoste E. What every Intensivist should know about COVID-19 associated acute kidney injury. J Crit Care. 2020;60:91–5. https://doi.org/10.1016/j.jcrc.2020.07.023.
Nasa P, Shrivastava PK, Kulkarni A, et al. Favipiravir induced nephrotoxicity in two patients of COVID-19. J Assoc Physicians India. 2021;69(6):11–2.
Shi R, Lai C, Teboul JL, et al. COVID-19 ARDS is characterized by higher extravascular lung water than non-COVID-19 ARDS: the PiCCOVID study. Crit Care. 2021;25(1):186. https://doi.org/10.1186/s13054-021-03594-6.
Ahuja S, de Grooth HJ, Paulus F, et al. Association between early cumulative fluid balance and successful liberation from invasive ventilation in COVID-19 ARDS patients—insights from the PRoVENT-COVID study: a national, multicenter, observational cohort analysis. Crit Care. 2022;26(1):157. https://doi.org/10.1186/s13054-022-04023-y.
Holt DB, Lardaro T, Wang AZ, et al. Fluid resuscitation and progression to renal replacement therapy in patients with COVID-19. J Emerg Med. 2022;62(2):145–53. https://doi.org/10.1016/j.jemermed.2021.10.026.
Silversides JA, Perner A, Malbrain MLNG. Liberal versus restrictive fluid therapy in critically ill patients. Intensive Care Med. 2019;45:1440–9.
Zheng Y, Ma Y, Zhang J, et al. COVID-19 and the cardiovascular system. Nat Rev Cardiol. 2020;17:259–60. https://doi.org/10.1038/s41569-020-0360-5.
Alhazzani W, Evans L, Alshamsi F, et al. Surviving sepsis campaign guidelines on the management of adults with coronavirus disease 2019 (COVID-19) in the ICU: first update. Crit Care Med. 2021;49(3):e219–34. https://doi.org/10.1097/CCM.0000000000004899.
World Health Organisation Clinical management of severe acute respiratory infection (SARI) when COVID-19 disease is suspected. https://www.who.int/emergencies/diseases/novel-coronavirus-2019/events-as-they-happen.
Clinical guide for the management of critical care for adults with COVID-19 during the coronavirus pandemic—AAGBI, RCOA, FICM, ICS. https://www.england.nhs.uk/coronavirus/wp-content/uploads/sites/52/2020/03/C0216_Specialty-guide_AdultCritiCare-and-coronavirus_V2.pdf.
Malbrain MLNG, Ho S, Wong A. Thoughts on COVID-19 from the International Fluid Academy. ICU Manag Pract. 2020;20(1):80–5.
Myatchin I, Abraham P, Malbrain MLNG. Bio-electrical impedance analysis in critically ill patients: are we ready for prime time? J Clin Monit Comput. 2020;34(3):401–10. https://doi.org/10.1007/s10877-019-00439-0. Epub 2019 Dec 5. PMID: 31808061; PMCID: PMC7223384.
Malbrain MLNG, Rice TW, Mythen M, Wuyts S. It is time for improved fluid stewardship. ICU Manag Pract. 2018;18(3):158–62. https://healthmanagement.org/c/icu/issuearticle/it-is-time-for-improved-fluid-stewardship.
Poston JT, Patel BK, Davis AM. Management of critically ill adults with COVID-19. JAMA. 2020;323(18):1839–41. https://doi.org/10.1001/jama.2020.4914.
Wang D, Hu B, Hu C, et al. Clinical characteristics of 138 hospitalized patients with 2019 novel coronavirus–infected pneumonia in Wuhan, China. JAMA. 2020;323(11):1061–9. https://doi.org/10.1001/jama.2020.1585.
Silversides JA, Major E, Ferguson AJ, et al. Conservative fluid management or deresuscitation for patients with sepsis or acute respiratory distress syndrome following the resuscitation phase of critical illness: a systematic review and meta-analysis. Intensive Care Med. 2017;43:155–70. https://doi.org/10.1007/s00134-016-4573-3.
Phua J, Weng L, Ling L, et al. Intensive care management of coronavirus disease 2019 (COVID-19): challenges and recommendations. Lancet Resp Med. 2020;8(5):506–17. https://doi.org/10.1016/S2213-2600(20)30161-2.
Acknowledgements
Parts of this chapter were published previously as open access under the creative commons Attribution 4.0 International Licence (CC BY 4.0) [1]. The European Commission announced it has adopted CC BY 4.0 and CC0 to share published documents, including photos, videos, reports, peer-reviewed studies, and data. The Commission joins other public institutions around the world that use standard, legally interoperable tools like Creative Commons licenses and public domain tools to share a wide range of content they produce. The decision to use CC aims to increase the legal interoperability and ease of reuse of author’s own materials.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Open Access This chapter is licensed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license and indicate if changes were made.
The images or other third party material in this chapter are included in the chapter's Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the chapter's Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder.
Copyright information
© 2024 The Author(s)
About this chapter
Cite this chapter
Malbrain, M.L.N.G., Ho, S., Nasa, P., Wong, A. (2024). Fluid Management in COVID-19 . In: Malbrain, M.L., Wong, A., Nasa, P., Ghosh, S. (eds) Rational Use of Intravenous Fluids in Critically Ill Patients. Springer, Cham. https://doi.org/10.1007/978-3-031-42205-8_26
Download citation
DOI: https://doi.org/10.1007/978-3-031-42205-8_26
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-031-42204-1
Online ISBN: 978-3-031-42205-8
eBook Packages: MedicineMedicine (R0)