Abstract
In this chapter, we introduce the autonomic nervous system (ANS), discuss the mechanisms underlying arousal regulation in humans, and present theoretical frameworks suggesting that altered autonomic functioning is likely to contribute to behavioral, cognitive, and emotional difficulties experienced by people with attention deficit/hyperactivity disorder (ADHD). The reviewed evidence in this chapter suggests that autonomic hypofunctioning and difficulties in regulating arousal according to situational demands may cause inattention, restlessness, reduced vigilance and cognitive difficulties (especially during monotonous and unrewarding activities), and emotional dysregulation and irritability in people with ADHD. Although the chapter is specifically focused on ADHD, we also provide the reader with an overview of the literature investigating autonomic dysfunction in psychiatric or psychological conditions that often co-occur with ADHD, including oppositional defiant disorder and conduct disorder, mood disorder, and autism spectrum disorder. We discuss the effects of pharmacological and nonpharmacological interventions for ADHD on autonomic functioning, and we propose that ADHD medication and some nonpharmacological interventions may be effective in reducing inattention and hyperactivity, and improving global functioning in people with ADHD, because they normalize activity of the ANS and improve arousal regulation. The concluding sections include a brief discussion about the possible implications of the findings presented in this chapter for clinical and research practice. Specifically, we stress the importance of clarifying, in future research, the role of altered autonomic functioning in ADHD, which could prove helpful for developing more efficient and valid assessment and intervention tools for people with this neurodevelopmental condition.
Access this chapter
Tax calculation will be finalised at checkout
Purchases are for personal use only
Similar content being viewed by others
Notes
- 1.
Aware of the debate on the use of ‘person-first’ or ‘identity-first’ language to refer to people who received a diagnosis of autism spectrum disorder, we decided to use ‘autistic people’ since this is what the majority of a sample of autistic adults, family members or friends and parents of an autistic person have reported to prefer in an online survey conducted in the United Kingdom (Kenny et al., 2015). We are also aware though that this may not be the case for other countries.
Abbreviations
- ACC:
-
Anterior Cingulate Cortex
- ADHD:
-
Attention Deficit/Hyperactivity Disorder
- ANS:
-
Autonomic Nervous System
- CD:
-
Conduct Disorder
- CI:
-
Confidence Interval
- CNS:
-
Central Nervous System
- CSI:
-
Cardiac Sympathetic Index
- CVI:
-
Cardiac Vagal Index
- EDA:
-
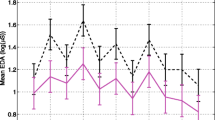
Electrodermal Activity
- EEG:
-
Electroencephalography
- ENS:
-
Enteric Nervous System
- fMRI:
-
Functional Magnetic Resonance Imaging
- HF-HRV:
-
High-Frequency component of Heart Rate Variability
- HR:
-
Heart Rate
- HRV:
-
Heart Rate Variability
- LC:
-
Locus Coeruleus
- LC-NE:
-
Locus Coeruleus-Norepinephrine
- LF-HRV:
-
Low-Frequency component of Heart Rate Variability
- NE:
-
Norepinephrine
- ODD:
-
Oppositional Defiant Disorder
- OFC:
-
Orbitofrontal Cortex
- OR:
-
Odds Ratio
- PEP:
-
Pre-Ejection Period
- PFC:
-
Pre-Frontal Cortex
- PNS:
-
Parasympathetic Nervous System
- rMSSD:
-
Square Root of the Mean of Successive Differences Between Inter-beat Intervals
- RSA:
-
Respiratory Sinus Arrhythmia
- SCT:
-
Sluggish-Cognitive Tempo
- SNS:
-
Sympathetic Nervous System
- SRD:
-
State Regulation Deficit
- vmPFC:
-
Ventro-Medial Pre-Frontal Cortex
References
Adamo, N., Michelini, G., Cheung, C. H. M., Buitelaar, J. K., Asherson, P., Rijsdijk, F., & Kuntsi, J. (2021). Does Co-Occurring Anxiety Modulate ADHD-Related Cognitive and Neurophysiological Impairments? Journal of Attention Disorders, 25(8), 1135–1145. https://doi.org/10.1177/1087054719879499
Alvares, G. A., Quintana, D. S., Hickie, I. B., & Guastella, A. J. (2016). Autonomic nervous system dysfunction in psychiatric disorders and the impact of psychotropic medications: a systematic review and meta-analysis. Journal of Psychiatry and Neuroscience, 41(2), 89–104. https://doi.org/10.1503/jpn.140217
American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders: DSM-5. https://doi.org/10.1176/appi.books.9780890425596
Anesiadou, S., Makris, G., Michou, M., Bali, P., Papassotiriou, I., Apostolakou, F., Korkoliakou, P., Papageorgiou, C., Chrousos, G., & Pervanidou, P. (2021). Salivary cortisol and alpha-amylase daily profiles and stress responses to an academic performance test and a moral cognition task in children with neurodevelopmental disorders. Stress Health, 37(1), 45–59. https://doi.org/10.1002/smi.2971
Angeli, E., Korpa, T., Johnson, E. O., Apostolakou, F., Papassotiriou, I., Chrousos, G. P., & Pervanidou, P. (2018). Salivary cortisol and alpha-amylase diurnal profiles and stress reactivity in children with Attention Deficit Hyperactivity Disorder. Psychoneuroendocrinology, 90, 174–181. https://doi.org/10.1016/j.psyneuen.2018.02.026
Arora, I., Bellato, A., Ropar, D., Hollis, C., & Groom, M. J. (2021). Is autonomic function during resting-state atypical in Autism: A systematic review of evidence. Neuroscience & Biobehavioral Reviews, 125, 417–441. https://doi.org/10.1016/j.neubiorev.2021.02.041
Aston-Jones, G., & Cohen, J. D. (2005). An integrative theory of locus coeruleus-norepinephrine function: Adaptive gain and optimal performance. Annual Review of Neuroscience, 28, 403–450. https://doi.org/10.1146/annurev.neuro.28.061604.135709
Aston-Jones, G., & Waterhouse, B. (2016). Locus coeruleus: From global projection system to adaptive regulation of behavior. Brain Research, 1645, 75–78. https://doi.org/10.1016/j.brainres.2016.03.001
Aston-Jones, G., Rajkowski, J., & Cohen, J. (2000). Locus coeruleus and regulation of behavioral flexibility and attention. Progress in Brain Research, 126, 165–182. https://doi.org/10.1016/S0079-6123(00)26013-5
Aston-Jones, G., Gonzalez, M. M. C., & Doran, S. (2007). Role of the locus coeruleus-norepinephrine system in arousal and circadian regulation of the sleep-wake cycle. Brain Norepinephrine: Neurobiology and Therapeutics. https://doi.org/10.1017/CBO9780511544156.007
Auerbach, J. G., Atzaba-Poria, N., Berger, A., & Landau, R. (2004). Emerging developmental pathways to ADHD: Possible path markers in early infancy. Neural plasticity, 11(1–2), 29–43. https://doi.org/10.1155/np.2004.29
Auerbach, J. G., Berger, A., Atzaba-Poria, N., Arbelĺe, S., Cypin, N., Friedman, A., & Landau, R. (2008). Temperament at 7, 12, and 25 months in children at familial risk for ADHD. Infant and Child Development, 17(4), 321–338. https://doi.org/10.1002/icd.579
Azeredo, A., Moreira, D., & Barbosa, F. (2018). ADHD, CD, and ODD: Systematic review of genetic and environmental risk factors. Research in Developmental Disabilities, 82, 10–19. https://doi.org/10.1016/j.ridd.2017.12.010
Barkley, R. A. (1997). Behavioral inhibition, sustained attention, and executive functions: Constructing a unifying theory of ADHD. Psychological Bulletin, 121(1), 65–94. https://doi.org/10.1037/0033-2909.121.1.65
Barkley, R. A. (2010). Deficient emotional self-regulation: A core component of attention-deficit/hyperactivity disorder. Journal of ADHD and Related Disorders, 1, 5–37.
Barrio, C., Arias-Sánchez, S., & Martín-Monzón, I. (2022). The gut microbiota-brain axis, psychobiotics and its influence on brain and behaviour: A systematic review. Psychoneuroendocrinology, 137, 105640. https://doi.org/10.1016/j.psyneuen.2021.105640
Barry, R. J., & Clarke, A. R. (2013). Resting state brain oscillations and symptom profiles in attention deficit/hyperactivity disorder. Supplements to Clinical Neurophysiology, 62, 275–287. https://doi.org/10.1016/b978-0-7020-5307-8.00017-x
Barry, R. J., Clarke, A. R., & Johnstone, S. J. (2003). A review of electrophysiology in attention-deficit/hyperactivity disorder: I. Qualitative and quantitative electroencephalography. Clinical Neurophysiology, 114(2), 171–183. https://doi.org/10.1016/s1388-2457(02)00362-0
Bast, N., Poustka, L., & Freitag, C. M. (2018). The locus coeruleus-norepinephrine system as pacemaker of attention – A developmental mechanism of derailed attentional function in autism spectrum disorder. European Journal of Neuroscience, 47(2), 115–125. https://doi.org/10.1111/ejn.13795
Bast, N., Boxhoorn, S., Supér, H., Helfer, B., Polzer, L., Klein, C., Cholemkery, H., & Freitag, C. M. (2021). Atypical arousal regulation in children with autism but not with attention-deficit/hyperactivity disorder as indicated by pupillometric measures of locus coeruleus activity. Biological Psychiatry: Cognitive Neuroscience & Neuroimaging. https://doi.org/10.1016/j.bpsc.2021.04.010
Beauchaine, T. P., & Thayer, J. F. (2015). Heart rate variability as a transdiagnostic biomarker of psychopathology. International Journal of Psychophysiology, 98(2 Pt 2), 338–350. https://doi.org/10.1016/j.ijpsycho.2015.08.004
Beauchaine, T. P., Gatzke-Kopp, L., Neuhaus, E., Chipman, J., Reid, M. J., & Webster-Stratton, C. (2013). Sympathetic- and parasympathetic-linked cardiac function and prediction of externalizing behavior, emotion regulation, and prosocial behavior among preschoolers treated for ADHD. Journal of Consulting and Clinical Psychology, 81(3), 481–493. https://doi.org/10.1037/a0032302
Beauchaine, T. P., Neuhaus, E., Gatzke-Kopp, L. M., Reid, M. J., Chipman, J., Brekke, A., Olliges, A., Shoemaker, S., & Webster-Stratton, C. (2015). Electrodermal responding predicts responses to, and may be altered by, preschool intervention for ADHD. Journal of Consulting and Clinical Psychology, 83(2), 293–303. https://doi.org/10.1037/a0038405
Becker, S. P., & McQuade, J. D. (2020). Physiological correlates of sluggish cognitive tempo in children: Examining autonomic nervous system reactivity during social and cognitive stressor tasks. Journal of Abnormal Child Psychology, 48(7), 923–933. https://doi.org/10.1007/s10802-020-00651-6
Becker, S. P., & Willcutt, E. G. (2019). Advancing the study of sluggish cognitive tempo via DSM, RDoC, and hierarchical models of psychopathology. European Child & Adolescent Psychiatry, 28(5), 603–613. https://doi.org/10.1007/s00787-018-1136-x
Bellato, A., Arora, I., Hollis, C., & Groom, M. J. (2020). Is autonomic nervous system function atypical in attention deficit hyperactivity disorder (ADHD)? A systematic review of the evidence. Neuroscience & Biobehavioral Reviews, 108, 182–206. https://doi.org/10.1016/j.neubiorev.2019.11.001
Bellato, A., Arora, I., Kochhar, P., Hollis, C., & Groom, M. J. (2021a). Indices of heart rate variability and performance during a response-conflict task are differently associated with ADHD and autism. Journal of Attention Disorders, 1087054720972793. https://doi.org/10.1177/1087054720972793
Bellato, A., Arora, I., Kochhar, P., Ropar, D., Hollis, C., & Groom, M. J. (2021b). Heart rate variability in children and adolescents with autism, ADHD and co-occurring autism and ADHD, during passive and active experimental conditions. Journal of Autism and Developmental Disorders. https://doi.org/10.1007/s10803-021-05244-w
Bellato, A., Norman, L., Idrees, I., Ogawa, C. Y., Waitt, A., Zuccolo, P. F., Tye, C., Radua, J., Groom, M. J., & Shephard, E. (2021c). A systematic review and meta-analysis of altered electrophysiological markers of performance monitoring in Obsessive-Compulsive Disorder (OCD), Gilles de la Tourette Syndrome (GTS), Attention-Deficit/Hyperactivity disorder (ADHD) and autism. Neuroscience & Biobehavioral Reviews, 131, 964–987. https://doi.org/10.1016/j.neubiorev.2021.10.018
Bellato, A., Sesso, G., Milone, A., Masi, G., & Cortese, S. (2023). Systematic Review and Meta-analysis: Altered Autonomic Functioning in Youths With Emotional Dysregulation. Journal of the American Academy of Child and Adolescent Psychiatry, S0890-8567(23)00075-8. Advance online publication. https://doi.org/10.1016/j.jaac.2023.01.017
Bench, S. W., & Lench, H. C. (2013). On the function of boredom. Behavioral sciences (Basel, Switzerland), 3(3), 459–472. https://doi.org/10.3390/bs3030459
Beopoulos, A., Gea, M., Fasano, A., & Iris, F. (2021). Autonomic nervous system neuroanatomical alterations could provoke and maintain gastrointestinal dysbiosis in Autism Spectrum Disorder (ASD): A novel microbiome-host interaction mechanistic hypothesis. Nutrients, 14(1). https://doi.org/10.3390/nu14010065
Bernhard, A., Mayer, J. S., Fann, N., & Freitag, C. M. (2021). Cortisol response to acute psychosocial stress in ADHD compared to conduct disorder and major depressive disorder: A systematic review. Neuroscience & Biobehavioral Reviews, 127, 899–916. https://doi.org/10.1016/j.neubiorev.2021.06.005
Berridge, C. W., & Waterhouse, B. D. (2003). The locus coeruleus-noradrenergic system: Modulation of behavioral state and state-dependent cognitive processes. Brain Research: Brain Research Reviews, 42(1), 33–84. https://doi.org/10.1016/s0165-0173(03)00143-7
Blomqvist, M., Holmberg, K., Lindblad, F., Fernell, E., Ek, U., & Dahllöf, G. (2007). Salivary cortisol levels and dental anxiety in children with attention deficit hyperactivity disorder. European Journal of Oral Sciences, 115(1), 1–6. https://doi.org/10.1111/j.1600-0722.2007.00423.x
Bond, A. J., James, D. C., & Lader, M. H. (1974). Physiological and psychological measures in anxious patients. Psychological Medicine, 4(4), 364–373. https://doi.org/10.1017/S0033291700045803
Börger, N., & van der Meere, J. (2000). Visual behaviour of ADHD children during an attention test: An almost forgotten variable. Journal of Child Psychology and Psychiatry, 41(4), 525-532. https://doi.org/10.1111/1469-7610.00637
Boxhoorn, S., Bast, N., Supèr, H., Polzer, L., Cholemkery, H., & Freitag, C. M. (2020). Pupil dilation during visuospatial orienting differentiates between autism spectrum disorder and attention-deficit/hyperactivity disorder. Journal of Child Psychology and Psychiatry, 61(5), 614–624. https://doi.org/10.1111/jcpp.13179
Bozhilova, N. S., Michelini, G., Kuntsi, J., & Asherson, P. (2018). Mind wandering perspective on attention-deficit/hyperactivity disorder. Neuroscience and biobehavioral reviews, 92, 464–476. https://doi.org/10.1016/j.neubiorev.2018.07.010
Bubier, J. L., & Drabick, D. A. (2008). Affective decision-making and externalizing behaviors: the role of autonomic activity. Journal of Abnormal Child Psychology, 36(6), 941–953. https://doi.org/10.1007/s10802-008-9225-9
Bundgaard-Nielsen, C., Knudsen, J., Leutscher, P. D. C., Lauritsen, M. B., Nyegaard, M., Hagstrøm, S., & Sørensen, S. (2020). Gut microbiota profiles of autism spectrum disorder and attention deficit/hyperactivity disorder: A systematic literature review. Gut Microbes, 11(5), 1172–1187. https://doi.org/10.1080/19490976.2020.1748258
Bunford, N., Evans, S. W., Zoccola, P. M., Owens, J. S., Flory, K., & Spiel, C. F. (2017). Correspondence between heart rate variability and emotion dysregulation in children, including children with ADHD. Journal of Abnormal Child Psychology, 45(7), 1325–1337. https://doi.org/10.1007/s10802-016-0257-2
Buyck, I., & Wiersema, J. R. (2014). Resting electroencephalogram in attention deficit hyperactivity disorder: Developmental course and diagnostic value. Psychiatry Research, 216(3), 391–397. https://doi.org/10.1016/j.psychres.2013.12.055
Buyck, I., & Wiersema, J. R. (2015). Task-related electroencephalographic deviances in adults with attention deficit hyperactivity disorder. Neuropsychology, 29(3), 433–444. https://doi.org/10.1037/neu0000148
Carriere, J. S. A., Seli, P., & Smilek, D. (2013). Wandering in both mind and body: individual differences in mind wandering and inattention predict fidgeting. Canadian journal of experimental psychology = Revue canadienne de psychologie experimentale, 67(1), 19–31. https://doi.org/10.1037/a0031438
Casavant, V., Chae, C., Sherwani, A., & Perlmuter, L. C. (2012). Subclinical orthostatic pulse pressure confirms mothers’ ratings of ADHD in preschoolers. Psychophysiology, 49(5), 708–712. https://doi.org/10.1111/j.1469-8986.2012.01351.x
Chang, J. P., Su, K. P., Mondelli, V., & Pariante, C. M. (2021). Cortisol and inflammatory biomarker levels in youths with attention deficit hyperactivity disorder (ADHD): Evidence from a systematic review with meta-analysis. Translational Psychiatry, 11(1), 430. https://doi.org/10.1038/s41398-021-01550-0
Checa-Ros, A., Jeréz-Calero, A., Molina-Carballo, A., Campoy, C., & Muñoz-Hoyos, A. (2021). Current evidence on the role of the gut microbiome in ADHD pathophysiology and therapeutic implications. Nutrients, 13(1), 249. https://www.mdpi.com/2072-6643/13/1/249
Cheng, Y. C., Huang, Y. C., & Huang, W. L. (2020). Heart rate variability in individuals with autism spectrum disorders: A meta-analysis. Neuroscience & Biobehavioral Reviews, 118, 463–471. https://doi.org/10.1016/j.neubiorev.2020.08.007
Colman, F. D., & Paivio, A. (1969). Pupillary response and galvanic skin response during an imagery task. Psychonomic Science, 16(6), 296–297. https://doi.org/10.3758/bf03332696
Condy, E. E., Scarpa, A., & Friedman, B. H. (2019). Restricted repetitive behaviors in autism spectrum disorder: A systematic review from the neurovisceral integration perspective. Biological Psychology, 148, 107739. https://doi.org/10.1016/j.biopsycho.2019.107739
Cortese, S., Konofal, E., Yateman, N., Mouren, M. C., & Lecendreux, M. (2006). Sleep and alertness in children with attention-deficit/hyperactivity disorder: A systematic review of the literature. Sleep, 29(4), 504–511.
Cortese, S., Adamo, N., Del Giovane, C., Mohr-Jensen, C., Hayes, A. J., Carucci, S., Atkinson, L. Z., Tessari, L., Banaschewski, T., Coghill, D., Hollis, C., Simonoff, E., Zuddas, A., Barbui, C., Purgato, M., Steinhausen, H.-C., Shokraneh, F., Xia, J., & Cipriani, A. (2018). Comparative efficacy and tolerability of medications for attention-deficit hyperactivity disorder in children, adolescents, and adults: A systematic review and network meta-analysis. The Lancet Psychiatry, 5(9), 727–738. https://doi.org/10.1016/S2215-0366(18)30269-4
Costa, V. D., & Rudebeck, P. H. (2016). More than meets the eye: The relationship between pupil size and locus coeruleus activity. Neuron, 89(1), 8–10. https://doi.org/10.1016/j.neuron.2015.12.031
Craig, F., Margari, F., Legrottaglie, A. R., Palumbi, R., de Giambattista, C., & Margari, L. (2016). A review of executive function deficits in autism spectrum disorder and attention-deficit/hyperactivity disorder. Neuropsychiatric Disease and Treatment, 12, 1191–1202. https://doi.org/10.2147/NDT.S104620
Critchley, H. D. (2005). Neural mechanisms of autonomic, affective, and cognitive integration. Journal of Comparative Neurology, 493(1), 154–166. https://doi.org/10.1002/cne.20749
Crowell, S. E., Beauchaine, T. P., Gatzke-Kopp, L., Sylvers, P., Mead, H., & Chipman-Chacon, J. (2006). Autonomic correlates of attention-deficit/hyperactivity disorder and oppositional defiant disorder in preschool children. Journal of Abnormal Psychology, 115(1), 174–178. https://doi.org/10.1037/0021-843x.115.1.174
Cuthbert, B. N., & Insel, T. R. (2013). Toward the future of psychiatric diagnosis: The seven pillars of RDoC. BMC Medicine, 11(1), 126. https://doi.org/10.1186/1741-7015-11-126
de Vries, L., Fouquaet, I., Boets, B., Naulaers, G., & Steyaert, J. (2021). Autism spectrum disorder and pupillometry: A systematic review and meta-analysis. Neuroscience & Biobehavioral Reviews, 120, 479–508. https://doi.org/10.1016/j.neubiorev.2020.09.032
Dekkers, T. J., Popma, A., Sonuga-Barke, E. J. S., Oldenhof, H., Bexkens, A., Jansen, B. R. J., & Huizenga, H. M. (2020). Risk taking by adolescents with Attention-Deficit/Hyperactivity Disorder (ADHD): A behavioral and psychophysiological investigation of peer influence. Journal of Abnormal Child Psychology, 48(9), 1129–1141. https://doi.org/10.1007/s10802-020-00666-z
Delamater, A. M., & Lahey, B. B. (1983). Physiological correlates of conduct problems and anxiety in hyperactive and learning-disabled children. Journal of Abnormal Child Psychology, 11(1), 85–100. https://doi.org/10.1007/bf00912180
Devilbiss, D. M., & Berridge, C. W. (2006). Low-dose methylphenidate actions on tonic and phasic locus coeruleus discharge. Journal of Pharmacology and Experimental Therapeutics, 319(3), 1327–1335. https://doi.org/10.1124/jpet.106.110015
Drescher, L. H., Boehler, C. N., & Wiersema, J. R. (2021). State regulation in adults scoring high versus low on ADHD symptomatology: A pupillometry study. Neuropsychology, 35(5), 486–497. https://doi.org/10.1037/neu0000738
Du Rietz, E., James, S. N., Banaschewski, T., Brandeis, D., Asherson, P., & Kuntsi, J. (2019). Autonomic arousal profiles in adolescents and young adults with ADHD as a function of recording context. Psychiatry Research, 275, 212–220. https://doi.org/10.1016/j.psychres.2019.03.039
Eisenberg, J., Ben-Daniel, N., Mei-Tal, G., & Wertman, E. (2004). An autonomic nervous system biofeedback modality for the treatment of attention deficit hyperactivity disorder – An open pilot study. Israel Journal of Psychiatry and Related Sciences, 41(1), 45–53.
Eskander, N. (2020). The psychosocial outcome of conduct and oppositional defiant disorder in children with attention deficit hyperactivity disorder. Cureus, 12(8), e9521. https://doi.org/10.7759/cureus.9521
Fanti, K. A., Eisenbarth, H., Goble, P., Demetriou, C., Kyranides, M. N., Goodwin, D., Zhang, J., Bobak, B., & Cortese, S. (2019). Psychophysiological activity and reactivity in children and adolescents with conduct problems: A systematic review and meta-analysis. Neuroscience & Biobehavioral Reviews, 100, 98–107. https://doi.org/10.1016/j.neubiorev.2019.02.016
Faraone, S. V., & Larsson, H. (2019). Genetics of attention deficit hyperactivity disorder. Molecular Psychiatry, 24(4), 562–575. https://doi.org/10.1038/s41380-018-0070-0
Faraone, S. V., Banaschewski, T., Coghill, D., Zheng, Y., Biederman, J., Bellgrove, M. A., Newcorn, J. H., Gignac, M., Al Saud, N. M., Manor, I., Rohde, L. A., Yang, L., Cortese, S., Almagor, D., Stein, M. A., Albatti, T. H., Aljoudi, H. F., Alqahtani, M. M. J., Asherson, P., et al. (2021). The World Federation of ADHD International Consensus Statement: 208 Evidence-based conclusions about the disorder. Neuroscience & Biobehavioral Reviews, 128, 789–818. https://doi.org/10.1016/j.neubiorev.2021.01.022
Fortier, M.-È., Sengupta, S. M., Grizenko, N., Choudhry, Z., Thakur, G., & Joober, R. (2013). Genetic evidence for the association of the hypothalamic-pituitary-adrenal (HPA) axis with ADHD and methylphenidate treatment response. NeuroMolecular Medicine, 15(1), 122–132. https://doi.org/10.1007/s12017-012-8202-1
Franke, B., Michelini, G., Asherson, P., Banaschewski, T., Bilbow, A., Buitelaar, J. K., Cormand, B., Faraone, S. V., Ginsberg, Y., Haavik, J., Kuntsi, J., Larsson, H., Lesch, K.-P., Ramos-Quiroga, J. A., Réthelyi, J. M., Ribases, M., & Reif, A. (2018). Live fast, die young? A review on the developmental trajectories of ADHD across the lifespan. European Neuropsychopharmacology: The Journal of the European College of Neuropsychopharmacology, 28(10), 1059–1088. https://doi.org/10.1016/j.euroneuro.2018.08.001
Geissler, J., Romanos, M., Hegerl, U., & Hensch, T. (2014). Hyperactivity and sensation seeking as autoregulatory attempts to stabilize brain arousal in ADHD and mania? Attention Deficit Hyperactivity Disorder, 6(3), 159–173. https://doi.org/10.1007/s12402-014-0144-z
Geva, R., & Feldman, R. (2008). A neurobiological model for the effects of early brainstem functioning on the development of behavior and emotion regulation in infants: Implications for prenatal and perinatal risk. Journal of Child Psychology and Psychiatry, 49(10), 1031–1041. https://doi.org/10.1111/j.1469-7610.2008.01918.x
Geva, R., Dital, A., Ramon, D., Yarmolovsky, J., Gidron, M., & Kuint, J. (2017). Brainstem as a developmental gateway to social attention. Journal of Child Psychology and Psychiatry, 58(12), 1351–1359. https://doi.org/10.1111/jcpp.12746
Gibbons, C. H. (2019). Basics of autonomic nervous system function. In K. H. Levin & P. Chauvel (Eds.), Handbook of clinical neurology (Vol. 160, pp. 407–418). Elsevier. https://doi.org/10.1016/B978-0-444-64032-1.00027-8
Gomez, I. N., Domondon, L. M., Tsang, H. W., Chan, C. C., & Lai, C. Y. (2021). Sensory behaviours and resting parasympathetic functions among children with and without ADHD. ScientificWorldJournal, 2021, 6615836. https://doi.org/10.1155/2021/6615836
Griffiths, K. R., Quintana, D. S., Hermens, D. F., Spooner, C., Tsang, T. W., Clarke, S., & Kohn, M. R. (2017). Sustained attention and heart rate variability in children and adolescents with ADHD. Biological Psychology, 124, 11–20. https://doi.org/10.1016/j.biopsycho.2017.01.004
Groeneveld, K. M., Mennenga, A. M., Heidelberg, R. C., Martin, R. E., Tittle, R. K., Meeuwsen, K. D., Walker, L. A., & White, E. K. (2019). Z-Score neurofeedback and heart rate variability training for adults and children with symptoms of attention-deficit/hyperactivity disorder: A retrospective study. Applied Psychophysiology and Biofeedback, 44(4), 291–308. https://doi.org/10.1007/s10484-019-09439-x
Hamrakova, A., Ondrejka, I., Sekaninova, N., Bona Olexova, L., Visnovcova, Z., Cesnekova, D., Hrtanek, I., Oppa, M., Hutka, P., & Tonhajzerova, I. (2020). Central autonomic regulation assessed by pupillary light reflex is impaired in children with attention deficit hyperactivity disorder. Physiological Research, 69(Suppl 3), S513–s521. https://doi.org/10.33549/physiolres.934589
Harteveld, L. M., Nederend, I., ten Harkel, A. D. J., Schutte, N. M., de Rooij, S. R., Vrijkotte, T. G. M., Oldenhof, H., Popma, A., Jansen, L. M. C., Suurland, J., Swaab, H., de Geus, E. J. C., Prätzlich, M., Ackermann, K., Baker, R., Batchelor, M., Baumann, S., Bernhard, A., Clanton, R., et al. (2021). Maturation of the cardiac autonomic nervous system activity in children and adolescents. Journal of the American Heart Association, 10(4), e017405. https://doi.org/10.1161/JAHA.120.017405
Hennissen, L., Bakker, M. J., Banaschewski, T., Carucci, S., Coghill, D., Danckaerts, M., Dittmann, R. W., Hollis, C., Kovshoff, H., McCarthy, S., Nagy, P., Sonuga-Barke, E., Wong, I. C., Zuddas, A., Rosenthal, E., & Buitelaar, J. K. (2017). Cardiovascular effects of stimulant and non-stimulant medication for children and adolescents with ADHD: A systematic review and meta-analysis of trials of methylphenidate, amphetamines and atomoxetine. CNS Drugs, 31(3), 199–215. https://doi.org/10.1007/s40263-017-0410-7
Howells, F. M., Stein, D. J., & Russell, V. A. (2012). Synergistic tonic and phasic activity of the locus coeruleus norepinephrine (LC-NE) arousal system is required for optimal attentional performance. Metabolic Brain Disease, 27(3), 267–274. https://doi.org/10.1007/s11011-012-9287-9
Idrees, I., Bellato, A., Cortese, S., & Groom, M. J. (2023). The effects of stimulant and non-stimulant medications on the autonomic nervous system (ANS) functioning in people with ADHD: A systematic review and meta-analysis. Neuroscience and Biobehavioral Reviews, 144, 104968. https://doi.org/10.1016/j.neubiorev.2022.104968
Imeraj, L., Antrop, I., Roeyers, H., Swanson, J., Deschepper, E., Bal, S., & Deboutte, D. (2012). Time-of-day effects in arousal: Disrupted diurnal cortisol profiles in children with ADHD. Journal of Child Psychology and Psychiatry, 53(7), 782–789. https://doi.org/10.1111/j.1469-7610.2012.02526.x
Isaksson, J., Nilsson, K. W., Nyberg, F., Hogmark, A., & Lindblad, F. (2012). Cortisol levels in children with attention-deficit/hyperactivity disorder. Journal of Psychiatric Research, 46(11), 1398–1405. https://doi.org/10.1016/j.jpsychires.2012.08.021
Isaksson, J., Nilsson, K. W., & Lindblad, F. (2013). Early psychosocial adversity and cortisol levels in children with attention-deficit/hyperactivity disorder. European Child & Adolescent Psychiatry, 22(7), 425–432. https://doi.org/10.1007/s00787-013-0383-0
Ito, W., Komada, Y., Okajima, I., & Inoue, Y. (2017). Excessive daytime sleepiness in adults with possible attention deficit/hyperactivity disorder (ADHD): A web-based cross-sectional study. Sleep Medicine, 32, 4–9. https://doi.org/10.1016/j.sleep.2016.04.008
James, S. N., Cheung, C. H. M., Rommel, A. S., McLoughlin, G., Brandeis, D., Banaschewski, T., Asherson, P., & Kuntsi, J. (2020). Peripheral hypoarousal but not preparation-vigilance impairment endures in ADHD remission. Journal of Attention Disorders, 24(13), 1944–1951. https://doi.org/10.1177/1087054717698813
Jennings, J. R., van der Molen, M. W., & Somsen, R. J. (1998). Changes in heart beat timing: reactivity resetting or perturbation? Biological Psychology, 47(3), 227–241. https://doi.org/10.1016/s0301-0511(97)00028-8
Jensen, C. M., & Steinhausen, H. C. (2015). Comorbid mental disorders in children and adolescents with attention-deficit/hyperactivity disorder in a large nationwide study. ADHD Attention Deficit and Hyperactivity Disorders, 7(1), 27–38. https://doi.org/10.1007/s12402-014-0142-1
Johnson, K. A., Wiersema, J. R., & Kuntsi, J. (2009). What would Karl Popper say? Are current psychological theories of ADHD falsifiable? Behavioral and Brain Functions, 5(1), 15. https://doi.org/10.1186/1744-9081-5-15
Johnston, B. A., Mwangi, B., Matthews, K., Coghill, D., Konrad, K., & Steele, J. D. (2014). Brainstem abnormalities in attention deficit hyperactivity disorder support high accuracy individual diagnostic classification. Human Brain Mapping, 35(10), 5179–5189. https://doi.org/10.1002/hbm.22542
Johnstone, S. J., Roodenrys, S., Phillips, E., Watt, A. J., & Mantz, S. (2010). A pilot study of combined working memory and inhibition training for children with AD/HD. Attention Deficit Hyperactivity Disorder, 2(1), 31–42. https://doi.org/10.1007/s12402-009-0017-z
Jones, B. E. (2003). Arousal systems. Frontiers in Bioscience, 8, s438–s451. https://doi.org/10.2741/1074
Kapp, S. K., Steward, R., Crane, L., Elliott, D., Elphick, C., Pellicano, E., & Russell, G. (2019). ‘People should be allowed to do what they like’: Autistic adults’ views and experiences of stimming. Autism, 23(7), 1782–1792. https://doi.org/10.1177/1362361319829628
Karemaker, J. M. (2017). An introduction into autonomic nervous function. Physiological Measurement, 38(5), R89–r118. https://doi.org/10.1088/1361-6579/aa6782
Karmiloff-Smith, A. (2009). Nativism versus neuroconstructivism: Rethinking the study of developmental disorders. Developmental Psychology, 45(1), 56–63. https://doi.org/10.1037/a0014506
Kenny, L., Hattersley, C., Molins, B., Buckley, C., Povey, C., & Pellicano, E. (2015). Which terms should be used to describe autism? Perspectives from the UK autism community. Autism, 20(4), 442–462. https://doi.org/10.1177/1362361315588200
Kharas, N., Reyes-Vazquez, C., & Dafny, N. (2017). Locus coeruleus neuronal activity correlates with behavioral response to acute and chronic doses of methylphenidate (Ritalin) in adolescent rats. Journal of Neural Transmission, 124(10), 1239–1250. https://doi.org/10.1007/s00702-017-1760-5
King, J. A., Barkley, R. A., & Barrett, S. (1998). Attention-deficit hyperactivity disorder and the stress response. Biological Psychiatry, 44(1), 72–74. https://doi.org/10.1016/S0006-3223(97)00507-6
Kleberg, J. L., Frick, M. A., & Brocki, K. C. (2020). Can auditory warning signals normalize eye movements in children with ADHD? European Child & Adolescent Psychiatry, 29(12), 1635–1644. https://doi.org/10.1007/s00787-020-01484-w
Kleberg, J. L., Frick, M. A., & Brocki, K. C. (2021). Increased pupil dilation to happy faces in children with hyperactive/impulsive symptoms of ADHD. Developmental Psychopathology, 33(3), 767–777. https://doi.org/10.1017/s0954579420000036
Koenig, J., Rash, J. A., Kemp, A. H., Buchhorn, R., Thayer, J. F., & Kaess, M. (2017). Resting state vagal tone in attention deficit (hyperactivity) disorder: A meta-analysis. World Journal of Biological Psychiatry, 18(4), 256–267. https://doi.org/10.3109/15622975.2016.1174300
Kofler, M. J., Rapport, M. D., Sarver, D. E., Raiker, J. S., Orban, S. A., Friedman, L. M., & Kolomeyer, E. G. (2013). Reaction time variability in ADHD: a meta-analytic review of 319 studies. Clinical Psychology Review, 33(6), 795–811. https://doi.org/10.1016/j.cpr.2013.06.001
Kofler, M. J., Raiker, J. S., Sarver, D. E., Wells, E. L., & Soto, E. F. (2016). Is hyperactivity ubiquitous in ADHD or dependent on environmental demands? Evidence from meta-analysis. Clinical Psychology Review, 46, 12–24. https://doi.org/10.1016/j.cpr.2016.04.004
Konrad, K., Neufang, S., Hanisch, C., Fink, G. R., & Herpertz-Dahlmann, B. (2006). Dysfunctional attentional networks in children with attention deficit/hyperactivity disorder: evidence from an event-related functional magnetic resonance imaging study. Biological Psychiatry, 59(7), 643–651. https://doi.org/10.1016/j.biopsych.2005.08.013
Kotov, R., Krueger, R. F., Watson, D., Achenbach, T. M., Althoff, R. R., Bagby, R. M., Brown, T. A., Carpenter, W. T., Caspi, A., Clark, L. A., Eaton, N. R., Forbes, M. K., Forbush, K. T., Goldberg, D., Hasin, D., Hyman, S. E., Ivanova, M. Y., Lynam, D. R., Markon, K., et al. (2017). The Hierarchical Taxonomy of Psychopathology (HiTOP): A dimensional alternative to traditional nosologies. Journal of Abnormal Psychology, 126(4), 454–477. https://doi.org/10.1037/abn0000258
Krahel, A., Paszynska, E., Slopien, A., Gawriolek, M., Otulakowska-Skrzynska, J., Rzatowski, S., Hernik, A., Hanć, T., Bryl, E., Szczesniewska, P., Bilska, K., Duda, J., Tyszkiewicz-Nwafor, M., & Dmitrzak-Weglarz, M. (2021). Stress/immune biomarkers in saliva among children with ADHD status. International Journal of Environmental Research and Public Health, 18(2). https://doi.org/10.3390/ijerph18020769
Kuntsi, J., & Klein, C. (2012). Intraindividual variability in ADHD and its implications for research of causal links. Current Topics in Behavioral Neurosciences, 9, 67–91. https://doi.org/10.1007/7854_2011_145
Kutscheidt, K., Dresler, T., Hudak, J., Barth, B., Blume, F., Ethofer, T., Fallgatter, A. J., & Ehlis, A. C. (2019). Interoceptive awareness in patients with attention-deficit/hyperactivity disorder (ADHD). Attention Deficit Hyperactivity Disorder, 11(4), 395–401. https://doi.org/10.1007/s12402-019-00299-3
Kvadsheim, E., Fasmer, O. B., Osnes, B., Koenig, J., Adolfsdottir, S., Eichele, H., Plessen, K. J., & Sørensen, L. (2020). Lower cardiac vagal activity predicts self-reported difficulties with emotion regulation in adolescents with ADHD. Frontiers in Psychiatry, 11, 244. https://doi.org/10.3389/fpsyt.2020.00244
Kvadsheim, E., Fasmer, O. B., Fasmer, E. E., Hauge, E. R., Thayer, J. F., Osnes, B., Haavik, J., Koenig, J., Adolfsdottir, S., Plessen, K. J., & Sørensen, L. (2022). Innovative approaches in investigating inter-beat intervals: Graph theoretical method suggests altered autonomic functioning in adolescents with ADHD. Psychophysiology, e14005. https://doi.org/10.1111/psyp.14005
Lacey, J. I. (1967). Somatic response patterning and stress: Some revisions of activation theory. In M. H. Appley & R. Trumbull (Eds.), Psychological stress: Issues in research (pp. 14-42). : Appleton-Century-Crofts.
Laitio, T., Jalonen, J., Kuusela, T., & Scheinin, H. (2007). The role of heart rate variability in risk stratification for adverse postoperative cardiac events. Anesthesia & Analgesia, 105(6), 1548–1560. https://doi.org/10.1213/01.ane.0000287654.49358.3a
Leitner, Y. (2014). The co-occurrence of autism and attention deficit hyperactivity disorder in children – What do we know? Frontiers in Human Neuroscience, 8, 268. https://doi.org/10.3389/fnhum.2014.00268
Liang, E. F., Lim, S. Z., Tam, W. W., Ho, C. S., Zhang, M. W., McIntyre, R. S., & Ho, R. C. (2018). The effect of methylphenidate and atomoxetine on heart rate and systolic blood pressure in young people and adults with Attention-Deficit Hyperactivity Disorder (ADHD): Systematic review, meta-analysis, and meta-regression. International Journal of Environmental Research and Public Health, 15(8). https://doi.org/10.3390/ijerph15081789
Libby, W. L., Jr., Lacey, B. C., & Lacey, J. I. (1973). Pupillary and cardiac activity during visual attention. Psychophysiology, 10(3), 270–294. https://doi.org/10.1111/j.1469-8986.1973.tb00526.x
Ludyga, S., Gerber, M., Mücke, M., Brand, S., Weber, P., Brotzmann, M., & Pühse, U. (2020). The acute effects of aerobic exercise on cognitive flexibility and task-related heart rate variability in children with ADHD and healthy controls. Journal of Attention Disorders, 24(5), 693–703. https://doi.org/10.1177/1087054718757647
Lydon, S., Healy, O., Reed, P., Mulhern, T., Hughes, B. M., & Goodwin, M. S. (2016). A systematic review of physiological reactivity to stimuli in autism. Developmental Neurorehabilitation, 19(6), 335–355. https://doi.org/10.3109/17518423.2014.971975
Madjar, N., Gazoli, R., Manor, I., & Shoval, G. (2020). Contrasting effects of music on reading comprehension in preadolescents with and without ADHD. Psychiatry Research, 291, 113207. https://doi.org/10.1016/j.psychres.2020.113207
Martella, D., Aldunate, N., Fuentes, L. J., & Sánchez-Pérez, N. (2020). Arousal and executive alterations in Attention Deficit Hyperactivity Disorder (ADHD) [Mini Review]. Frontiers in Psychology, 11. https://doi.org/10.3389/fpsyg.2020.01991
Mather, M., Clewett, D., Sakaki, M., & Harley, C. W. (2016). Norepinephrine ignites local hotspots of neuronal excitation: How arousal amplifies selectivity in perception and memory. Behavioral and Brain Sciences, 39, e200. https://doi.org/10.1017/S0140525X15000667
McKlveen, J. M., Myers, B., & Herman, J. P. (2015). The medial prefrontal cortex: Coordinator of autonomic, neuroendocrine and behavioural responses to stress. Journal of Neuroendocrinology, 27(6), 446–456. https://doi.org/10.1111/jne.12272
McQuade, J. D., & Breaux, R. P. (2017). Are elevations in ADHD symptoms associated with physiological reactivity and emotion dysregulation in children? Journal of Abnormal Child Psychology, 45(6), 1091–1103. https://doi.org/10.1007/s10802-016-0227-8
McQuade, J. D., Dixon-Gordon, K. L., Breaux, R., & Babinski, D. E. (2022). Interactive effects of parent emotion socialization and child physiological reactivity in predicting adolescent borderline personality disorder features. Research on Child and Adolescent Psychopathology, 50(1), 89–100. https://doi.org/10.1007/s10802-020-00717-5
Mefford, I. N., & Potter, W. Z. (1989). A neuroanatomical and biochemical basis for attention deficit disorder with hyperactivity in children: A defect in tonic adrenaline mediated inhibition of locus coeruleus stimulation. Medical Hypotheses, 29(1), 33–42. https://doi.org/10.1016/0306-9877(89)90164-3
Metin, B., Roeyers, H., Wiersema, J. R., van der Meere, J., & Sonuga-Barke, E. (2012). A meta-analytic study of event rate effects on Go/No-Go performance in attention-deficit/hyperactivity disorder. Biological Psychiatry, 72(12), 990–996. https://doi.org/10.1016/j.biopsych.2012.08.023
Metin, B., Krebs, R. M., Wiersema, J. R., Verguts, T., Gasthuys, R., van der Meere, J. J., Achten, E., Roeyers, H., & Sonuga-Barke, E. (2015). Dysfunctional modulation of default mode network activity in attention-deficit/hyperactivity disorder. Journal of Abnormal Psychology, 124(1), 208–214. https://doi.org/10.1037/abn0000013
Metin, B., Wiersema, J. R., Verguts, T., Gasthuys, R., van Der Meere, J. J., Roeyers, H., & Sonuga-Barke, E. (2016). Event rate and reaction time performance in ADHD: Testing predictions from the state regulation deficit hypothesis using an ex-Gaussian model. Child Neuropsychology, 22(1), 99–109.
Meyer, T., Becker, A., Sundermann, J., Rothenberger, A., & Herrmann-Lingen, C. (2017). Attention deficit-hyperactivity disorder is associated with reduced blood pressure and serum vitamin D levels: Results from the nationwide German Health Interview and Examination Survey for Children and Adolescents (KiGGS). European Child & Adolescent Psychiatry, 26(2), 165–175. https://doi.org/10.1007/s00787-016-0852-3
Miller, N., & Prevatt, F. (2020). Redefining ADHD using an adult population: Should inattention be viewed as a separate dimension from cognitive and physiological activity level? Journal of Attention Disorders, 24(14), 1977–1988. https://doi.org/10.1177/1087054717733045
Molina, R., Redondo, B., Molina-Carballo, A., García, J. A., Muñoz-Hoyos, A., Vera, J., & Jiménez, R. (2021). Capturing attention improves accommodation: An experimental study in children with ADHD using multiple object tracking. Vision Research, 186, 52–58. https://doi.org/10.1016/j.visres.2021.05.002
Morris, S. S. J., Musser, E. D., Tenenbaum, R. B., Ward, A. R., Martinez, J., Raiker, J. S., Coles, E. K., & Riopelle, C. (2020). Emotion regulation via the autonomic nervous system in children with Attention-Deficit/Hyperactivity Disorder (ADHD): Replication and extension. Journal of Abnormal Child Psychology, 48(3), 361–373. https://doi.org/10.1007/s10802-019-00593-8
Morris, S. S. J., Musser, E. D., Tenenbaum, R. B., Ward, A. R., Raiker, J. S., & Coles, E. K. (2021). Methylphenidate improves autonomic functioning among youth with attention-deficit/hyperactivity disorder. Research on Child and Adolescent Psychopathology. https://doi.org/10.1007/s10802-021-00870-5
Mulkey, S. B., & du Plessis, A. J. (2019). Autonomic nervous system development and its impact on neuropsychiatric outcome. Pediatric Research, 85(2), 120–126. https://doi.org/10.1038/s41390-018-0155-0
Murphy, P. R., O’Connell, R. G., O’Sullivan, M., Robertson, I. H., & Balsters, J. H. (2014). Pupil diameter covaries with BOLD activity in human locus coeruleus. Human Brain Mapping, 35(8), 4140–4154. https://doi.org/10.1002/hbm.22466
Musser, E. D., & Nigg, J. T. (2019). Emotion dysregulation across emotion systems in attention deficit/hyperactivity disorder. Journal of Clinical Child & Adolescent Psychology, 48(1), 153–165. https://doi.org/10.1080/15374416.2016.1270828
Musser, E. D., Backs, R. W., Schmitt, C. F., Ablow, J. C., Measelle, J. R., & Nigg, J. T. (2011). Emotion regulation via the autonomic nervous system in children with attention-deficit/hyperactivity disorder (ADHD). Journal of Abnormal Child Psychology, 39(6), 841–852. https://doi.org/10.1007/s10802-011-9499-1
Musser, E. D., Galloway-Long, H. S., Frick, P. J., & Nigg, J. T. (2013). Emotion regulation and heterogeneity in attention-deficit/hyperactivity disorder. Journal of the American Academy of Child & Adolescent Psychiatry, 52(2), 163–171.e162. https://doi.org/10.1016/j.jaac.2012.11.009
Nada, P. J. (2009). Heart rate variability in the assessment and biofeedback training of common mental health problems in children. Medical Archives, 63(5), 244–248.
Nobukawa, S., Shirama, A., Takahashi, T., Takeda, T., Ohta, H., Kikuchi, M., Iwanami, A., Kato, N., & Toda, S. (2021). Identification of attention-deficit hyperactivity disorder based on the complexity and symmetricity of pupil diameter. Scientific Reports, 11(1), 8439. https://doi.org/10.1038/s41598-021-88191-x
O’Connell, R. G., Bellgrove, M. A., Dockree, P. M., Lau, A., Fitzgerald, M., & Robertson, I. H. (2008). Self-Alert Training: Volitional modulation of autonomic arousal improves sustained attention. Neuropsychologia, 46(5), 1379–1390. https://doi.org/10.1016/j.neuropsychologia.2007.12.018
Orekhova, E. V., & Stroganova, T. A. (2014). Arousal and attention re-orienting in autism spectrum disorders: Evidence from auditory event-related potentials. Frontiers in Human Neuroscience, 8, 34. https://doi.org/10.3389/fnhum.2014.00034
Paulus, F. W., Ohmann, S., Möhler, E., Plener, P., & Popow, C. (2021). Emotional dysregulation in children and adolescents with psychiatric disorders. A narrative review. Frontiers in Psychiatry, 12, 628252. https://doi.org/10.3389/fpsyt.2021.628252
Payen, A., Chen, M. J., Carter, T. G., Kilmer, R. P., & Bennett, J. M. (2022). Childhood ADHD, going beyond the brain: A meta-analysis on peripheral physiological markers of the heart and the gut [Systematic Review]. Frontiers in Endocrinology, 13. https://www.frontiersin.org/article/10.3389/fendo.2022.738065
Pliszka, S. R., McCracken, J. T., & Maas, J. W. (1996). Catecholamines in attention-deficit hyperactivity disorder: current perspectives. Journal of the American Academy of Child and Adolescent Psychiatry, 35(3), 264–272. https://doi.org/10.1097/00004583-199603000-00006
Porges, S. W. (2007). The polyvagal perspective. Biological Psychology, 74(2), 116–143. https://doi.org/10.1016/j.biopsycho.2006.06.009
Porges, S. W. (2009). The polyvagal theory: New insights into adaptive reactions of the autonomic nervous system. Cleveland Clinic Journal of Medicine, 76(Suppl 2), S86–S90. https://doi.org/10.3949/ccjm.76.s2.17
Posner, J., Polanczyk, G. V., & Sonuga-Barke, E. (2020). Attention-deficit hyperactivity disorder. Lancet, 395(10222), 450–462. https://doi.org/10.1016/s0140-6736(19)33004-1
Quadt, L., Critchley, H., & Nagai, Y. (2022). Cognition, emotion, and the central autonomic network. Autonomic Neuroscience: Basic and Clinical, 238, 102948. https://doi.org/10.1016/j.autneu.2022.102948
Ramos-Quiroga, J. A., Corominas-Roso, M., Palomar, G., Ferrer, R., Valero, S., Corrales, M., Richarte, V., & Casas, M. (2016). Cortisol awakening response in adults with attention deficit hyperactivity disorder: Subtype differences and association with the emotional lability. European Neuropsychopharmacology, 26(7), 1140–1149. https://doi.org/10.1016/j.euroneuro.2016.03.014
Rash, J. A., & Aguirre-Camacho, A. (2012). Attention-deficit hyperactivity disorder and cardiac vagal control: A systematic review. Attention Deficit Hyperactivity Disorder, 4(4), 167–177. https://doi.org/10.1007/s12402-012-0087-1
Redondo, B., Vera, J., Molina, R., Garcia, J. A., Catena, A., Muñoz-Hoyos, A., & Jimenez, R. (2020). Accommodation and pupil dynamics as potential objective predictors of behavioural performance in children with attention-deficit/hyperactivity disorder. Vision Research, 175, 32–40. https://doi.org/10.1016/j.visres.2020.06.005
Robe, A., Dobrean, A., Cristea, I. A., Păsărelu, C. R., & Predescu, E. (2019). Attention-deficit/hyperactivity disorder and task-related heart rate variability: A systematic review and meta-analysis. Neuroscience & Biobehavioral Reviews, 99, 11–22. https://doi.org/10.1016/j.neubiorev.2019.01.022
Robe, A., Păsărelu, C. R., & Dobrean, A. (2021). Exploring autonomic regulation in children with ADHD with and without comorbid anxiety disorder through three systematic levels of cardiac vagal control analysis: Rest, reactivity, and recovery. Psychophysiology, 58(9), e13850. https://doi.org/10.1111/psyp.13850
Rowe, D. L., Robinson, P. A., & Gordon, E. (2005). Stimulant drug action in attention deficit hyperactivity disorder (ADHD): Inference of neurophysiological mechanisms via quantitative modelling. Clinical Neurophysiology, 116(2), 324–335. https://doi.org/10.1016/j.clinph.2004.08.001
Rubia, K., Alegría, A. A., & Brinson, H. (2014). Brain abnormalities in attention-deficit hyperactivity disorder: A review. Revue Neurologique, 58(Suppl 1), S3–S16.
Samuels, R. E., & Szabadi, E. (2008). Functional neuroanatomy of the noradrenergic locus coeruleus: Its roles in the regulation of arousal and autonomic function part I: Principles of functional organisation. Current Neuropharmacology, 6(3), 235–253. https://doi.org/10.2174/157015908785777229
Sander, C., Hensch, T., Wittekind, D. A., Böttger, D., & Hegerl, U. (2015). Assessment of wakefulness and brain arousal regulation in psychiatric research. Neuropsychobiology, 72(3-4), 195–205. https://doi.org/10.1159/000439384
Sanders, A. F. (1983). Towards a model of stress and human performance. Acta Psychologica, 53(1), 61–97. https://doi.org/10.1016/0001-6918(83)90016-1
Sandgren, A. M., & Brummer, R. J. M. (2018). ADHD-originating in the gut? The emergence of a new explanatory model. Medical Hypotheses, 120, 135–145. https://doi.org/10.1016/j.mehy.2018.08.022
Sara, S. J., & Bouret, S. (2012). Orienting and reorienting: The locus coeruleus mediates cognition through arousal. Neuron, 76(1), 130–141. https://doi.org/10.1016/j.neuron.2012.09.011
Sarchiapone, M., Gramaglia, C., Iosue, M., Carli, V., Mandelli, L., Serretti, A., Marangon, D., & Zeppegno, P. (2018). The association between electrodermal activity (EDA), depression and suicidal behaviour: A systematic review and narrative synthesis. BMC Psychiatry, 18(1), 22. https://doi.org/10.1186/s12888-017-1551-4
Sarver, D. E., Rapport, M. D., Kofler, M. J., Raiker, J. S., & Friedman, L. M. (2015). Hyperactivity in Attention-Deficit/Hyperactivity Disorder (ADHD): Impairing deficit or compensatory behavior? Journal of Abnormal Child Psychology, 43(7), 1219–1232. https://doi.org/10.1007/s10802-015-0011-1
Sayer, G. R., McGough, J. J., Levitt, J., Cowen, J., Sturm, A., Castelo, E., & McCracken, J. T. (2016). Acute and long-term cardiovascular effects of stimulant, guanfacine, and combination therapy for attention-deficit/hyperactivity disorder. Journal of Child and Adolescent Psychopharmacology, 26(10), 882–888. https://doi.org/10.1089/cap.2015.0264
Schloß, S., Derz, F., Schurek, P., Cosan, A. S., Becker, K., & Pauli-Pott, U. (2021). Reward-related dysfunctions in children developing attention deficit hyperactivity disorder-roles of oppositional and callous-unemotional symptoms. Frontiers in Psychiatry, 12, 738368. https://doi.org/10.3389/fpsyt.2021.738368
Schulz, J., Huber, F., Schlack, R., Hölling, H., Ravens-Sieberer, U., Meyer, T., Poustka, L., Rothenberger, A., Wang, B., & Becker, A. (2021). The association between low blood pressure and Attention-Deficit Hyperactivity Disorder (ADHD) observed in children/adolescents does not persist into young adulthood. A population-based ten-year follow-up study. International Journal of Environmental Research and Public Health, 18(4). https://doi.org/10.3390/ijerph18041864
Sergeant, J. (2000). The cognitive-energetic model: An empirical approach to attention-deficit hyperactivity disorder. Neuroscience & Biobehavioral Reviews, 24(1), 7–12. https://doi.org/10.1016/s0149-7634(99)00060-3
Sergeant, J. A. (2005). Modeling attention-deficit/hyperactivity disorder: A critical appraisal of the cognitive-energetic model. Biological Psychiatry, 57(11), 1248–1255. https://doi.org/10.1016/j.biopsych.2004.09.010
Shaffer, F., & Ginsberg, J. P. (2017). An overview of heart rate variability metrics and norms. Frontiers in Public Health, 5, 258–258. https://doi.org/10.3389/fpubh.2017.00258
Shaw, P., Stringaris, A., Nigg, J., & Leibenluft, E. (2014). Emotion dysregulation in attention deficit hyperactivity disorder. American Journal of Psychiatry, 171(3), 276–293. https://doi.org/10.1176/appi.ajp.2013.13070966
Shirama, A., Takeda, T., Ohta, H., Iwanami, A., Toda, S., & Kato, N. (2020). Atypical alert state control in adult patients with ADHD: A pupillometry study. PLoS One, 15(12), e0244662. https://doi.org/10.1371/journal.pone.0244662
Snoek, H., Van Goozen, S. H., Matthys, W., Buitelaar, J. K., & van Engeland, H. (2004). Stress responsivity in children with externalizing behavior disorders. Developmental Psychopathology, 16(2), 389–406. https://doi.org/10.1017/s0954579404044578
Sonuga-Barke, E. J., Wiersema, J. R., van der Meere, J. J., & Roeyers, H. (2010). Context-dependent dynamic processes in attention deficit/hyperactivity disorder: Differentiating common and unique effects of state regulation deficits and delay aversion. Neuropsychology Review, 20(1), 86–102. https://doi.org/10.1007/s11065-009-9115-0
Souroulla, A. V., Panteli, M., Robinson, J. D., & Panayiotou, G. (2019). Valence, arousal or both? Shared emotional deficits associated with attention deficit and hyperactivity disorder and oppositional/defiant-conduct disorder symptoms in school-aged youth. Biological Psychology, 140, 131–140. https://doi.org/10.1016/j.biopsycho.2018.11.007
Storebø, O. J., Krogh, H. B., Ramstad, E., Moreira-Maia, C. R., Holmskov, M., Skoog, M., Nilausen, T. D., Magnusson, F. L., Zwi, M., Gillies, D., Rosendal, S., Groth, C., Rasmussen, K. B., Gauci, D., Kirubakaran, R., Forsbøl, B., Simonsen, E., & Gluud, C. (2015). Methylphenidate for attention-deficit/hyperactivity disorder in children and adolescents: Cochrane systematic review with meta-analyses and trial sequential analyses of randomised clinical trials. BMJ, 351, h5203. https://doi.org/10.1136/bmj.h5203
Sukmajaya, A. C., Lusida, M. I., & Soetjipto, & Setiawati, Y. (2021). Systematic review of gut microbiota and attention-deficit hyperactivity disorder (ADHD). Annals of General Psychiatry, 20(1), 12. https://doi.org/10.1186/s12991-021-00330-w
Taskiran, C., Karaismailoglu, S., Cak Esen, H. T., Tuzun, Z., Erdem, A., Balkanci, Z. D., Dolgun, A. B., & Cengel Kultur, S. E. (2018). Clinical features and subjective/physiological responses to emotional stimuli in the presence of emotion dysregulation in attention-deficit hyperactivity disorder. Journal of Clinical and Experimental Neuropsychology, 40(4), 389–404. https://doi.org/10.1080/13803395.2017.1353952
Tenenbaum, R. B., Musser, E. D., Raiker, J. S., Coles, E. K., Gnagy, E. M., & Pelham, W. E., Jr. (2018). Specificity of reward sensitivity and parasympathetic-based regulation among children with attention-deficit/hyperactivity and disruptive behavior disorders. Journal of Abnormal Child Psychology, 46(5), 965–977. https://doi.org/10.1007/s10802-017-0343-0
Tenenbaum, R. B., Musser, E. D., Morris, S., Ward, A. R., Raiker, J. S., Coles, E. K., & Pelham, W. E., Jr. (2019). Response inhibition, response execution, and emotion regulation among children with attention-deficit/hyperactivity disorder. Journal of Abnormal Child Psychology, 47(4), 589–603. https://doi.org/10.1007/s10802-018-0466-y
Thayer, J. F., & Lane, R. D. (2000). A model of neurovisceral integration in emotion regulation and dysregulation. Journal of Affective Disorders, 61(3), 201–216. https://doi.org/10.1016/s0165-0327(00)00338-4
Thayer, J. F., Åhs, F., Fredrikson, M., Sollers, J. J., & Wager, T. D. (2012). A meta-analysis of heart rate variability and neuroimaging studies: Implications for heart rate variability as a marker of stress and health. Neuroscience & Biobehavioral Reviews, 36(2), 747–756. https://doi.org/10.1016/j.neubiorev.2011.11.009
Toichi, M., Sugiura, T., Murai, T., & Sengoku, A. (1997). A new method of assessing cardiac autonomic function and its comparison with spectral analysis and coefficient of variation of R-R interval. Journal of the Autonomic Nervous System, 62(1-2), 79–84. https://doi.org/10.1016/s0165-1838(96)00112-9
Tursky, B., Shapiro, D., Crider, A., & Kahneman, D. (1969). Pupillary, heart rate, and skin resistance changes during a mental task. Journal of Experimental Psychology: General, 79(1), 164–167. https://doi.org/10.1037/h0026952
Tye, C., Asherson, P., Ashwood, K. L., Azadi, B., Bolton, P., & McLoughlin, G. (2014). Attention and inhibition in children with ASD, ADHD and co-morbid ASD + ADHD: an event-related potential study. Psychological Medicine, 44(5), 1101–1116. https://doi.org/10.1017/S0033291713001049
Van Cauwenberge, V., El Kaddouri, R., Hoppenbrouwers, K., & Wiersema, J. R. (2017). To make a molehill out of a mountain: An ERP-study on cognitive reappraisal of negative pictures in children with and without ADHD. Clinical Neurophysiology, 128(4), 529–537. https://doi.org/10.1016/j.clinph.2017.01.008
van der Meere, J. (2005). State regulation and attention deficit hyperactivity disorder. In D. Gozal & D. L. Molfese (Eds.), Attention deficit hyperactivity disorder: From genes to patients (pp. 413–433). Humana Press. https://doi.org/10.1385/1-59259-891-9:413
Van der Meere, J., & Sergeant, J. A. (1988). Controlled processing and vigilance in hyperactivity: Time will tell. Journal of Abnormal Child Psychology, 16(6), 641–655. https://doi.org/10.1007/BF00913475
van der Meere, J. J., Shalev, R. S., Borger, N., & Wiersema, J. R. (2009). Methylphenidate, interstimulus interval, and reaction time performance of children with attention deficit/hyperactivity disorder: A pilot study. Child Neuropsychology, 15(6), 554–566. https://doi.org/10.1080/09297040902758803
van der Meere, J. J., Börger, N. A., & Wiersema, J. R. (2010). ADHD: State regulation and motivation. Current Medical Literature. Psychiatry, 21(1), 14–20.
van Lang, N. D., Tulen, J. H., Kallen, V. L., Rosbergen, B., Dieleman, G., & Ferdinand, R. F. (2007). Autonomic reactivity in clinically referred children attention-deficit/hyperactivity disorder versus anxiety disorder. European Child & Adolescent Psychiatry, 16(2), 71–78. https://doi.org/10.1007/s00787-006-0575-y
Vélez-Galarraga, R., Guillén-Grima, F., Crespo-Eguílaz, N., & Sánchez-Carpintero, R. (2016). Prevalence of sleep disorders and their relationship with core symptoms of inattention and hyperactivity in children with attention-deficit/hyperactivity disorder. European Journal of Paediatric Neurology, 20(6), 925–937. https://doi.org/10.1016/j.ejpn.2016.07.004
Wang, T. S., Huang, W. L., Kuo, T. B., Lee, G. S., & Yang, C. C. (2013). Inattentive and hyperactive preschool-age boys have lower sympathetic and higher parasympathetic activity. Journal of Physiological Sciences, 63(2), 87–94. https://doi.org/10.1007/s12576-012-0238-3
Wang, X., Piñol, R. A., Byrne, P., & Mendelowitz, D. (2014). Optogenetic stimulation of locus ceruleus neurons augments inhibitory transmission to parasympathetic cardiac vagal neurons via activation of brainstem α1 and β1 receptors. Journal of Neuroscience, 34(18), 6182–6189. https://doi.org/10.1523/jneurosci.5093-13.2014
Wang, C.-A., Baird, T., Huang, J., Coutinho, J. D., Brien, D. C., & Munoz, D. P. (2018). Arousal effects on pupil size, heart rate, and skin conductance in an emotional face task [Original research]. Frontiers in Neurology, 9. https://doi.org/10.3389/fneur.2018.01029
Waxenbaum, J. A., Reddy, V., & Varacallo, M. (2022). Anatomy, autonomic nervous system. In StatPearls. StatPearls Publishing.
Wehrwein, E. A., Orer, H. S., & Barman, S. M. (2016). Overview of the anatomy, physiology, and pharmacology of the autonomic nervous system. Comprehensive Physiology, 6(3), 1239–1278. https://doi.org/10.1002/cphy.c150037
Wiersema, J. R., & Godefroid, E. (2018). Interoceptive awareness in attention deficit hyperactivity disorder. PLoS One, 13(10), e0205221. https://doi.org/10.1371/journal.pone.0205221
Wiersema, R., van der Meere, J., Antrop, I., & Roeyers, H. (2006a). State regulation in adult ADHD: an event-related potential study. Journal of Clinical and Experimental Neuropsychology, 28(7), 1113–1126. https://doi.org/10.1080/13803390500212896
Wiersema, R., Van Der Meere, J., Roeyers, H., Van, C. R., & Baeyens, D. (2006b). Event rate and event-related potentials in ADHD. Journal of Child Psychology and Psychiatry, 47(6), 560–567. https://doi.org/10.1111/j.1469-7610.2005.01592.x
Willcutt, E. G., Doyle, A. E., Nigg, J. T., Faraone, S. V., & Pennington, B. F. (2005). Validity of the executive function theory of attention-deficit/hyperactivity disorder: A meta-analytic review. Biological Psychiatry, 57(11), 1336–1346. https://doi.org/10.1016/j.biopsych.2005.02.006
Yerkes, R. M., & Dodson, J. D. (1908). The relation of strength of stimulus to rapidity of habit-formation. Journal of Comparative Neurology and Psychology, 18(5), 459–482. https://doi.org/10.1002/cne.920180503
Yu, C. L., Hsieh, S. S., Chueh, T. Y., Huang, C. J., Hillman, C. H., & Hung, T. M. (2020). The effects of acute aerobic exercise on inhibitory control and resting state heart rate variability in children with ADHD. Scientific Reports, 10(1), 19958. https://doi.org/10.1038/s41598-020-76859-9
Yung, T. W. K., Lai, C. Y. Y., Chan, J. Y. C., Ng, S. S. M., & Chan, C. C. H. (2020). Neuro-physiological correlates of sluggish cognitive tempo (SCT) symptoms in school-aged children. European Child & Adolescent Psychiatry, 29(3), 315–326. https://doi.org/10.1007/s00787-019-01353-1
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2023 The Author(s), under exclusive license to Springer Nature Switzerland AG
About this chapter
Cite this chapter
Bellato, A., Wiersema, J.R., Groom, M.J. (2023). Autonomic Nervous System Functioning in ADHD. In: Matson, J.L. (eds) Clinical Handbook of ADHD Assessment and Treatment Across the Lifespan. Autism and Child Psychopathology Series. Springer, Cham. https://doi.org/10.1007/978-3-031-41709-2_3
Download citation
DOI: https://doi.org/10.1007/978-3-031-41709-2_3
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-031-41708-5
Online ISBN: 978-3-031-41709-2
eBook Packages: Behavioral Science and PsychologyBehavioral Science and Psychology (R0)