Abstract
New technologies are emerging under the umbrella of digital transformation in healthcare such as artificial intelligence (AI) and medical analytics to provide insights beyond the abilities of human experts. Because AI is increasingly used to support doctors in decision-making, pattern recognition, and risk assessment, it will most likely transform healthcare services and the way doctors deliver those services. However, little is known about what triggers such transformation and how the European Union (EU) and Norway launch new initiatives to foster the development of such technologies. We present the case of Operating Room of the Future (FOR), a research infrastructure and an integrated university clinic which investigates most modern technologies such as artificial intelligence (AI), machine learning (ML), and deep learning (DL) to support the analysis of medical images. Practitioners can benefit from strategies related to AI development in multiple health fields to best combine medical expertise with AI-enabled computational rationality.
You have full access to this open access chapter, Download chapter PDF
Similar content being viewed by others
Keywords
- Artificial intelligence (AI)
- Machine learning (ML)
- Future of work
- Knowledge management
- Healthcare
- Digitalization
- Operating Room of the Future (FOR)
1 Introduction
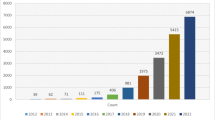
Artificial intelligence (AI) implementation in healthcare organizations as part of digital transformation initiatives is an area with growing interest and accelerating implementation [1, 2]. AI can be leveraged to analyze big volume, variety, and velocity data and in supporting evidence-based decision-making while reducing medical errors and improving care coordination [3]. Because AI can automate various tasks that previously required human judgment such as reasoning, risk assessment, and decision-making, it appears to edge closer and closer to human capabilities generating new human-AI hybrid collaboration that opens completely new questions for work and organizing [4]. Thus, the introduction of AI in organizations is posing significant challenges such as doubting the diagnosis when making professional judgements with AI [2].
Initial studies on AI and the future of work focused on the evolution of professions and the economic impact, expecting that knowledge work would be substituted by intelligent machines [5]. Yet, acknowledging that organizations will thrive by combining the best of both worlds, humans with machines [6], several scholars started to investigate how the nature of work is changing with AI and with what implications for management and organizations [7]. For example, deep machine learning can perform cognitive work by learning from large high-quality data sets to improve the resolution of cardiovascular imaging, to develop pattern recognition, and to make automated predictions of cardiovascular diseases months in advance compared to traditional diagnostics [8].
AI is therefore predicted to affect almost every aspect of the work that medical professionals need to perform. However, little is known about what triggers such transformation and how the European Union (EU) and Norway launch new initiatives to foster the development of such technologies. Moreover, it is unclear how medical work is changing with the introduction of algorithms that process information and provide predictions. Additionally, AI implementation poses many challenges concerning the nature of medical work, professions that predominantly relied on human knowledge and judgement, and ethical concerns, which call for new approaches such as responsible AI. As a result, the repercussions on medical work have emerged as a major issue when considering AI implementation, since health professions tend to utilize a plethora of advanced technologies that shape work content, process, and organizational structures [9]. This prompts the issue that health professionals need to navigate the transition from “human-based” to “human-AI hybrids” collaborations during their work activities.
This chapter presents the Operating Room of the Future (FOR), which is a research infrastructure and an integrated university clinic developed from a multidisciplinary collaboration between St. Olav Hospital in Norway and the Norwegian University of Science and Technology (NTNU) and key initiatives related to AI technology. The main goal of these projects is to support medical professionals to combine their expertise with novel AI technology for improving their work performance. In the next sections, we present important notions about digital transformation in healthcare with a focus on AI technology. Then, we discuss the strategies and policies developed in EU and in Norway as part of digital transformation.
2 Digital Transformation in Healthcare
Digital transformation (DT) had and is continuing to have a profound impact on the way we create our social reality [10]. The word digital is omnipresent in everyday activities, and it is transforming the way organizations operate in the new virtual reality [11, 12]. We refer to digital transformation as “a process that aims to improve an entity by triggering significant changes to its properties through combinations of information, computing, communication, and connectivity technologies” [13]. Recently, DT has shifted its influence from the mere technicalities of creating a virtual tool toward human-electronic devices interaction, which requires specific attention and investigation for being able to exploit its opportunities and to be aware of its challenges [1]. Given the unprecedented amount of digital technologies and pervasive information, organizations need to understand the way such technologies have been developed, the way they are implemented in organizations, and with what consequences for management [14].
Several examples show how digital technologies are transforming multiple industries. For instance, telecommunication focused on the operating system platforms like Android and iOS and on the development of mobile applications to gain value and maintain own position on the marketplace [15, 16]. Another example refers to dynamics within the travel industry that took another path with the advent of peer-to-peer digital platforms such as Airbnb, TripAdvisor, Booking.com, and others, which shifted the power of control from the providers toward the final customers during the pre- and post-acquisition process [11, 17]. Indeed, the customer evaluation acquired not only social but also economic impacts on many companies in several industries, acting as an electronic word of mouth always available online [18]. Therefore, digital platforms are changing the way people interact [19], and new payment platforms are reconfiguring payment methods making them available anytime everywhere. Another example refers to the healthcare industry, which by definition is a knowledge-intensive and information-intensive industry and is making progress by rendering available medical information through electronic health records [20, 21], mobile health applications [22], and more in general with health information exchange platforms (HIE) [20, 23].
The implementation of digital technologies in healthcare gives new opportunities to improve the quality of healthcare services and to decrease the costs through data processing and intelligent sharing of information [10, 20, 24]. Digital technologies are particularly beneficial for improving internal and external processes of healthcare facilities and for managing large amount of medical information [25, 26]. Therefore, the generation, storage, and processing of digital information is the lifeblood of digital transformation. This allows to exploit different advantages of intra- and inter-organizational distribution of limited resources with a patient-centered perspective [27], to facilitate the interactions between multiple healthcare actors, and to optimize internal processes [10, 23].
The digital transformation in healthcare does not involve only few countries, but it has an international or better said global magnitude. For example, the European Union developed a Digital Health and Care Innovation initiative in the context of the Digital Single Market Strategy 2021–2027Footnote 1 to enhance the interoperability of healthcare systems, its quality, and access across European counties. New Zealand Health Strategy 2017–2027Footnote 2 defined the four core components that will guide the strategic digital investments for the next years. Australian digital health strategyFootnote 3 outlined seven strategic priorities to foster a patient-centered system and to provide choice, control, and transparency. The policy at a global level provides financial investments to foster digital transformation in healthcare. Among the global initiatives, electronic healthcare records (EHR) and more in general the development of healthcare platforms played a strategic role [28]. Its main aim is to store digital medical information over time and share it with authorized healthcare actors [29]. They are implemented as vehicles to improve the communication between actors and to increase the coordination at high levels of reliability. Their implementation is valuable also for administrative purposes and patient transactions as they contain personal information of patients and are available across time and space [30]. EHR has the possibility to combine clinical and financial data to contain costs and improve the care quality, which is also supported by political initiatives to support digital transformation of healthcare.
3 Artificial Intelligence Technology as Part of Digital Transformation in Healthcare
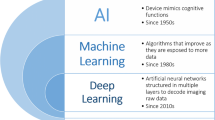
New initiatives are emerging under the umbrella of digital transformation in healthcare such as artificial intelligence (AI) and medical analytics to develop deeper and better insights beyond the abilities of human experts by delivering granular, micro-targeted insights [31]. AI is extensively used for cleaning and analyzing structured and unstructured data from multiple sources. Since data analysts spend most of their time cleaning and organizing data, AI has been extensively used to accelerate this process while saving time and making the process more efficient [32]. AI can autonomously generate insights for taking actions based on information extracted from datasets to reach a set of objectives. We refer to AI as “the ability of a system to identify, interpret, make inferences, and learn from data to achieve predetermined organizational and societal goals” [33].
In line with this definition, artificial intelligence has been increasingly used for analyzing vast amounts of medical information collected through digitized devices from multiple sources across healthcare units to offer IT infrastructure, operational, organizational, managerial, and strategic benefits [34, 35] and to enable the shift toward value-based care over volume [36], whereas the term “medical analytics” refers to descriptive and interpretive analysis of digitized data with advanced statistical, data mining, and machine learning methods for problem-solving and algorithmic (supporting or driving) decision-making [37]. Analytics have the potential to make sense of the information created by individuals defined also as “walking data generators” [38]. They are promising for their ability to collect not only structured but also unstructured data to identify connections and patterns across vast datasets [39], to track and profile fine-grained behaviors of patients [40], and to make algorithm-driven predictions [41].
Previous studies investigated this phenomenon by focusing on its inherent duality. On one side, advanced analytics have been effective in increasing firms’ competitiveness [42], making better predictions and more informed decisions [43]. On the other side, they have been criticized for breach of privacy as they distort the power relationship on personal information [44], exploit individuals for data collection purpose [45], share information with other organizations beyond the purposes of individuals’ given consents [46], and restrict their choices through algorithms for profiling individuals [47]. Despite the promising benefits, the aggregation and use of the information extracted from vast datasets challenges accepted social and ethical norms [40]. Specifically, ethical concerns are stemming from the sensitivity of data and from unlimited and unknown opportunities that may arise from identified patterns and connections across vast datasets, which might limit or totally obscure these promised benefits [48].
Ethical concerns became even more pervasive because social processes, business transactions, and governmental decisions are increasingly delegated to advanced analytics such as algorithms, machine learning, deep learning, and big data analytics [49]. The promise of making sense of the information collected in big datasets is also coupled with discrimination against disadvantaged groups, uncertainty over how and why algorithm-driven decisions has been achieved (explainability), which rules have been applied, and to which specific information in the datasets as analytics has the capacity of tweaking operational parameters and rules. Therefore, more challenges and ethical concerns arose with the analytics’ complexity and their interaction with others’ results [49]. Authors developed a map for a rigorous diagnosis of ethical concerns emerged with algorithms. They discussed three epistemic types of ethical concerns that refer to the quality of the evidence provided by the algorithms and two normative kinds of ethical concerns, which refer to the “fairness” of the actions taken based on algorithms results and its effects. This framework was used to conduct a synthesis of prior literature and provide a research agenda for future studies to develop responsible AI for digital health [50].
Moreover, AI technology often provides results that are significantly different from those elaborated by experts, the so-called AI opacity problem [51]. In these circumstances, when experts try to compare the reasoning behind their results with the logic and the procedures followed by algorithms, it is difficult or almost impossible not only for the experts but also for the developers of algorithms due to the black box issue. A recent study highlighted the issue of training and evaluating algorithms only on know-what aspects of knowledge, while experts use rich know-how practices in their daily work [9]. Although more information is captured digitally that can contribute to make more informed and evidence-based decisions, at the same time, algorithms can actually reduce the transparency of the outcomes as they provide black box outputs. On the one hand, AI comes with the promise of more objectivity and fairness by mitigating human biases. On the other hand, AI raises significant ethical challenges related to the quality of the evidence provided that might be inconclusive, inscruble, or misguided, leadning to unfair outcomes and unexpected transformative effects [50]. For example, the introduction of hiring algorithms in organizations shapes the notion of fairness in different ways by confirming and contesting it in different phases of implementation [4].
Medical analytics are characterized by unique features such as the capability to aggregate, process, and analyze huge volumes of medical information for transforming it into actionable information [52]. To materialize this feature in the healthcare context, an in-depth understanding of the information lifecycle management (ILM) is necessary. Among the several definitions of analytics capability, our study embraces the perspective offered by Wang and Hajli [52], which defined it as “the ability to acquire, store, process and analyse large amounts of health data in various forms, and deliver meaningful information to users, which allows them to discover business values and insights in a timely fashion” (p. 290). Consequently, analytics are increasingly used in the process of knowledge creation by collecting, elaborating, and displaying valuable information for decision-making [51]. There are several categories of medical analytics [35, 52] in healthcare (Table 1).
Descriptive capability refers to summarization of historical data in digital formats, where a high-speed parallel processing helps better understand what happened in the past. Although the capability used to quickly synthesize vast amounts of health data to compare medical interventions across settings of care enables care actors to improve the quality of care services by providing patient-centered care, few studies discussed descriptive analytics [55]. A recent review highlighted the importance to collect and analyze data with analytical methods to describe specific situations of specific patients, to understand what happened to them through the categorization of knowledge from vast datasets [34]. The techniques of profiling and classifying individuals into groups based on any given characteristic to support realistic public health interventions are widely used techniques to make actionable and interpretable recommendations [54]. Based on the categorization of this information, small patterns or correlations are calculated, which created clusters of groups according to their behavior, preferences, and other characteristics [53, 56].
Predictive capability relies on a set of sophisticated statistical tools to develop models and estimations to forecast the future for a specific variable, which helps understand what will happen in the future. The use of advanced analytics to predict future patterns of care behavior was the most popular capability in healthcare because predictions in healthcare seem to be considered more valuable than explanation since algorithms results are measured in lives [34, 39, 65, 66]. For example, an algorithm can calculate patients’ individual therapeutic goals and preferences, hospital staffing (including staff members’ experience and performance), resource constraints, and external conditions such as whether other hospitals are diverting patients in the emergency department in the case of a disaster [53]. Algorithms that make predictions and suggest decisions based on probabilities were considered an ideal application because AI-controlled algorithm predicts the admission trajectory significantly better than medical officers, who have an average error rate of about 30% [41]. They were intensively used also to make treatment recommendations to improve overall health outcomes in a population. However, these recommendations may conflict with physicians’ ethical obligations to act in the best interests of individual patients [53].
Prescriptive capability enables users to automatically improve prediction accuracy by taking in new datasets to develop more thorough decisions regarding the diagnoses and treatments. Next, Wang et al. [35] identified additional categories, which are more advanced and sophisticated. Analytical capability processes massive healthcare records (structured data collected inside the healthcare units) to identify patterns of care and discover associations. It allows healthcare organizations to parallel process large data volumes, manipulate real-time or near-real-time data, and capture all patients’ visual data or medical records. Unstructured data analytical capability processes massive healthcare data (unstructured and semi-structured data gathered across multiple healthcare units, so do not fit into predefined data models) to identify unnoticed patterns of care.
Decision-making capability shares information and knowledge such as historical reporting, executive summaries, drilldown queries, statistical analyses, and time series comparisons. It provides a comprehensive view for evidence-based medicine, for detecting advanced warnings for disease surveillance, and for developing personalized patient care. Artificial intelligence systems were commonly used to gather structured and unstructured data to automatically assist medical decision-making based on the recommendations done through pattern recognition [3, 32, 53, 59]. One of the main benefits referred to the possibility to compare data from multiple sources and to identify potential solutions visible in the forms of trees. AI was intensively used to create deeper knowledge and to identify the logics underlying AI predictive modelling [54]. New insights extracted from health-related data were extremely helpful to detect a disease and to decide the treatment(s) to follow [67]. Therefore, the decision-making process was partially delegated to advanced analytics. This delegation has been translated also in the design of algorithms by inscribing developers vision of who will be responsible for mistakes through the degree of social embeddedness and reflection permitted in use [68]. The decision-making capability is coupled with “reporting capability,” for organizing the collected data in easily understandable ways, such as describing the information contained in the datasets for specific purposes [34].
Surveillance capability offers the opportunity to survey and monitor past actions based on the information collected indirectly such as the time, the care actor who did that action, the notes taken in databases, and the information consulted based on specific accounts and other. For example, patients now have the possibility to own health information anytime and take decisions in everyday life concerning healthcare, disease prevention, and health promotion [69]. Although they do not possess the expertise for the physician to interpret the information received from the previous medical visits and cannot make an auto-diagnosis, the patient is empowered to the information collected, which requires a higher patient involvement and also some digital and health literacy. Patients are not considered passive receivers of the healthcare services anymore. This aspect was already inscribed in the design of analytics for more transparency for being able to perform those actions [58, 67] as recognized also by policy-makers [64]. From this indirect data, it was possible also to understand the assumption of the actions done, which might help the traceability.
The capability to correct mistakes offers the opportunity to adjust the erroneous results of algorithms that contributed to a larger decision [68]. The results of advanced analytics were prone to errors as will be discussed in the next section. Therefore, such capability will be extremely beneficial for correcting the results provided by algorithms. It will increase the awareness of potential errors created by AI systems, which will be trained to detect such errors to correct them or to take them into account when making the decision. Therefore, designers will need to develop the ability to question the results provided by AI tools, and this can be achieved by analyzing the process AI followed and by extracting meaningful information for future reflections. Lastly, traceability tracks output data from the system’s IT components throughout the organization’s service units. Examples of healthcare-related data are cost data, clinical data, pharmaceutical R&D data, patient behavior and sentiment data from payers, healthcare services, pharmaceutical companies, consumers, and stakeholders outside healthcare.
Artificial intelligence and medical analytics have the potential to generate multiple benefits, but at the same time, they are coupled with significant ethical challenges [50, 70] as the “walking data generators” (individuals) are often unaware of how their data are used, for which purposes, and by whom [37]. Therefore, the increasing use of big data containing personal, sensitive information and the growing reliance on algorithms to make sense of this data and identify behavioral patterns raise concerns of fairness, responsibility, and human rights [70]. Scholars shifted their attention from technological means toward the content (information) created by these technologies, which is composed of different moral dimensions. Information is increasingly used as evidence to make decisions and choices, whose outcomes are calling for ethical approaches to address the information creation, sharing, storage, use, and protection. However, ethics concerns first the collections, aggregation, use, and analysis of large datasets and then the information, thus creating a semantic shift [40].
4 Digital Healthcare Transformation in Europe and in Norway
To appreciate the digital transformation in healthcare, it is helpful to understand broader initiatives developed by the European Union (EU) and Norway that are engaged with policies and actions to provide top-quality digital services. The final aim is to empower citizens to build a healthier society and to offer citizen-centered health services. The maximum aspiration is to help citizens take care of their health and prevent future disease. Indeed, one of the most desirable solutions to decrease care costs is to prevent any kind of disease. This means to educate citizens to develop healthy lifestyles and to avoid bad behaviors in the present, which might lead to potential disease in the future. If the aim of empowering citizens towards the prevention will not achieve the desired outcomes, citizen will receive innovative health services to respond to their health demand following a citizen-centered approach.
The European Union focuses on three priorities.Footnote 4 The first one is to provide citizen secure access to personal health data across EU borders; the second refers to the implementation of personalized medicine through shared European data infrastructure, while the third one focuses on increasing citizen empowerment to encourage people to take care of their health and to stimulate interactions between patients and care providers. The aim is to become more resilient, accessible, and effective in providing quality care for European citizens.Footnote 5 The implementation of new technologies aims at fostering organizational changes in different departments and for alternative work activities. Digital tools are co-created, co-distributed, and co-used involving directly the end users and consciously fostering a highly collaborative environment. Indeed, the contribution of patients and of other active actors represents the keystone for an interactive digital healthcare ecosystem. A continuous state of evolution and a steady contribution from end users create unexpected changes, which may enable new patterns of communication and interaction.
Digital transformation of healthcare can foster the transition toward new care models focused on patients’ need. Patients’ contribution represents a keystone for creating useful and usable services for everyday activities and at the same time ends up with enriching the construction of a new healthcare digital ecosystem. The innovativeness lies in the integration of different needs of all involved categories in an open space for dialogue, listening, co-creating, and negotiating toward proposals for common innovative solutions [30]. The aim is to offer tailored digital health services and to give access to dematerialized medical information, to manage personal medical information, to monitor the process of personal continuous healthcare, to be aware of the healthcare process, to understand how healthcare system works (transparency), and to be responsible for the personal medical data management (patient empowerment and awareness).
Patient-centered care system can be seen as a partnership among caregivers and care receivers to diagnose and prescribe a suitable treatment. Six aspects are fundamental to define this concept, which are shared decision-making, psychosocial support, access to information, access to care, coordination of care, and self-management [71]. With the use of new digital technologies, a new healthcare paradigm emerges, which transforms the delivery of healthcare services to bring them closer to the patient guided by the following strategies. (1) Efficiency aims at reducing healthcare costs by avoiding unnecessary diagnostic interventions and increasing communication between healthcare institutions and the patient. At the same time, it is committed to ensuring the quality of health services through comparisons between different suppliers to enhance the delivered quality (2). Encourage the empowerment of patients (3) by making personal data, medical records, diagnosis, and treatment accessible through digital platforms and by making more responsible the care information process. Increasing the quality of the doctor-patient relationship to facilitate shared decision-making is a direct consequence of patient empowerment [27]. The digital transformation of healthcare sector increases the probability to maintain and further improve these strategies. The healthcare quality is not only a medical concern, but it is also about the process to reach outstanding care results, which is one of the high priorities of the Norwegian healthcare system.
Norway is one of the most innovative and technological countries, and it is constantly engaged with transforming health and welfare system with new tools, services, or technologies. Key initiatives refer to the development of electronic health record (EHR), ePrescriptions, and algorithms. Ellingsen and Monteiro [72] provided a chronological perspective of the EHR as follows. In the mid-1980s, a group of laboratory technicians in a central hospital highlighted the need of creating a system to support internal work processes by sharing files necessary to perform daily tasks. For the next 10 years, this group and other hospitals continued to develop a network of computers and other important features such as writing clinical documents of each patient and sharing it with the network. In 1997, a limited company was established to follow the implementation of the new system in smaller hospitals. The number of users and hospitals that adhered to this initiative increased, more employees have been hired, and new challenges mined the internal coordination. In 2002, the Norwegian health system established regional health authorities, which were in charge of managing the acquisition of new systems in hospitals with public bids for tenders. This triggered new needs for different types of users at the regional level, which were difficult to meet. Such changes led to redesign the process of EHR software and to redefine the content in the EHR in a dynamic way. A project management approach was used to work on new activities, which was increasingly used in the next years.
The process of transforming the healthcare system continued during 2000 with the eNorway plan,Footnote 6 which enabled patients to communicate with their doctors and the hospital through digital platforms such as electronic healthcare record (EHR). This gave the citizens freedom to choose the family doctor online, to receive online medical results from the hospital, and to have access to own medical data with referrals and medical records at any time. The eNorway plan offered telemedicine solutions by implementing broadband in hospitals and primary health services. It was an essential service during the COVID-19 pandemic. Healthcare public system provided telehealth consultations since the 1990s; thus, it could rely on prior experience to further improve this technology to share high-quality medical images to help make diagnoses.
From 2022, Norway plan to implement a new unified EHR, called EPIC, the regional Health Platform program [73]. The new system was acquired with a bid-and-tender process in order to unify the disparate patient records systems used currently in healthcare organizations. The aim is to reduce information fragmentation and facilitate cross-sectoral coordination. EPIC will be implemented first in Trondheim municipality and then in other municipalities in Central Norway. It is important to note that GPs offices are private business, and they have the possibility of deciding whether to implement it or not.
ePrescriptions are another key initiative of the digital transformation in healthcare sector in Norway, which started to be widely adopted from 2011 [74]. The digital prescriptions aim to support general physicians with the activity of prescribing patients medicines or medical visits with hospitals or other healthcare organizations. The first drafts of the prescriptions were developed since the 1990s; however, the results were discouraging. Only in 2011, a large-scale deployment achieved positive outcomes. Until 2013, ePrescriptions have been implemented in General Physicians’ (GPs) offices and pharmacies in all municipalities.Footnote 7
Norwegian healthcare system has been a model for other countries around the world, and it is developing new healthcare models based on digital data and advanced technologies in order to move toward a more preventative approach presented in The Nordic Health 2030.Footnote 8 In line with this, Norway developed a national strategy for artificial intelligence in order to create a good basis for AI for enhancing innovation capacity in multiple sectors such as healthcare.Footnote 9 Another way to trigger digital healthcare transformation in Norway is by constructing operating rooms that use most advanced technologies to support medical work in critical times. In the next section, we present the case of Operating Room of the Future (FOR) in Trondheim, Norway.
5 What Is the Operating Room of the Future?
The Operating Room of the Future (FOR) is a research infrastructure and an integrated university clinic developed from a multidisciplinary collaboration between St. Olav Hospital in Norway,Footnote 10 the Norwegian University of Science and Technology (NTNU),Footnote 11 and the not-for-profit and independent research institute SINTEF.Footnote 12 The three entities developed the basis for the infrastructure in terms of funding proposals, scientific content, logistics, and others between 2003 and 2005. From 2006 to 2012, two operating rooms have been developed for laparoscopic surgery and vascular diseases close to the existing operating department. An interactive lecture room was equipped with HD transmission to watch the operative procedures and to communicate directly through dedicated audio and video channels. From 2013 to present, new operating rooms have been developed within surgical disciplines such as neurosurgery, gastrointestinal, ear-nose-and-throat diseases (ENT), orthopedic, and genecology (Fig. 1). FOR is now a department under the director of research and development at St. Olav’s hospital and Department of Circulation and Medical Imaging, Faculty of Medicine, NTNU.
Various stakeholders such as clinicians, PhD candidates, technologists, scientists, and industry conduct cutting-edge research in these six operating rooms. They are unique “laboratories” for developing, testing, and implementing new technologies and new treatment modalities with a focus on minimal invasive image-guided patient treatment and medical technology [75]. This arena for research and development investigates most modern medical equipment such as artificial intelligence (AI), machine learning (ML), deep learning (DL), neural networks, and integration of advanced visualization tools, robotic arms, and others. The six FOR operating rooms have become an important clinical research platform for minimally invasive therapy and for the development of medical technology. The overarching aim is to improve patient care, to develop more efficient logistics and a better architecture of operating departments. The Research Council of Norway financially supported the development of FOR; it is part of the national research infrastructure NorMIT (Norwegian centre for Minimally invasive Image guided Therapy and medical technologies)Footnote 13 and cooperates with the Intervention Centre at the National Hospital, Oslo.
There is an increasing number of research projects conducted in the Operating Room of the Future (FOR) in several fields. Decision support in lung cancer diagnosticsFootnote 14 is an ongoing project that integrates and implements new tools for image analysis and decision support in patient care for lung cancer. A multidisciplinary team (MDT) is developing a digital technology to support patient assessment and treatment [76]. Artificial intelligence (machine learning) is used to analyze patient’s CT and PET-CT for finding normal anatomy and pathology (tumor). It is especially used for automatic detection and segmentation of mediastinal anatomical structures and potentially malignant lymph nodes for accurate lung cancer diagnosis.
In line with cancer diagnostic, FOR recently developed the project entitled IDEAR: Improving Cancer Diagnostics in Flexible Endoscopy Using Artificial Intelligence and Medical Robotics in collaboration with Craiova University, Romania.Footnote 15 This project is developing an advanced prototype of a medical software and robotic platform for improving cancer diagnostics in flexible endoscopy using AI and medical robotics. The researchers are creating a platform to allow concomitant visualization of the anatomical target(s), the neighboring anatomy, and the CT/MRI image. The project allows performing both diagnostic and treatment during the same procedure using an advanced smart robotic system and customized instruments with dual electromagnetic-optical tracking.
Deep convolutional neural networks (CNNs) are increasingly used for digital analysis of histopathological images. A research team is developing and implementing an open-source platform for deep learning-based research and decision support in digital pathology [77]. FastPathology is a new platform using the FAST framework and C++ to minimize memory usage for reading and process whole-slide microscopy images (WSIs). This offers an efficient visualization and processing of WSIs in a single application, including inference of CNNs with real-time display of the results.
6 Conclusions
This chapter presents key initiatives of digital transformation in the healthcare sector in the age of artificial intelligence, where the line between virtual and physical reality is pretty thin. We started with a general overview of digital transformation in healthcare. Then, we discussed the emergence of new technologies such as artificial intelligence (AI) and medical analytics as part of digital transformation. In this section, we highlighted the main capabilities that differentiate these technologies from the previous ones and how they contribute to “triggering significant changes to the properties of entities through combinations of information, computing, communication, and connectivity technologies” [13]. After presenting two specific examples of digital health transformation in Europe and in Norway, we conclude with Operating Room for the Future (FOR), an outstanding research infrastructure and an integrated university clinic, which is developing AI technology to support medical tasks in specific health fields such as pulmonology, digital pathology, cardiology, and others.
Due to digital pervasiveness of new technologies, it is pivotal to understand the mechanisms of organizational processes, multi-sided platforms, healthcare applications, and social networks as they have the potentiality to lead toward an effective design, management, and implementation of digital health information systems. Moreover, we believe that the materialization of this opportunity depends on the engagement of the actors involved in this process. It is important to investigate topics at the intersection of work, technology, and information systems and for a broader academic audience such as medicine, computer science, and sociology of work. Such a focus will contribute to the understanding of the development of AI technology in the workplace and to the literature on knowledge creation [14, 78, 79]. Next, there is the need to investigate the challenges doctors are facing with the introduction of AI such as disputing what is worth knowing, what actions matter to acquire new knowledge, and who has the authority to make decisions. This will provide new insights into how and why AI is reconfiguring work boundaries of healthcare professionals and with important consequences for their jurisdictions, skills, status, and visibility. Lastly, it is important to highlight the ways AI tools are used in medical work by paying equal attention to the actions performed by doctors and their social interactions as well as to the machines that are part of the medical workplace [11, 80].
The digital transformation of the healthcare sector is driven by multiple mechanisms, such as the transformation of the population demand for health services, the changes in the relationship between patients and care providers, the pervasive use of digital technologies, and the emergence of new technologies that significantly differ compared to the previous ones. The digitalization of the care paths, increased interoperability among actors, organizational communication, tools, and organizations offer new models for knowledge management, which can be beneficial for individual performance and organizational efficiency, but it also raises several concerns related to privacy, security, and responsibility. A dynamic and digital environment of an ecosystem composed of often-conflicting interests requires a better understanding of the logic and opportunities of a plethora of virtual tools to match them with everyday requirements. The activity of matching the digital solutions with specific and context-dependent needs composes the puzzle of managing the Health Information Systems in current times. The main objectives refer to increasing the quality of service delivery, empowering the citizen-patient that fosters a patient-centered ecosystem.
Notes
- 1.
- 2.
- 3.
- 4.
- 5.
- 6.
- 7.
- 8.
- 9.
- 10.
- 11.
- 12.
- 13.
- 14.
- 15.
References
Baptista, J., Stein, M.-K., Klein, S., Watson-Manheim, M. B., & Lee, J. (2020). Digital work and organisational transformation: Emergent Digital/Human work configurations in modern organisations. Journal of Strategic Information Systems, 101618. https://doi.org/10.1016/j.jsis.2020.101618
Lebovitz, S., Levina, N., & Lifshitz-Assaf, H. (2021). Is AI ground truth really “true”? The dangers of training and evaluating AI tools based on experts’ know-what. Management Information Systems Quarterly.
Bjerring, J. C., & Busch, J. (2020). Artificial intelligence and patient-centered decision-making. Philosophy & Technology. https://doi.org/10.1007/s13347-019-00391-6
van den Broek, E., Sergeeva, A., & Huysman, M. (2021). When the machine meets the expert: An ethnography of developing AI for hiring. MIS Quarterly.
Frey, C. B., & Osborne, M. A. (2017). The future of employment: How susceptible are jobs to computerisation? Technological Forecasting and Social Change, 114, 254–280. https://doi.org/10.1016/j.techfore.2016.08.019
McAfee, A., & Brynjolfsson, E. (2017). Machine, platform, crowd: Harnessing our digital future. WW Norton.
Raisch, S., & Krakowski, S. (2020). Artificial intelligence and management: The automation-augmentation paradox. Academy of Management Review.
Choi, E., Schuetz, A., Stewart, W. F., & Sun, J. (2017). Using recurrent neural network models for early detection of heart failure onset. Journal of the American Medical Informatics Association, 24(2), 361–370.
Lebovitz, S., Lifshitz-Assaf, H., & Levina, N. (2022). To engage or not to engage with AI for critical judgments: How professionals deal with opacity when using AI for medical diagnosis. Organization Science.
Karahanna, E., Chen, A., Liu, Q. B., & Serrano, C. (2019). Capitalizing on health information technology to enable digital advantage in US hospitals. MIS Quarterly, 43(1), 113–140. https://doi.org/10.25300/misq/2019/12743
Orlikowski, W. J., & Scott, S. V. (2015). The algorithm and the crowd: Considering the materiality of service innovation. MIS Quarterly, 39(1), 201–216. https://doi.org/10.25300/MISQ/2015/39.1.09
Orlikowski, W. J., & Scott, S. V. (2021). Liminal innovation in practice: Understanding the reconfiguration of digital work in crisis. Information and Organization, 31(1), 100336. https://doi.org/10.1016/j.infoandorg.2021.100336
Vial, G. (2019). Understanding digital transformation: A review and a research agenda. The Journal of Strategic Information Systems, 28(2), 118–144. https://doi.org/10.1016/j.jsis.2019.01.003
Benbya, H., Pachidi, S., & Jarvenpaa, S. L. (2021). Special Issue Editorial: Artificial intelligence in organizations: Implications for information systems research. Journal of the Association for Information Systems, 22(2), 281–303.
Spagnoletti, P., Resca, A., & Lee, G. (2015). A design theory for digital platforms supporting online communities: A multiple case study. Journal of Information Technology, 30(4), 364–380.
Ye, H. (Jonathan), Kankanhalli, A., & National University of Singapore. (2018). User service innovation on mobile phone platforms: Investigating impacts of lead userness, toolkit support, and design autonomy. MIS Quarterly, 42(1), 165–187. https://doi.org/10.25300/MISQ/2018/12361
Ciborra, C., Braa, K., Cordella, A., Dahlbom, B., Hepsø, V., Failla, A., Hanseth, O., Ljungberg, J., & Monteiro, E. (2000). From control to drift: The dynamics of corporate information infrastructures. Oxford University Press on Demand.
Orlikowski, W. J., & Scott, S. V. (2014). What happens when evaluation goes online? Exploring apparatuses of valuation in the travel sector. Organization Science, 25(3), 868–891. https://doi.org/10.1287/orsc.2013.0877
Sæbø, Ø., Federici, T., & Braccini, A. M. (2020). Combining social media affordances for organising collective action. Information Systems Journal, 30(4), 699–732. https://doi.org/10.1111/isj.12280
Adjerid, I., Adler-Milstein, J., & Angst, C. (2018). Reducing Medicare spending through electronic health information exchange: The role of incentives and exchange maturity. Information Systems Research, 29(2), 341–361. https://doi.org/10.1287/isre.2017.0745
Volkoff, O., & Strong, D. M. (2013). Critical realism and affordances: Theorizing IT-associated organizational change processes. MIS Quarterly, 37(3), 819–834. https://doi.org/10.25300/MISQ/2013/37.3.07
Fox, G., & Connolly, R. (2018). Mobile health technology adoption across generations: Narrowing the digital divide. Information Systems Journal, 28(6), 995–1019. https://doi.org/10.1111/isj.12179
Chen, L., Baird, A., Georgia State University, USA, Straub, D., & Temple University, USA. (2019). An analysis of the evolving intellectual structure of health information systems research in the information systems discipline. Journal of the Association for Information Systems, 1023–1074. https://doi.org/10.17705/1jais.00561
Hansen, S., & Baroody, A. J. (2020). Electronic health records and the logics of care: Complementarity and conflict in the US healthcare system. Information Systems Research, 31(1), 57–75. https://doi.org/10.1287/isre.2019.0875
Makowski, P. T., & Kajikawa, Y. (2021). Automation-driven innovation management? Toward Innovation-Automation-Strategy cycle. Technological Forecasting and Social Change, 168, 120723. https://doi.org/10.1016/j.techfore.2021.120723
Tschang, F. T., & Mezquita, E. A. (2020). Artificial intelligence as augmenting automation: Implications for employment. Academy of Management Perspectives, amp.2019.0062. doi:https://doi.org/10.5465/amp.2019.0062
Yaraghi, N., Gopal, R. D., & Ramesh, R. (2019). Doctors’ orders or patients’ preferences? Examining the role of physicians in patients’ privacy decisions on health information exchange platforms. Journal of the Association for Information Systems, 20(7), 14. https://doi.org/10.17705/1jais.00557
Esmaeilzadeh, P. (2019). The process of building patient trust in health information exchange (HIE): The impacts of perceived benefits, perceived transparency of privacy policy, and familiarity. Communications of the Association for Information Systems, 364–396. https://doi.org/10.17705/1CAIS.04521
Kohli, R., & Tan, S. S.-L. (2016). Electronic health records: How can IS researchers contribute to transforming healthcare? MIS Quarterly, 40(3), 553–573. https://doi.org/10.25300/MISQ/2016/40.3.02
Anderson, C. L., & Agarwal, R. (2011). The Digitization of healthcare: Boundary risks, emotion, and consumer willingness to disclose personal health information. Information Systems Research, 22(3), 469–490.
Fan, W., Liu, J., Zhu, S., & Pardalos, P. M. (2018). Investigating the impacting factors for the healthcare professionals to adopt artificial intelligence-based medical diagnosis support system (AIMDSS). Annals of Operations Research, 1–26.
Morley, J., Machado, C., Burr, C., Cowls, J., Taddeo, M., & Floridi, L. (2019, November 13). The debate on the ethics of AI in health care: A reconstruction and critical review. SSRN Electronic Journal. https://doi.org/10.2139/ssrn.3486518
Mikalef, P., & Gupta, M. (2021). Artificial intelligence capability: Conceptualization, measurement calibration, and empirical study on its impact on organizational creativity and firm performance. Information & Management, 58(3), 103434. https://doi.org/10.1016/j.im.2021.103434
Galetsi, P., & Katsaliaki, K. (2020). A review of the literature on big data analytics in healthcare. Journal of the Operational Research Society, 71(10), 1511–1529. https://doi.org/10.1080/01605682.2019.1630328
Wang, Y., Kung, L., & Byrd, T. A. (2018). Big data analytics: Understanding its capabilities and potential benefits for healthcare organizations. Technological Forecasting and Social Change, 126, 3–13. https://doi.org/10.1016/j.techfore.2015.12.019
Agarwal, R., Dugas, M., Gao, G. G., & Kannan, P. K. (2020). Emerging technologies and analytics for a new era of value-centered marketing in healthcare. Journal of the Academy of Marketing Science, 48(1), 9–23. https://doi.org/10.1007/s11747-019-00692-4
Newell, S., & Marabelli, M. (2015). Strategic opportunities (and challenges) of algorithmic decision-making: A call for action on the long-term societal effects of ‘datification’. The Journal of Strategic Information Systems, 24(1), 3–14. https://doi.org/10.1016/j.jsis.2015.02.001
McAfee, A., & Brynjolfsson, E. (2012). Big data: The management revolution. Harvard Business Review, 90(10), 9.
Floridi, L., Cowls, J., King, T. C., & Taddeo, M. (2020). How to design AI for social good: Seven essential factors. Science and Engineering Ethics, 26(3), 1771–1796. https://doi.org/10.1007/s11948-020-00213-5
Mittelstadt, B. D., & Floridi, L. (2016). The ethics of big data: Current and foreseeable issues in biomedical contexts. Science and Engineering Ethics, 22(2), 303–341. https://doi.org/10.1007/s11948-015-9652-2
Henriksen, A., & Bechmann, A. (2020). Building truths in AI: Making predictive algorithms doable in healthcare. Information, Communication & Society, 23(6), 802–816. https://doi.org/10.1080/1369118X.2020.1751866
Mikalef, P., Krogstie, J., Pappas, I. O., & Pavlou, P. (2020). Exploring the relationship between big data analytics capability and competitive performance: The mediating roles of dynamic and operational capabilities. Information & Management, 57(2), 103169.
Meyer, G., Adomavicius, G., Johnson, P. E., Elidrisi, M., Rush, W. A., Sperl-Hillen, J. M., & O’Connor, P. J. (2014). A machine learning approach to improving dynamic decision making. Information Systems Research, 25(2), 239–263.
Zuboff, S. (2015). Big other: Surveillance capitalism and the prospects of an information civilization. Journal of Information Technology, 30(1), 75–89.
Clarke, R. (2016). Big data, big risks. Information Systems Journal, 26(1), 77–90. https://doi.org/10.1111/isj.12088
Martin, K. E. (2015). Ethical issues in the big data industry. MIS Quarterly Executive, 14, 2.
Loebbecke, C., & Picot, A. (2015). Reflections on societal and business model transformation arising from digitization and big data analytics: A research agenda. The Journal of Strategic Information Systems, 24(3), 149–157.
Floridi, L., Luetge, C., Pagallo, U., Schafer, B., Valcke, P., Vayena, E., Addison, J., Hughes, N., Lea, N., Sage, C., Vannieuwenhuyse, B., & Kalra, D. (2019). Key ethical challenges in the European medical information framework. Minds and Machines, 29(3), 355–371. https://doi.org/10.1007/s11023-018-9467-4
Mittelstadt, B. D., Allo, P., Taddeo, M., Wachter, S., & Floridi, L. (2016). The ethics of algorithms: Mapping the debate. Big Data & Society, 3(2), 2053951716679679. https://doi.org/10.1177/2053951716679679
Trocin, C., Mikalef, P., Papamitsiou, Z., & Conboy, K. (2021). Responsible AI for digital health: A synthesis and a research agenda. Information Systems Frontiers. https://doi.org/10.1007/s10796-021-10146-4
Anthony, C. (2021). When knowledge work and analytical technologies collide: The practices and consequences of black boxing algorithmic technologies. Administrative Science Quarterly, 00018392211016755. https://doi.org/10.1177/00018392211016755
Wang, Y., & Hajli, N. (2017). Exploring the path to big data analytics success in healthcare. Journal of Business Research, 70, 287–299. https://doi.org/10.1016/j.jbusres.2016.08.002
Cohen, I. G., Amarasingham, R., Shah, A., Xie, B., & Lo, B. (2014). The legal and ethical concerns that arise from using complex predictive analytics in health care. Health Affairs, 33(7), 1139–1147. https://doi.org/10.1377/hlthaff.2014.0048
Garattini, C., Raffle, J., Aisyah, D. N., Sartain, F., & Kozlakidis, Z. (2019). Big data analytics, infectious diseases and associated ethical impacts. Philosophy & Technology, 32(1), 69–85. https://doi.org/10.1007/s13347-017-0278-y
Gray, E. A., & Thorpe, J. H. (2015). Comparative effectiveness research and big data: Balancing potential with legal and ethical considerations. Journal of Comparative Effectiveness Research, 4(1), 61–74. https://doi.org/10.2217/cer.14.51
Maher, N. A., Senders, J. T., Hulsbergen, A. F. C., Lamba, N., Parker, M., Onnela, J.-P., Bredenoord, A. L., Smith, T. R., & Broekman, M. L. D. (2019). Passive data collection and use in healthcare: A systematic review of ethical issues. International Journal of Medical Informatics, 129, 242–247. https://doi.org/10.1016/j.ijmedinf.2019.06.015
Mittelstadt, B. D., Stahl, B. C., & Fairweather, N. B. (2015). How to shape a better future? Epistemic difficulties for ethical assessment and anticipatory governance of emerging technologies. Ethical Theory and Moral Practice, 18(5), 1027–1047. https://doi.org/10.1007/s10677-015-9582-8
Morley, J., Machado, C. C. V., Burr, C., Cowls, J., Joshi, I., Taddeo, M., & Floridi, L. (2020). The ethics of AI in health care: A mapping review. Social Science & Medicine, 260, 113172. https://doi.org/10.1016/j.socscimed.2020.113172
Mittelstadt, B. (2017). Ethics of the health-related internet of things: A narrative review. Ethics and Information Technology, 19(3), 157–175. https://doi.org/10.1007/s10676-017-9426-4
Varlamov, O. O., Chuvikov, D. A., Adamova, L. E., Petrov, M. A., Zabolotskaya, I. K., & Zhilina, T. N. (2019). Logical, philosophical and ethical aspects of AI in medicine. International Journal of Machine Learning and Computing, 9(6), 868–873. https://doi.org/10.18178/ijmlc.2019.9.6.885
Astromskė, K., Peičius, E., & Astromskis, P. (2020). Ethical and legal challenges of informed consent applying artificial intelligence in medical diagnostic consultations. AI & SOCIETY. https://doi.org/10.1007/s00146-020-01008-9
Kaplan, B. (2016). How should health data be used?: Privacy, secondary use, and big data sales. Cambridge Quarterly of Healthcare Ethics, 25(2), 312–329. https://doi.org/10.1017/S0963180115000614
Martin, K. (2019). Ethical implications and accountability of algorithms. Journal of Business Ethics, 160(4), 835–850. https://doi.org/10.1007/s10551-018-3921-3
Woolley, J. P. (2019). Trust and justice in big data analytics: Bringing the philosophical literature on trust to bear on the ethics of consent. Philosophy & Technology, 32(1), 111–134. https://doi.org/10.1007/s13347-017-0288-9
Burr, C., Taddeo, M., & Floridi, L. (2020). The ethics of digital well-being: A thematic review. Science and Engineering Ethics, 26(4), 2313–2343. https://doi.org/10.1007/s11948-020-00175-8
Cath, C., Wachter, S., Mittelstadt, B., Taddeo, M., & Floridi, L. (2017). Artificial Intelligence and the ‘Good Society’: The US, EU, and UK approach. Science and Engineering Ethics. https://doi.org/10.1007/s11948-017-9901-7
Lankshear, G., & Mason, D. (2001). Technology and ethical dilemmas in a medical setting: Privacy, professional autonomy, life and death. Ethics and Information Technology, 3(3), 223–233. https://doi.org/10.1023/A:1012248219018
Martin, K. (2019). Designing ethical algorithms. MIS Quarterly Executive, 129–142. doi:https://doi.org/10.17705/2msqe.00012
Schmietow, B., & Marckmann, G. (2019). Mobile health ethics and the expanding role of autonomy. Medicine, Health Care and Philosophy, 22(4), 623–630. https://doi.org/10.1007/s11019-019-09900-y
Floridi, L., & Taddeo, M. (2016). What is data ethics? Philosophical Transactions of the Royal Society A: Mathematical, Physical and Engineering Sciences, 374(2083), 20160360. https://doi.org/10.1098/rsta.2016.0360
Zhou, Y., Kankanhalli, A., Yang, Z., & Lei, J. (2017). Expectations of patient-centred care: Investigating IS-related and other antecedents. Information & Management, 54(5), 583–598. https://doi.org/10.1016/j.im.2016.11.009
Ellingsen, G., & Monteiro, E. (2012). Electronic patient record development in Norway: The case for an evolutionary strategy. Health Policy and Technology, 1(1), 16–21. https://doi.org/10.1016/j.hlpt.2012.01.007
Hertzum, M., Ellingsen, G., & Melby, L. (2021). Drivers of expectations: Why are Norwegian general practitioners skeptical of a prospective electronic health record? Health Informatics Journal, 27(1), 1460458220987298. https://doi.org/10.1177/1460458220987298
Hanseth, O., & Bygstad, B. (2017). The ePrescription initiative and information infrastructure in Norway. In M. Aanestad, M. Grisot, O. Hanseth, & P. Vassilakopoulou (Eds.), Information infrastructures within European health care: Working with the installed base (pp. 73–87). Springer International. https://doi.org/10.1007/978-3-319-51020-0_6
Skogås, J. G., Myhre, H. O., Ødegård, A., & Kiss, G. (2016). Imaging for minimally invasive surgery. Surgical Science, 7(8), 333–341. https://doi.org/10.4236/ss.2016.78048
Bouget, D., Jørgensen, A., Kiss, G., Leira, H. O., & Langø, T. (2019). Semantic segmentation and detection of mediastinal lymph nodes and anatomical structures in CT data for lung cancer staging. International Journal of Computer Assisted Radiology and Surgery, 14(6), 977–986. https://doi.org/10.1007/s11548-019-01948-8
Pedersen, A., Valla, M., Bofin, A. M., De Frutos, J. P., Reinertsen, I., & Smistad, E. (2021). FastPathology: An open-source platform for deep learning-based research and decision support in digital pathology. IEEE Access, 1–1. https://doi.org/10.1109/ACCESS.2021.3072231
Faraj, S., Pachidi, S., & Sayegh, K. (2018). Working and organizing in the age of the learning algorithm. Information and Organization, 28(1), 62–70. https://doi.org/10.1016/j.infoandorg.2018.02.005
Pachidi, S., Berends, H., Faraj, S., & Huysman, M. (2021). Make way for the algorithms: Symbolic actions and change in a regime of knowing. Organization Science, 32(1), 18–41. https://doi.org/10.1287/orsc.2020.1377
Orlikowski, W. J., & Scott, S. V. (2016). Digital work: A research agenda. In A research agenda for management and organization studies. Edward Elgar.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Open Access This chapter is licensed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license and indicate if changes were made.
The images or other third party material in this chapter are included in the chapter's Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the chapter's Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder.
Copyright information
© 2022 The Author(s)
About this chapter
Cite this chapter
Trocin, C., Skogås, J.G., Langø, T., Kiss, G.H. (2022). Operating Room of the Future (FOR) Digital Healthcare Transformation in the Age of Artificial Intelligence. In: Mikalef, P., Parmiggiani, E. (eds) Digital Transformation in Norwegian Enterprises . Springer, Cham. https://doi.org/10.1007/978-3-031-05276-7_9
Download citation
DOI: https://doi.org/10.1007/978-3-031-05276-7_9
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-031-05275-0
Online ISBN: 978-3-031-05276-7
eBook Packages: Computer ScienceComputer Science (R0)