Abstract
The surgery of the biceps brachii anchors the tendon to the bone, usually using sutures and/or screws. The usual technique is to drill a tunnel in the radius and secure the tendon in it using a small metal piece (button). However, it is also possible to add an interference screw in the bone tunnel to increase the fixation capacity. The objective of this work has been to evaluate the improvement of the repair of the biceps brachii tendon with the use of an interference screw. To this end, reconstructions of the distal tendon were carried out using bones and tendons of animal origin and tested cyclically. The results indicate that adding the screw reduces the displacement and increases the loading capacity significantly. Therefore, the addition of the interference screw is recommended, especially in young and active patients.
You have full access to this open access chapter, Download conference paper PDF
Similar content being viewed by others
Keywords
1 Introduction
Distal biceps brachii tendon rupture is not uncommon and most orthopedic surgeons have to deal with this problem at least a few times a year. Clinical units specialized in upper limb surgery treat this injury several times a month. Approximately 90% of all patients are men, between 35- and 50-year-old, with an incidence of 2.5 in 100,000 per year. Usually, it is a sudden eccentric load, rather than a repetitive or heavy load, that causes failure of the anatomic insertion of the tendon. Patients report a sudden pain, often with a pop.
The biceps brachii muscle plays a crucial role in the ability to lift, rotate, and move the upper arm. It is attached to the elbow and shoulder by tendons that, if torn, significantly reduce the strength of the upper arm and its movements can become painful. A distal biceps tendon rupture is the injury that occurs in the elbow joint. Most people who suffer from this injury require surgery to correct it. The objective of the surgery is to re-anchor the tendon to the bone, normally using sutures and/or screws.
The most recommended technique is to perform a bone tunnel in the radius and secure the tendon in with a small metal piece, a button, on the other side of the tunnel [1, 2]. Many biomechanical studies have studied distal biceps brachii tendon repair and there is relative consensus regarding the suitability of the button system [1,2,3,4,5,6,7,8,9,10,11].
However, it is possible not only to use the techniques separately, but to combine them. Specifically, it is also possible to add an interference screw in the bone tunnel when using the button technique, to increase fixation capacity, but this possibility, to the best of our knowledge, has not been biomechanically assessed.
The objective of this work has been to evaluate the biomechanical improvement of the distal biceps brachii tendon repair when introducing an interferential screw in the bone tunnel practiced in the button technique, which we will call the hybrid technique. For this purpose, reconstructions of the distal tendon were carried out using porcine bones and tendons, and cyclical tensile tests were carried out simulating the immediate rehabilitation period after surgery.
2 Methodology
2.1 Materials
Twenty bovine digital extensor tendons and the same number of porcine tibiae were used. Due to the difficulty of obtaining human cadaveric tendons and bones, it has been decided to use animal tissues. Furthermore, this reduces the variability inherent in biological samples, since equal tendon diameters and lengths can be easily selected.
Tendons were removed from bovine legs obtained from a local slaughterhouse and all adjacent tissues were cleaned. A tendon caliper was used to select only the 7 mm diameter tendons. Subsequently, each tendon was wrapped in gauze soaked in saline solution for its conservation, placed in a plastic bag and kept frozen at a temperature of −20 °C until the tests were carried out.
Porcine tibiae, mimicking the human radius, were obtained from a local butcher shop, and cleaned of surrounding soft tissue. Only tibiae with a diaphyseal diameter of about 20 mm were used. Subsequently, they were preserved under the same conditions as the tendons. Twelve hours prior to the tests, tissues were thawed at room temperature.
Ten distal bicep tendon reconstruction were performed for each of the two techniques tested. In the first group, the reconstruction was performed using only the suture (FiberLoop® Nº2) and the button (BicepsButton®, 2.6 × 12 mm), both from Arthrex (FL, USA), and in the second group it was also added the interference screw (7 mm × 10 mm PEEK tenodesis screw) from the same company. The button is made of surgical titanium (Ti6Al4V) and the screw is made of PEEK (polyetheretherketone). We have called the first group the “button technique” and the second group the “hybrid technique”.
2.2 Testing Protocol
Each of the 20 reconstructions were tested in a universal testing machine (Microtest EFH/5/FR, Madrid, Spain). A custom made fixation system for the tibia was used to secure its rigid anchorage to the testing machine and to achieve its correct positioning, placing the bone tunnel in the tensile direction, the worst-case load scenario in clinical practice. The proximal end of the graft was fixed to the machine crosshead by a jaw designed to prevent slippage of the tendon during the test (Fig. 1).
After correct positioning, and before proceeding to the tensile test, an initial preload of 30 N for 2 min was applied. The reconstruction was then subjected to 1,000 load cycles between 10 and 50 N at 0.5 Hz. Once these cycles were completed, it was again preloaded to 55 N for another 2 min, followed by another 1,000 load cycles between 10 and 100 N at 0.5 Hz. Immediately after the second part of the cyclical test, the specimen was subjected to a tensile test until failure at a 20 mm/min rate, simulating the reconstruction failure caused by a traumatic overload.
During all the test, the tendon was kept wet with nebulized saline solution, to avoid dehydration, keeping its mechanical properties throughout the test. At the end of the test, all the specimens were inspected, and the failure mode was recorded, classifying them as: a) tearing of the tendon due to the suture; b) loosening of the knot; and c) rupture of the tendon adjacent to the screw.
2.3 Data Analysis
The force and displacement data were obtained with the sensors and software of the testing machine. The stiffness for each cycle is calculated as the slope of the line that best fits the complete cycle by the method of least squares in the force–displacement graph. The stiffness of the final part of the test (failure) was obtained as the slope of the line of best fit of the final part of the test.
The results of both groups were compared using a Student's t-test for two independent samples (significant difference p < 0.05). Previously, a normality analysis was performed with the Shapiro–Wilk test because there were fewer than 30 samples. The results indicated that there was no evidence to reject the normality of the data.
3 Results
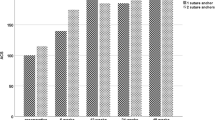
Table 1 shows the values obtained in the tests. Mean values of tendon displacement in the hybrid technique were on the order of approximately half those obtained from tests performed with the button technique.
Both repair techniques showed an increase in displacement throughout the test, with significant differences in the value of displacement at the end of the first 1000 cycles (load between 10 and 50 N) and at the end of the second 1000 cycles (load between 10 and 100 N). However, no significant differences were found for the stiffness value at any number of cycles. It is also observed that the repair of the distal biceps brachii tendon using the hybrid technique has significantly higher yield load and ultimate load than the button technique. No significant differences were found regarding the value of stiffness at failure.
All the specimens, except one from the button technique, passed the cyclic load and were subjected to the final tensile test. The failure modes in the button technique were: 5 tearing of the tendon due to the suture, 2 loosening of the knot (the one that did not exceed the cyclic load is included) and 3 combinations of both reasons. There were no deformations of the button or breakage of the suture.
In the hybrid technique, the failure mode in 8 specimens was caused by rupture of the tendon adjacent to the interferential screw, in one specimen the tendon rupture occurred in the vicinity of the clamp and in the last case the failure was produced by migration of the screw followed by tendon tear.
4 Conclusions
Unrepaired distal biceps tendon rupture causes a 30–50% loss of strength in supination and 30% in flexion. For this reason, surgery is considered the current treatment of first choice in active patients. Recently, much emphasis has been placed on surgical techniques that limit complications and improve tendon-bone fixation strength [3].
In this study, the techniques that are commonly used in the repair of the biceps brachii tendon have been assessed. The ideal technique is the one that guarantees an anatomical reconstruction and sufficient mechanical strength and stiffness for the application of a controlled early mobilization protocol [4].
The repairs carried out were subjected to cyclical tests to simulate the immediate rehabilitation process and to quasi-static tests to simulate failure due to overload. Both the range of loads and the number of cycles used in this study are similar to those used in previous studies [5]. In this study we have focused on three biomechanical parameters to evaluate the clinical success of the reconstruction: the displacement of the tendon in the bone tunnel during cyclic loading, the yield load and the failure mode. Ultimate load and stiffness have also been studied, although we consider them to be of less clinical importance.
The displacement of the tendon in the bone tunnel indicates the laxity with which the repair will remain throughout the rehabilitation. The smaller it is, the better the repair. Actually, it does not consider the effect of biological fixation during the postoperative period, but it clearly indicates the benefits of one repair over another. Data shows that the displacements obtained after the 1000 and subsequent cycles are significantly different between the two techniques, with approximately 50% less displacement when the interferential screw is added.
Although no significant differences have been found regarding stiffness, when both techniques are compared, it is observed that the hybrid technique reaches significantly higher levels of resistance, specifically in terms of the level of yield and ultimate load. The yield load is considered to be the most representative value of the evolution of failure, since if higher tensile loads appear, the damage will be permanent and the displacement will grow very rapidly towards values of laxity that are not admissible in clinical practice.
Regarding the failure mode, in the specimens with the tendon anchored only with the button, the failure mode was tendon tear due to the suture, loosening of the knot, or both. With the hybrid technique, 80% of the failures were due to rupture of the tendon adjacent to the screw. In addition, the only reconstruction that broke before the final tensile test was performed with the button technique. Therefore, it can be inferred that the hybrid technique, limits suture slippage failure and prevents loosening of the knot.
From a clinical point of view, adding the interferential screw to the button system does not significantly increase operating time. Although the use of two implants (button and screw) makes the cost of the procedure more expensive, the good results, the low percentage of complications and the faster return to the activity of daily life, work and/or sports, make it the first therapeutic option in young, active patients with high functional demand.
One limitation of this study is that animal tissues have been used, so the quantitative values resulting from the tests cannot be directly extrapolated to human behavior. However, the results are adequate for the purposes of qualitative comparison between the different techniques.
Finally, the results of this study suggest that, with the hybrid technique, that is, adding the interferential screw, a significantly better repair of the biceps brachii is achieved at its distal insertion. Also, by reducing displacement by approximately half and increasing load capacity, the hybrid technique allows for an early and effective rehabilitation program [12].
References
Mazzocca, A.D., et al.: Biomechanical evaluation of 4 techniques of distal biceps Brachii tendon repair. Am. J. Sports Med. 35(2), 252–258 (2007)
Wörner, E., et al.: Higher failure rate of suture anchors in partial distal biceps tendon ruptures in comparison with Endobutton fixation. JSES Int. 5(4), 821–826 (2021)
Spang, J.T., et al.: A biomechanical comparison of Endobutton versus suture anchor repair of distal tendon injuries. J. Shoulder Elbow Surg. 15(4), 509–514 (2006)
Arianjam, A., et al.: Biomechanical comparison of interference screw and cortical button with screw hybrid technique for distal biceps brachii tendon repair. Orthopedics 36(11), 1371–1377 (2013)
Rutka, V., et al.: Distal biceps tendon repair via new knotless Endobutton fixation: a biomechanical study. Shoulder Elbow 13(3), 321–328 (2021)
Greenberg, J.A., et al.: Endobutton-assisted repair of distal biceps tendon ruptures. J. Shoulder Elbow Surg. 12, 484–490 (2003)
Lemos, S.E., et al.: A new technique: in vitro suture anchor fixation has superior yield strength to bone tunnel fixation for distal biceps tendon repair. Am. J. Sports Med. 32(2), 406–410 (2004)
Idler, C.S., et al.: Distal biceps tendon repair: a biomechanical comparison of intact tendon and 2 repair techniques. Am. J. Sports Med. 34(6), 968–974 (2006)
Kettler, M., et al.: Failure strengths in distal biceps tendon repair. Am. J. Sports Med. 35(9), 1544–1548 (2007)
Krushinski, E.M., et al.: Distal biceps tendon rupture: biomechanical analysis of repair strength of the Bio-Tenodesis screw versus suture anchors. J. Shoulder Elbow. Surg. 16, 218–223 (2007)
Chavan, P.R., et al.: Repair of the ruptured distal biceps tendon: a systematic review. Am. J. Sports Med. 36(8), 1618–1624 (2008)
Bisson, L.J., et al.: Is it safe to perform aggressive rehabilitation after distal biceps tendon repair using the modified 2-incision approach? A biomechanical study. Am. J. Sports Med. 35(12), 2045–2050 (2007)
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Open Access This chapter is licensed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license and indicate if changes were made.
The images or other third party material in this chapter are included in the chapter's Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the chapter's Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder.
Copyright information
© 2023 The Author(s)
About this paper
Cite this paper
Santa-María, A.L., Agharbi, M., Thams, C.B., Martel, O. (2023). Biomechanical Study of the Addition of the Interferential Screw in the Repair of the Distal Biceps Brachii Tendon. In: Vizán Idoipe, A., García Prada, J.C. (eds) Proceedings of the XV Ibero-American Congress of Mechanical Engineering. IACME 2022. Springer, Cham. https://doi.org/10.1007/978-3-031-38563-6_19
Download citation
DOI: https://doi.org/10.1007/978-3-031-38563-6_19
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-031-38562-9
Online ISBN: 978-3-031-38563-6
eBook Packages: EngineeringEngineering (R0)