Abstract
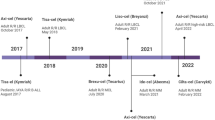
The development of genetically modified chimeric antigen receptor (CAR) T-cells to target cancer by conferring tumour antigen recognition has tremendously improved the fight against the disease and broadened treatment options for haematological malignancies (Elsallab et al. 2020b). However, in contrast to conventional drugs that patients can easily access, the implementation of CAR-T-cell therapy in routine clinical practice poses significant challenges. Access to CAR-T-cell products is currently limited to specific certified centres meeting the requirements set up by manufacturers and regulatory agencies. There are also issues regarding insurance coverage, reimbursement, affordability, and pricing, which have critical impacts on broadening patient access to these novel therapies (Abou-El-Enein et al. 2016a, b). Current list pricing ranges between $373,000 and $475,000 per one-time infusion for the four CAR-T-cell therapies currently approved by the FDA (tisagenlecleucel, Kymriah®; axicabtagene ciloleucel, Yescarta®; brexucabtagene autoleucel, Tecartus®; lisocabtagene maraleucel, Breyanzi®). In addition to the cost of the CAR-T-cell product, patient preparation (leukapheresis and/or lymphodepletion), product infusion, pre- and post-infusion patient management, and monitoring for side effects (Wagner et al. 2021) significantly add to the final price tag. There are calls for restructuring the current payment and reimbursement models to allow better access to CAR-T-cell therapies (Abou-El-Enein et al. 2014). However, this would only be possible after examining the strength of clinical evidence generated during product development (Abou-El-Enein and Hey 2019; Elsallab et al. 2020a) and, most importantly, by determining the value of CAR-T-cell therapy.
You have full access to this open access chapter, Download chapter PDF
Similar content being viewed by others
The development of genetically modified chimeric antigen receptor (CAR) T-cells to target cancer by conferring tumour antigen recognition has tremendously improved the fight against the disease and broadened treatment options for haematological malignancies (Elsallab et al. 2020b). However, in contrast to conventional drugs that patients can easily access, the implementation of CAR-T-cell therapy in routine clinical practice poses significant challenges. Access to CAR-T-cell products is currently limited to specific certified centres meeting the requirements set up by manufacturers and regulatory agencies. There are also issues regarding insurance coverage, reimbursement, affordability, and pricing, which have critical impacts on broadening patient access to these novel therapies (Abou-El-Enein et al. 2016a, b). Current list pricing ranges between $373,000 and $475,000 per one-time infusion for the five CAR-T-cell therapies currently approved by the FDA (tisagenlecleucel, Kymriah®; axicabtagene ciloleucel, Yescarta®; brexucabtagene autoleucel, Tecartus®; lisocabtagene maraleucel, Breyanzi®; idecabtagene vicleucel, Abecma®). In addition to the cost of the CAR-T-cell product, patient preparation (leukapheresis and/or lymphodepletion), product infusion, pre- and post-infusion patient management, and monitoring for side effects (Wagner et al. 2021) significantly add to the final price tag. There are calls for restructuring the current payment and reimbursement models to allow better access to CAR-T-cell therapies (Abou-El-Enein et al. 2014). However, this would only be possible after examining the strength of clinical evidence generated during product development (Abou-El-Enein and Hey 2019; Elsallab et al. 2020a) and, most importantly, by determining the value of CAR-T-cell therapy.
Efficacy does not automatically entail value. Quality-adjusted life years (QALYs) per dollar spent reflect a well-accepted measure of cost-effectiveness to assess value. QALYs enable evaluation of the impact of a certain therapy on the entire lifespan of a patient (quantity of life) and on health-related quality of life (HRQoL), reflecting a main parameter of treatment outcomes (Whitehead and Ali 2010). As composite estimates of mortality and morbidity, QALYs are conventionally calculated by accumulating life years attained from a utility value specific to certain health states. Preference elicitation studies in patients with a certain medical condition, such as in clinical trial scenarios, or in the general population serve as the basis to derive this utility value (Prieto and Sacristán 2003; Whitehead and Ali 2010; Sanders et al. 2016; Fiorenza et al. 2020).
Various models have been utilized to assess the cost-effectiveness of CAR-T-cell therapy. With respect to Kymriah® and Yescarta®, Lin et al. used a decision analytic Markov model and data from multicentre single-arm trials from a US health payer perspective for patients with relapsed or refractory (r/r) adult large B-cell lymphoma. CAR-T-cell therapies were compared to salvage chemotherapy and stem cell transplantation by incorporating certain assumptions regarding long-term effectiveness in the model. Yescarta® was shown to prolong life expectancy by 8.2 years at $129,000/QALY gained (95% uncertainty interval, $90,000 to $219,000) when assuming a 40% 5-year progression-free survival (PFS). Kymriah® led to an increase of 4.6 years at $168,000/QALY gained (95% uncertainty interval, $105,000 to $414,000/QALY) when assuming a 35% 5-year PFS (Lin et al. 2019). The study indicated that lowering the list price of Yescarta® and Kymriah® to $250,000 and $200,000 in the US, respectively, or implementing payment only for an initial complete response (at current prices) would enable both CAR-T-cell therapies to cost less than $150,000/QALY even at the more conservative assumption of a 25% 5-year PFS (Lin et al. 2019). Using data of paediatric patients with r/r B-cell ALL, Sarkar et al. built a microsimulation model to measure the incremental cost-effectiveness ratio (ICER) (Sanders et al. 2016) comparing CAR-T-cell therapy to standard of care, considering ICERs below a threshold of $100,000 per QALY as cost-effective (Sarkar et al. 2019). Assuming a 76% 1-year survival, they demonstrated an increase in overall cost by $528,200 with improved effectiveness by 8.18 QALYs, leading to an ICER of $64,600/QALY. However, if the assumption was modified to 57.8% 1-year survival, CAR-T-cell therapy in paediatric B-ALL patients was no longer cost-effective. While probabilistic sensitivity analysis showed CAR-T-cell therapy to be cost-effective in approximately 95% of iterations at a level of willingness to pay $100,000/QALY (Sarkar et al. 2019), assumptions made regarding long-term outcomes in both models need to be confirmed by real-world data with longer follow-up duration to enable robust validation of study outcomes.
When discussing value-based considerations, social value gained by CAR-T-cell therapy in the long term should also be taken into account. Offering a cure to paediatric cancer patients would enable them to lead a more productive life (Fiorenza et al. 2020). Moreover, successful milestones reached with respect to patenting (Jürgens and Clarke 2019) and regulatory and clinical success (Elsallab et al. 2020b) will increase public recognition, financial support, and advancements in the entire cellular therapy field. A recent study applied an economic framework to measure the social value of CAR-T-cell therapy as a sum of consumer surplus and profit for the manufacturing company (Thornton Snider et al. 2019). Consumer surplus reflected the difference between the added value of health gains achieved by the therapy and its incremental cost, accounting also for indirect costs and patient benefits. The gained social value was determined to be as much as $6.5 billion and $34.8 billion for paediatric ALL and DLBCL, respectively, with a net social value gain of $952,991 per child treated for B-ALL, even after including costs for production and treatment. However, they also showed a critical effect of treatment delays that negatively affect the social value generated by CAR-T-cell therapy, with a 1, 2, or 6 month treatment delay leading to a 9.8%, 36.2%, and 67.3% loss of social value, respectively, for paediatric ALL patients and a 4.2%, 11.5%, and 46.0% loss of social value, respectively, for patients with DLBCL (Thornton Snider et al. 2019). Thus, timely patient access is a key factor in the level of value achieved. Other key parameters to optimize the value of CAR-T-cell therapies rely on improving response rates, minimizing the risk of relapse and lowering the costs of toxicity management (Fiorenza et al. 2020).
Although CAR-T-cell therapy is undoubtedly transforming the therapeutic landscape for cancer patients, significant economic challenges ought to be addressed to allow broader and fairer access to these new therapies. Since most cost-effectiveness models are highly assumption-sensitive, a longer follow-up duration is warranted to better assess the value of CAR-T-cell therapies compared to alternative approaches.
-
CAR-T-cells have emerged as an important therapeutic approach for many cancer patients; however, issues regarding insurance coverage, reimbursement, affordability and pricing impact access to these novel therapies.
-
Short-term clinical data have demonstrated the potential of CAR-T-cells to become a cost-effective approach for cancer patients, but availability of long-term clinical outcomes will be required to achieve this goal.
-
The value of such a novel therapeutic modality should also be evaluated within the social gains of cancer patients resuming normal and productive lifestyles. However, these gains are dramatically influenced by delays in receiving the treatments.
References
Abou-El-Enein M, Hey SP. Cell and gene therapy trials: are we facing an “evidence crisis”? EClinicalMedicine. 2019;7:13–4. https://doi.org/10.1016/j.eclinm.2019.01.015.
Abou-El-Enein M, Bauer G, Reinke P. The business case for cell and gene therapies. Nat Biotechnol. 2014;32(12):1192–3. https://doi.org/10.1038/nbt.3084.
Abou-El-Enein M, Elsanhoury A, Reinke P. Overcoming challenges facing advanced therapies in the EU market. Cell Stem Cell. 2016a;12:293–7. https://doi.org/10.1016/j.stem.2016.08.012.
Abou-El-Enein M, et al. Putting a price tag on novel autologous cellular therapies. Cytotherapy. 2016b;18(8):1056–61. https://doi.org/10.1016/j.jcyt.2016.05.005.
Elsallab M, Bravery CA, et al. Mitigating deficiencies in evidence during regulatory assessments of advanced therapies: a comparative study with other biologicals. Mol Ther. 2020a;18:269–79. https://doi.org/10.1016/j.omtm.2020.05.035.
Elsallab M, Levine BL, et al. CAR-T-cell product performance in haematological malignancies before and after marketing authorisation. In: The lancet oncology. Amsterdam: Elsevier; 2020b. p. 104–16. https://doi.org/10.1016/S1470-2045(19)30729-6.
Fiorenza S, et al. Value and affordability of CAR-T-cell therapy in the United States. Bone Marrow Transplant. 2020;55(9):1706–15. https://doi.org/10.1038/s41409-020-0956-8.
Jürgens B, Clarke NS. Evolution of CAR-T -cell immunotherapy in terms of patenting activity. Nat Biotechnol. 2019;37(4):370–5. https://doi.org/10.1038/s41587-019-0083-5.
Lin JK, et al. Cost effectiveness of chimeric antigen receptor T-Cell therapy in multiply relapsed or refractory adult large B-cell lymphoma. J Clin Oncol. 2019;37(24):2105–19. https://doi.org/10.1200/JCO.18.02079.
Prieto L, Sacristán JA. Problems and solutions in calculating quality-adjusted life years (QALYs). Health Qual Life Outcomes. 2003;1:80. https://doi.org/10.1186/1477-7525-1-80.
Sanders GD, et al. Recommendations for conduct, methodological practices, and reporting of cost-effectiveness analyses. JAMA. 2016;316(10):1093. https://doi.org/10.1001/jama.2016.12195.
Sarkar RR, et al. Cost-effectiveness of chimeric antigen receptor T-cell therapy in pediatric relapsed/refractory B-cell acute lymphoblastic leukemia. J Natl Cancer Inst. 2019;111(7):719–26. https://doi.org/10.1093/jnci/djy193.
Thornton Snider J, et al. The potential impact of CAR-T-cell treatment delays on society. Am J Manag Care. 2019;25(8):379–86.
Wagner DL, et al. Immunogenicity of CAR-T cells in cancer therapy. Nat Rev Clin Oncol. 2021. https://doi.org/10.1038/s41571-021-00476-2.
Whitehead SJ, Ali S. Health outcomes in economic evaluation: the QALY and utilities. Br Med Bull. 2010;96(1):5–21. https://doi.org/10.1093/bmb/ldq033.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Open Access This chapter is licensed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license and indicate if changes were made.
The images or other third party material in this chapter are included in the chapter's Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the chapter's Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder.
Copyright information
© 2022 The Author(s)
About this chapter
Cite this chapter
Abou-el-Enein, M., Gauthier, J. (2022). The Value of CAR-T-cell Immunotherapy in Cancer. In: Kröger, N., Gribben, J., Chabannon, C., Yakoub-Agha, I., Einsele, H. (eds) The EBMT/EHA CAR-T Cell Handbook. Springer, Cham. https://doi.org/10.1007/978-3-030-94353-0_46
Download citation
DOI: https://doi.org/10.1007/978-3-030-94353-0_46
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-94352-3
Online ISBN: 978-3-030-94353-0
eBook Packages: MedicineMedicine (R0)