Abstract
Under current European Union regulations, CAR-T cell therapies fall under the advanced therapy medicinal products (ATMPs) framework. ATMPs represent a category of medicinal products defined in EU Regulation 1394/2007 and subdivided into four categories, of which autologous or allogeneic CAR-T cells, among other therapies, are considered gene therapy medicinal products (GTMPs). ATMPs are subject to a centralized evaluation framework whereby one authorization is valid for all countries in the EU led by the European Medicines Agency’s Committee for Advanced Therapies (CAT). The framework includes different regulatory pathways for bringing ATMPs from clinical trials to market authorization, and the regulatory pathway taken will depend on a product’s characteristics and the target patient population. In 2018, two chimeric antigen receptor (CAR) T cell therapies, Yescarta and Kymriah, completed their authorization process via the priority medicines PRIME scheme to Marketing Authorization (Detela and Lodge 2019).
You have full access to this open access chapter, Download chapter PDF
Similar content being viewed by others
Current Framework
Under current European Union regulations, CAR-T cell therapies fall under the advanced therapy medicinal products (ATMPs) framework. ATMPs represent a category of medicinal products defined in EU Regulation 1394/2007 and subdivided into four categories, of which autologous or allogeneic CAR-T cells, among other therapies, are considered gene therapy medicinal products (GTMPs). ATMPs are subject to a centralized evaluation framework whereby one authorization is valid for all countries in the EU led by the European Medicines Agency’s Committee for Advanced Therapies (CAT). The framework includes different regulatory pathways for bringing ATMPs from clinical trials to market authorization, and the regulatory pathway taken will depend on a product’s characteristics and the target patient population. In 2018, two chimeric antigen receptor (CAR) T cell therapies, Yescarta and Kymriah, completed their authorization process via the priority medicines PRIME scheme to Marketing Authorization (Detela and Lodge 2019).
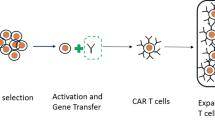
The production, distribution, and administration of ATMPs require a completely different organization plan than that used for HSCT, with manufacturing typically at a central facility in compliance with good manufacturing practices (GMPs), a version of which was released in 2017 by the European Commission to specifically deal with the manufacturing of ATMPs.Footnote 1 Since a majority of the ATMPs that progress to authorization or at least to clinical trials are manufactured from autologous mononuclear cells, starting material is usually procured by hospital- or blood bank-operated apheresis facilities, creating a peculiar situation in which a product starts under one regulation—EU Tissues and Cells DirectivesFootnote 2—before passing to another—ATMP Regulation- and in which a hospital acts as a service provider to industry, an interaction that requires further definition of the respective responsibilities and liabilities (McGrath and Chabannon 2018). The Tissues and Cells Directives, which cover all steps in the transplant process from donation, procurement, testing, processing, preservation, storage, and distribution, are undergoing a review that is expected to lead to a legislative proposal by the European Commission in late 2021, and it is anticipated that the new framework will further consider how products cross the interface between the two frameworks.
Given the high toxicity profile of CAR-T cell therapies, marketing authorization may be subject to conditions that lead to a risk management plan (RMP). The RMP for the currently authorized CAR-T therapies includes the need for manufacturers to qualify the sites that will treat patients. Site qualification is addressed below.
Hospital Exemption
In recognizing that many potential ATMPs are used for limited numbers of patients and with little commercial interest, Regulation 1394/2007 created the so-called hospital exemption (HE) under Article 28, exempting from authorization requirements those ATMPs manufactured in hospitals or universities where the medicine is prescribed for individual patients under the care of a medical practitioner. This manufacturing should occur on a nonroutine basis according to specific quality standards (GMPs) and only within the same member state.
In February 2021, the Spanish pharmaceutical regulator AEMPS authorized the first CAR-T cell therapy approved by a European national authority under the hospital exemption clause for the ARI-0001 CAR-T developed by the Hospital Clinic in Barcelona.Footnote 3
National authorities oversee the approval of HE products, which has resulted in significant variations between member states in how approval is applied, in turn leading to criticism from both industry and academia that the approval process is unclear and inconsistent.
Role of Academia
Academia remains very active in the early phases of clinical trials designed to evaluate innovative GTMPs as potential complements, substitutes, or bridges to historical forms of haematopoietic cell transplants. One recent study calculated that even now, when industry interest in these therapies has increased significantly in the last 5–6 years, over 50% of CAR-T cell trials in the USA are still sponsored by academia (Kassir et al. 2020). Many public institutions have invested significant resources to upgrade their processing facilities to GMP-compliant levels, thus allowing for small-scale manufacturing of experimental medicinal products to support phase I and possibly phase II studies. Furthermore, academia must become a proactive stakeholder in the regulatory area by engaging with the authorities, sharing their know-how and voicing their opinion. Through continental registries, such as EBMT, academic institutions will continue to play a key role due to their data and procedural knowledge, which will be very useful not only for researchers but also for industry, health care regulators and payers (Hildebrandt 2020).
Health Technology Assessment
For a marketing authorization holder, approval by EMA is just one step. To gain market access in the EU, the manufacturer must now approach national health care reimbursement authorities, collectively known as health technology assessment (HTA) bodies, who will assess the cost of the added value of novel therapies compared to the current standard of care. Unlike the centralized authorization process, HTA assessments are performed at the national level and are subject to great variability between member states. Over the past decade, the EU has pursued a more harmonized HTA process across Europe, although there remains significant resistance among member states, and a legislative proposal adopted by the Commission in early 2018 is only very slowly progressing through the parliamentary process.
Future Focus
Access to ATMPs, including cellular therapies, is likely to be a particular challenge for patients, health care professionals, and national health systems due to their expected high costs and complexity. Foreseeable changes to the regulatory framework could see closer alignment with MA and HTA to make them more concurrent and less sequential processes. The EMA’s strategy for big data places an emphasis on using real-world data (RWD) to support regulatory decisions, and significant efforts are being made to prepare the structures to support this move. Accelerated processes, such as PRIME, will continue to evolve as regulators gain more knowledge and the science and medicine develop. The interplay between European medicinal product regulations and genetically modified organism (GMO) frameworks will likely continue to be the focus of efforts to harmonize interpretations across the EU. Regulators will see more automation of manufacturing processes, which should help reduce risk and variability, while decentralized or ‘bedside’ manufacturing could become more common but still need regulatory approval and oversight. Allogeneic CAR-T products will also require substantial evidence to reassure regulators regarding safety concerns about graft versus host disease, cell rejection, and the risks associated with gene editing. Data protection measures under the General Data Protection Regulation (GDPR) for health-related personal data could see adaptations to better facilitate secondary use of data collected to support investigational and regulatory needs.
Centre Qualification by Competent Authorities and Manufacturers
Shared Goals
A high degree of competencies is required from centres involved in CAR-T cell therapies by both the competent authorities and the manufacturers. With regard to centre qualification, authorities and manufacturers share at least some own goals, which is minimizing CAR-T cell therapy-associated risks for patients to deliver safe and efficient therapy. Authorities at the international, national, or regional levels assess the quality of care, level of practice and health outcomes, and qualify centres that successfully demonstrate high standards of health care and patient safety. For a manufacturer, accreditation by the competent authority verifies that the required standards are followed and the necessary qualifications, processes and resources are present. From the centre’s perspective, receiving necessary accreditations and approvals from both the competent authority and the respective manufacturer is a prerequisite to support concrete CAR-T cell therapy.
Centre Assessment
The presence of accreditation by a competent authority is among the first items checked by a manufacturer during the so-called feasibility assessment. The other reviewed items include the scope of authorized activities; the centre’s ability to perform particular procedures and tests, incorporate the manufacturer’s requirements, and guarantee specific environmental conditions; and the presence of requested equipment and qualified personnel. For a manufacturer, the assessment is a great chance to obtain a better understanding of a centre’s setup and daily routine and its procedural and capacity constraints. The assessment might also reveal gaps, such as the inadequateness or complete absence of required processes. Generally, the feasibility assessment is a unique opportunity to evaluate prospective candidates for collaboration, and it precedes all other steps in a centre’s qualification by a manufacturer, which may vary in scope and detail depending on the particular therapy.
Centre Auditing
The centre qualification audit is usually performed by a manufacturer prior to commencement of any collaboration. The aim is to evaluate compliance with applicable regulatory requirements and the centre’s own procedures or policies. Manufacturers obtain an appropriate understanding of the performed services and the robustness of engaged systems, including quality management, personnel training, and the capacity of available resources. They usually request some of the centre’s internal documents and process details to be shared prior to the audit to allow for a thorough review. During the audit, auditors examine more of the centre’s documentation, interview personnel, inspect the facility’s key locations, and evaluate processes in targeted functional areas.
In the course of an established collaboration, other types of audits can be organized. The so-called surveillance audit is a periodic audit to ensure that a centre is continuing to comply with the required standards. The emphasis is on reviewing significant changes that have occurred in the relevant procedures, facility and its quality system since the qualification audit. A follow-up on any previous audit findings, including the implementation of corrective and preventive actions, is also a common part of surveillance audits, which are usually performed every 2–3 years.
A for-cause audit can be called in response to serious circumstances, including deficiency in meeting regulatory requirements, occurrence of a major deviation, repeated deviations, or the risk or occurrence of patient safety issues. This audit generally focuses on identified nonconformities and areas of manufacturer concern.
Any type of audit will result in an audit report, which lists audit observations or findings that might be evaluated for significance as minor, major, or critical. In response to a finding, a centre’s own internal procedure usually mandates insurance of a corrective action. This frequently means strengthening the existing processes or creation of brand-new processes. Acceptable responses to audit findings are required to close an audit.
Centre Training
Audited centres are further qualified by the manufacturers for support of concrete CAR-T cell therapy. Manufacturers usually do not aim to boost personnel’s general knowledge or the skills and attitudes required for daily routine practice. Their focus is on explaining the specificities of clinical trials or authorized therapies, with few differences between the requirements of the two categories. Generally, the critical parameters of procedures and products are explained, as well as timelines, environmental conditions, types of equipment and material, completion and usage of involved documents, and principles of communication among stakeholders. Due to the complexity of CAR-T cell therapies, centre personnel qualified by manufacturers perform a wide range of functions. Manufacturers usually train those involved in patient or donor care; starting material procurement, processing, intermediate storage, packaging, release, and testing; completion of documents; and ATMP receipt, storage, thawing and administration. In practice, these functions involve physicians, nurses, pharmacists, apheresis and laboratory technicians, and administrative workers.
Required procedure parameters include duration limits, processed volume targets, type of anticoagulant, environmental conditions (such as temperature and humidity), and methods of disconnecting and sealing collection bags. Product parameters that manufacturers like to specify include targets for collected volume, yield and purity and the required number of units and samples. With regard to timelines, the importance of procedure scheduling and harmonization with other procedural steps or treatment sessions is emphasized. Manufacturers are usually very clear about the type of equipment and material required for procurement, intermediate storage, indoor transport, the processing and packaging of starting material or storage, and thawing and administration of ATMPs. The purpose and usage of the involved documents are explained, and instructions for completing, archiving, or sharing with other stakeholders are provided. Colour-coded sample documents, prepopulated forms, and checklists are among the most frequent support materials.
Centre qualification is not bound to its on-site execution. It can also be performed remotely when travel or visitor restrictions or social distancing guidelines make any externally driven on-site activities impossible. Internet-based applications, teleconferencing tools, and purposely developed virtual procedures have recently been successfully used by manufacturers to perform feasibility assessments, audits, and trainings.
Key Points
-
CAR-T cell therapy falls under the ATMP framework, presenting challenges to all stakeholders, including health care providers and patients.
-
Regulatory issues concern not only marketing authorization but also mechanisms for cost–benefit assessment and, less directly, GMOs and data protection.
-
Academia will continue to play a significant role in the development and delivery of these new therapies and should expect to engage with other stakeholders.
-
The regulatory framework is not static and evolves with experience and knowledge.
-
Competent authorities and manufacturers have a common goal, which is minimizing CAR-T cell therapy-associated risks for patients.
-
Accreditation of a centre by a competent authority is understood as verification that the required standards are followed and the necessary qualifications, processes and resources are present.
-
Manufacturers qualify centres for support of a concrete CAR-T cell therapy and focus on the specificities of a particular project.
-
Centre qualification is not bound to on-site execution and can be performed remotely using internet-based applications, teleconferencing tools, and purposely developed virtual procedures.
Sources of Information
-
World Health Organization—Patient Safety [Internet]. 13 September 2019. Available from: https://www.who.int/news-room/fact-sheets/detail/patient-safety (Accessed February 2021)
-
Yakoub-Agha I, Chabannon C, Bader P, Basak GW, Bonig H, Ciceri F, Corbacioglu S, Duarte RF, Einsele H, Hudecek M, Kernsten MJ, Köhl U, Kuball J, Mielke S, Mohty M, Murray J, Nagler A, Robinson S, Saccardi R, Sanchez-Guijo F, Snowden JA, Srour M, Styczynski J, Urbano-Ispizua A, Hayden PJ, Kröger N. Management of adults and children undergoing chimeric antigen receptor T-cell therapy: best practice recommendations of the European Society for Blood and Marrow Transplantation (EBMT) and the Joint Accreditation Committee of ISCT and EBMT (JACIE) [Internet]. February 2020. Available from: https://haematologica.org/article/view/9515 (Accessed February 2021)
-
Taylor L, Rodriguez ES, Reese A, Anderson K. Building a Program—Implications for infrastructure, nursing education, and training for CAR-T cell therapy. Clin J Oncol Nurs. 2019 Apr 1;23(2):20–26. https://doi.org/10.1188/19.CJON.S1.20-26. [Internet]. Available from: https://pubmed.ncbi.nlm.nih.gov/30880820/ (Accessed February 2021)
-
Black A, Gabriel S, Caulfield D. Implementing chimeric antigen receptor T-cell therapy in practice. The Pharmaceutical Journal [Internet]. 22 May 2020. Available from: https://pharmaceutical-journal.com/article/ld/implementing-chimeric-antigen-receptor-t-cell-therapy-in- practice (Accessed February 2021)
-
Quality System Audit Program—Activate apheresis and cell collection sites faster by licensing GTP audit results. Be The Match BioTherapies. [Internet]. Available from: https://bethematchbiotherapies.com/solutions/quality-system-audit-program/ (Accessed February 2021)
-
Vincinis R. Major vs. Minor Audit Findings. The Auditor. [Internet]. Available from: https://www.theauditoronline.com/major-vs-minor-audit-findings/ (Accessed February 2021)
Notes
- 1.
Guidelines of 22.11.2017 Good Manufacturing Practice for Advanced Therapy Medicinal Products. EudraLex The Rules Governing Medicinal Products in the European Union Volume 4 Good Manufacturing Practice.
- 2.
Directive 2004/23 of the European Parliament and of the Council of 31 March 2004 on setting standards of quality and safety for the donation, procurement, testing, processing, preservation, storage, and distribution of human tissues and cells.
- 3.
References
Detela G, Lodge A. EU regulatory pathways for ATMPs: standard, accelerated and adaptive pathways to marketing authorisation. Mol Therap Method Clin Develop. 2019;13:205–32. https://doi.org/10.1016/j.omtm.2019.01.010.
Hildebrandt M. Horses for courses: an approach to the qualification of clinical trial sites and investigators in ATMPs. Drug Discov Today. 2020;25(2):265–8. https://doi.org/10.1016/j.drudis.2019.10.003.
Kassir Z, et al. Sponsorship and funding for gene therapy trials in the United States. JAMA Am Med Assoc. 2020;323(9):890. https://doi.org/10.1001/jama.2019.22214.
McGrath E, Chabannon C. Regulatory aspects of ATMP versus minimally manipulated immune cells. In: The EBMT handbook: hematopoietic stem cell transplantation and cellular therapies. Springer; 2018. p. 461–4. https://doi.org/10.1007/978-3-030-02278-5_62.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Open Access This chapter is licensed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license and indicate if changes were made.
The images or other third party material in this chapter are included in the chapter's Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the chapter's Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder.
Copyright information
© 2022 The Author(s)
About this chapter
Cite this chapter
McGrath, E., Machalik, P. (2022). The Regulatory Framework for CAR-T Cells in Europe: Current Status and Foreseeable Changes AND Centre Qualification by Competent Authorities and Manufacturers. In: Kröger, N., Gribben, J., Chabannon, C., Yakoub-Agha, I., Einsele, H. (eds) The EBMT/EHA CAR-T Cell Handbook. Springer, Cham. https://doi.org/10.1007/978-3-030-94353-0_37
Download citation
DOI: https://doi.org/10.1007/978-3-030-94353-0_37
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-94352-3
Online ISBN: 978-3-030-94353-0
eBook Packages: MedicineMedicine (R0)