Abstract
Energy and fatigue carry important implications for vitality and overall quality of life. Lacking energy and experiencing fatigue can be both burdensome as well as adaptive. This chapter first classifies energy and fatigue and then reviews their measurement. This chapter closes with opportunities for future directions.
Energy and fatigue are present under varying conditions including in daily performance, during and after acute physical or mental strain (capacity), and in the context of chronic conditions. Energy and fatigue have been measured both subjectively and objectively. Subjective outcomes can be derived from self-reported scales and prompts; objective outcomes may be derived from performance and capacity tasks and technology-reported physiological, biological, and behavioural markers. The scales and tasks employed to measure energy have been traditionally validated but may lack daily life context and ecological validity. Prompts and behavioural monitoring methods are emerging as promising alternatives.
Energy and fatigue have also been routinely monitored for specific diseases and occupations. However, fewer studies monitor healthy individuals through consumer technology in daily life contexts. More research is needed for an objective, unobtrusive, longitudinal, and contextual measurement of energy and fatigue in the healthy general population, in service of improving health, wellbeing, and quality of life.
You have full access to this open access chapter, Download chapter PDF
Similar content being viewed by others
Keywords
- Energy
- Fatigue
- Vitality
- Fatigue taxonomy
- Pathological fatigue
- Non-pathological fatigue
- Physical fatigue
- Fatigability
- Mental fatigue
- Burnout
- Fatigue scale
- Fatigue task
- Subjective measurement
- Objective measurement
- Mixed methods
- Validated scale
- Ecological momentary assessment
- Research sensor
- Consumer wearable
- Measurement property spectrum
- Longitudinal behaviour monitoring.
Introduction
There are many ways to conceptualize “Energy” and “Fatigue” in the context of the WHO Quality of Life domain [1]. Energy and fatigue may be interrelated but may also be considered orthogonal. Low energy can be characterized by fatigue, lack of motivation, and lack of interest, while states of excessive energy can reach pathological levels that include disrupted sleep, restlessness and agitation, or even mania [2]. Although lacking energy can be burdensome and uncomfortable, it is simultaneously an adaptive symptom that is perceived as a need to rest or slow down [3]. Given that energy is a valuable resource, efficient spending and conservation of energy may result in the greatest chances of vitality and even survival [4]. Curiously, one tends to think of energy as a resource that is depleted and then replenished with rest. It is also frequently observed that using energy may be synonymous with generating energy (e.g. one may feel more replenished after engaging in an activity than they do following rest). This curious paradox highlights the potential value of classifying and enhancing our understanding of energy. Fatigue is both a normative experience as well as associated with many chronic illnesses and psychiatric disorders. Fatigue can be characterized by subjective feelings of “tiredness” and “lack of energy” [5] and can serve as a signal to prevent strain, damage, and injury [6].
In this chapter, energy refers to the strength and vitality required for sustained physical or mental activity. Lack of energy or fatigue is used to describe the subjective sensation (perceived fatigue) as well as the objective and quantifiable change in performance (fatigability ) [7]. Fatigue can be classified as pathological or non-pathological. Pathological fatigue can be described as an overwhelming sense of tiredness at rest, exhaustion with activity, lack of energy that precludes daily tasks, or loss of vigour [7]. In healthy adults, non-pathological fatigue is predictable and does not interfere with usual daily activities. Non-pathological fatigue is typically brought about by prolonged exertion and diminishes with rest [8]. In addition to pathological and non-pathological fatigue, fatigue may also be subdivided as either physical or mental (cognitive/psychiatric) and further subdivided as primary (neurological) or secondary (non-neurological) [7,8,9,10]. Furthermore, performance refers to an individual’s functioning in their daily environment while capacity refers to the maximal or optimized level of functioning.
Preliminary studies were conducted on energy and fatigue during the First World War when researchers investigated the impact of fatigue on efficiency and productivity of the industrial workforce [11]. This “occupational fatigue” continues to be a focus of research attention, especially in vocations and occupations in which fatigue carries serious implications. Traditionally, energy and fatigue have been assessed using qualitative, self-reported outcomes [12] and can be obtained from a number of validated scales [13, 14]. Most clinical fatigue studies use self-report measures that can broadly be classified as measuring perceptions of fatigue [8]. Despite the numerous scales that measure fatigue, there is no agreed-upon standard of which to compare subjective reports of fatigue [15, 16].
The use of technology to monitor and manage energy and fatigue has been investigated in order to help healthy individuals continue to live healthily [3, 6, 17], assist individuals with health issues [18,19,20], and address vocational or occupational fatigue to improve personal and workplace safety [21,22,23]. The monitoring of energy and fatigue helps individuals adapt their effort in recreational (e.g., amateur sport, exercise) and occupational (e.g., drivers, pilots, police officers, professional athletes, shift workers) settings to prevent negative effects (e.g., burnout, exhaustion, accidents, injury) and maintain quality of life [24, 25]. Further, energy and fatigue research is needed to examine their connection to underlying or potential health conditions as well as interventional studies to validate the operationalization of energy and fatigue monitoring in daily life.
In this chapter, we will classify energy and fatigue and present their measurement. The chapter is structured as methods of our work, classification of energy and fatigue (pathological as well as non-pathological), measurement and assessment of energy and fatigue, discussion of results, and conclusive remarks.
Methods
We conducted a scoping review of the existing literature between 2010 and 2020 in Google Scholar on the technology-enabled assessment of energy and fatigue. Search terms related to energy and fatigue (e.g., “fatigability”, “tiredness”) were coupled with terms pertaining to each of the following domains: (1) the population under study (e.g., “athlete”, “driver”), (2) the health outcomes (e.g., “circulation”, “dementia”, “heart”), and (3) the measurement (e.g., “accelerometer”, “electrocardiogram”, “wearable”). One example search phrase was “galvanic energy fatigue tiredness vitality”. We also reviewed the relevant references of the identified literature. Table 4.1 reviews the domains, search terms (selective), and the rationale for choosing the domain.
Results
We found 40 reviews on energy and fatigue pertaining to the domains and 60 studies assessing fatigue by using technology. The search results included in this review either (1) reviewed energy and fatigue assessment for a specific population and/or health outcome, (2) provided evidence for the use of measurement to monitor or manage energy or fatigue, or (3) discussed human factors of technology towards monitoring energy and fatigue. The taxonomy of fatigue resulting from our literature review is depicted in Fig. 4.1.
Energy and Fatigue Classification
Pathological Fatigue
Pathological fatigue is prolonged or chronic (>6 months), can be highly debilitating, and is much less common than non-pathological fatigue [27]. Pathological fatigue may be best understood as an amplified sense of normal (non-pathological) fatigue that can be induced by changes in one or more variables regulating work output [9]. For instance, a healthy individual may experience fatigue during or after exercising, but the same individual may perceive even more fatigue when exercising during an infectious disease [7]. Diseased individuals describe fatigue as an overwhelming sense of tiredness at rest, exhaustion with activity, loss of vigour, or lack of energy that precludes daily tasks, inertia or lack of endurance [28]. Pathological fatigue may be classified as physical or mental and is associated with multiple illnesses.
Physical Fatigue
Pathological physical fatigue includes neurological and non-neurological fatigue.
Neurological Fatigue
Neurological fatigue suggests that the physical expression of fatigue is mediated by central and peripheral mechanisms [27]. Therefore, neurological fatigue may be further classified as central or peripheral [9].
Central fatigue is generated at sites proximal to the peripheral nerves and referred to as a progressive decline in the ability to activate muscles voluntarily [29]. Central fatigue is due to impaired muscle performance that arises from the central nervous system [28]. A feeling of constant exhaustion is a characteristic of central fatigue [9]. Pathological central fatigue is found in Multiple Sclerosis, Traumatic Brain Injury, Parkinson’s Disease, and many others.
Mechanisms of peripheral fatigue are usually attributable to a neuronal or muscular origin. Peripheral fatigue results from a lack of response in the neuromuscular system after central stimulation [27]. Peripheral fatigue is characterized by the failure to sustain the force of muscle contraction [9]. Pathological peripheral fatigue is found in neuromuscular disorder, rhabdomyolysis, muscle ischemia, restless legs syndrome and more.
In many of the previously mentioned health conditions , physical inactivity is a contributing factor to the increased fatigue of the patient [30]. Deconditioning, as a result of restricted physical activity, results in large decreases in muscle mass and strength, as well as increased fatigue due to changes in muscle metabolism [31, 32]. Physical fatigue is also increasingly observed as a secondary outcome in many diseases and health conditions during the performance of everyday activities [32].
Non-Neurological Fatigue
The exact mechanism of how non-neurological disease causes fatigue is not fully understood [7]. However, there are indications that peripheral proinflammatory cytokines signal the central nervous system to initiate fatigue [33]. A common non-neurological cause of temporary fatigue is an infection or the common cold. Non-neurological causes of chronic fatigue include infectious diseases (human immunodeficiency virus, mononucleosis, Borreliosis, and chronic pancreatitis), hematologic disease (anaemia and hemochromatosis), dehydration, immunological disease (celiac disease), rheumatological disease, cardiac disease (heart failure and cardiomyopathy), endocrinologic disorder (diabetes, Addison’s disease, hypopituitarism, and hypothyroidism), renal disease (insufficiency and dialysis), lung disease (chronic obstructive lung disease and asthma), malnutrition (poor diet, irritable bowel disease, eating disorders and hypoproteinemia), liver disease, chronic pain, chronic fatigue syndrome, fibromyalgia, malignancy (cancer, sarcoma, lymphoma, and leukaemia), Gulf War disease, poisoning, mineral or vitamin deficiencies, drugs, or irradiation [7].
Drugs and medications may also be a cause of non-neurological fatigue. The drugs that cause fatigue include alcohol, antihistamines, benzodiazepines, antispasmodics, antiepileptic drugs, neuroleptics, and narcotics [7].
Mental Fatigue
Mental fatigue in the pathological domain includes cognitive and affective (psychological/psychiatric) fatigue. Cognitive fatigue has been studied in the context of MS [34], cancer [35], TBI [36], HIV [37], and other diseases. Affective fatigue is influenced by psychological factors (attitude, motivation, will, endurance, flexibility, inertia, persistence, concentration, and alertness) as well as psychiatric factors (depression, mania, psychosis, and addiction) [28]. Individuals with chronic fatigue report poorer mental health than their non-chronic fatigue counterparts [38].
Non-pathological Fatigue
In contrast to pathological fatigue, non-pathological fatigue is short term and remits with rest. Non-pathological fatigue is sometimes referred to as physiological fatigue in the scientific literature. Non-pathological fatigue alerts the individual to opportunity costs of current activities, as well as of the attraction of alternative activities [39]. Fatigue in healthy individuals is a universal experience and a natural occurrence after physical or mental efforts, usually relieved by rest. Research has examined biological explanations for pathological versus non-pathological fatigue [40], as well as self-report scales to distinguish fatigue associated disease from fatigue associated with healthy controls [41]. It has been reported that 55% of healthy individuals identified a physical sensation of fatigue and 24% identified a mental sensation of fatigue [26].
Physical Fatigue
From a physical perspective , fatigue is described as the inability of the muscles to maintain the required level of strength during exercise activities [42, 43]. It can also be characterized as an exercise-induced reduction in muscle’s capability to generate force. There is no single cause of physical fatigue [44] and physical fatigue includes both central and peripheral fatigue.
Central fatigue designates a decrease in voluntary activation of the muscle, whereas, peripheral fatigue indicates a decrease in the contractile strength of the muscle fibres and changes in the mechanisms underlying the transmission of muscle action potentials [45]. Central and peripheral fatigue is a common experience during sport and exercise activities.
The impact of physical fatigue on cognitive performance depends both on the intensity and the duration of the exercise [46, 47]. Prolonged physical exercise leading to dehydration and physical fatigue is associated with a reduction in cognitive performance [48].
Mental Fatigue
Mental fatigue includes cognitive and affective fatigue and is an unfocused mental state, characterized by distraction, frustration, or discomfort. Mental fatigue is a psychobiological state caused by prolonged periods of demanding cognitive activity and characterized by subjective feelings of “tiredness” and “lack energy” [4].
In terms of cognitive activities, mental fatigue may be defined as the perception of feeling cognitively fatigued after performing demanding cognitive activities that involve concentration, attention, endurance, or alertness [49]. In the cognitive domain, fatigability can be measured as a decline in the reaction time, a decline in accuracy on continuous performance tasks, or a probe task that is given before and immediately after a fatiguing cognitive task [50, 51]. This cognitive fatigue is associated with problems completing tests, particularly where there is a requirement to sustain high levels of effort over time [39]. The effects of mental fatigue on cognitive performance [4, 51,52,53], and the skilled performance of drivers [54] and air pilots [55], have been investigated. Mental fatigue also limits physical performance [56] through perceived exertion [5]. Similarly, mental fatigue, following the performance of cognitive tasks, impairs emotion regulation [57].
Affective fatigue is characterized by low mood, tiredness, weariness, and lethargy [39]. It has been reported that 21% of healthy individuals identified an affective sensation of fatigue [26]. Non-pathological affective fatigue includes self-regulatory fatigue, empathy fatigue, and other fatigue associated with emotional depletion (burnout).
Factors Influencing Fatigue
Pathological and non-pathological fatigue is influenced by numerous factors, such as age, gender, physical condition, diet, latency to last meal, mental status, psychological conditions, personality type, life experience, and the health status of the individual [7]. Most studies found more fatigue in women than in men [38, 58,59,60,61,62]. Inconsistent findings have been reported regarding age and fatigue [38, 58, 62, 63]. Additionally, a high level of formal education has been associated with a lower prevalence of fatigue [61, 64, 65].
Sleepiness and fatigue are distinct and interrelated. Sleepiness refers to an increased propensity to fall asleep [66], while fatigue refers to tiredness resulting from exertion or illness. Fatigue may be regarded as a motivational drive to rest [67] and non-pathological fatigue will usually remit with rest. Sleepiness is related to circadian and homeostatic influences and remits after sleep [68], but not after rest.
Energy and Fatigue Measures
Fatigue perception is frequently measured by self-report scales, while fatigability is frequently assessed by performance, capacity, and technology-reported measures [69]. Subjective measures include scales and prompts for assessment while objective measures include performance and capacity tasks (physical and cognitive), physiological measurements (cardiac, ocular, neural), and markers (biological and behavioural).
Subjective Measures
Fatigue perception is frequently measured by application of patient-reported outcomes (PRO) [12] through validated scales prompted for assessment. These scales may be administered momentarily, daily, monthly etc. through paper, web, or smartphone.
Scale Instruments
Scales for self-reporting may be unidimensional, evaluating a single property, or multidimensional, evaluating multiple properties [49]. These instruments address different aspects of fatigue and energy and some address more than one aspect. No single measure of fatigue adequately captures the complexity of the phenomenon [15]. Researchers have pointed out that “in developing fatigue scales, there is a “catch 22″ situation: before a concept can be measured, it must be defined, and before a definition can be agreed upon, there must exist an instrument for assessing phenomenology. There is, unfortunately, no “gold standard” for fatigue, nor is there ever likely to be” [13]. Table 4.2 in this section depicts several scale instruments routinely used to measure energy and fatigue. The majority of these energy/fatigue self-report scales were designed for pathologic populations, but have been applied to non-pathologic populations as well.
Considerations in choosing a particular scale include recall period, unidimensionality or multidimensionality, scale structure and length, and suitable population. Scales differ in their scope, some measuring severity only, and others duration and impact on a range of functions [14]. Fatigue measures have been evaluated for the number of symptoms assessed, dimensions of fatigue explored, the time frame of the assessment, scale, method, the population on which the scale was developed, and psychometric properties [13, 14].
Some applications of these scales are illustrated below. SF-36 and PROMIS have been used in traditional studies assessing fatigue in the general population [14, 81]. FQ, FSS, and MAF have been employed to assess workplace-related fatigue [82, 83]. POMS has been used to assess fatigue in bus drivers [84] and sport athletes [24]. Scales were also used in traditional studies to assess energy and fatigue in individuals with a plethora of diseases, e.g., cancer [85, 86], cardiovascular disease [87, 88], chronic obstructive pulmonary disease [89], diabetes [90], fibromyalgia [91], hearing loss [16], inflammatory bowel disease [92,93,94], lupus [95], major depressive disorder [96], multiple sclerosis [97,98,99], psoriasis [100], pulmonary arterial hypertension [101], renal disease [102], rheumatic disease [103, 104], sleep apnea [105], stroke [106, 107], and traumatic brain injury [10].
Smartphone collection of self-reported energy and fatigue data has been utilized in the context of multiple sclerosis [108], cancer-related fatigue [109], and bipolar disorder [110]. Smartphone data collection often incorporates validated scales. For example, a mobile phone application to collect data on self-reported fatigue for multiple sclerosis [108] incorporated PROMIS. Researchers concluded that a phone application incorporating PROMIS may be useful to provide estimates of fatigue to facilitate clinical monitoring of fatigue for clinic settings.
Momentary Assessments
The Ecological Momentary Assessment (EMA) is a technique that elicits a repeated , real-time measurement of behaviours or experiences as they occur in the naturalistic setting of an individual’s daily life. This method was originally developed to perform in situ data collection for behavioural medicine [111]. The Experience Sampling Method (ESM) aims to assess participant thoughts, behaviours, and feelings during daily life by collecting self-reports, triggered at various moments during the day [112]. The two terms (EMA and ESM) are used interchangeably, and in practice, they are measured using the same methods [113].
Traditional studies employing EMA/ESM assessed fatigue and fatigability in segments of the general population. For instance, this method has been applied to demographic groups, work settings, and disease populations. Specifically, the relationship between women’s passion for physical activity and vitality was examined using SF-36 scale [114]. Researchers have also employed POMS scale to examine occupational energy management strategies by hourly diary questions in academic workers [115]. A separate study examined the effects of breaks on regaining vitality in the workplace using an activation–deactivation adjective checklist [116]. Additionally, EMA/ESM assessment of energy/fatigue has been applied to disease populations including osteoarthritis ([117] researchers used SF-36 scale), kidney disease ([45] researchers used Daytime Insomnia Symptom Scale), and cancer ([118] researchers used a single-item fatigue intensity scale; [20] researchers used 10-point Likert scale for current fatigue).
Mobile-administered EMA/ESM has been applied to the management of diseases. For cancer and its treatment, fatigue is one of the most common and distressing side effects. Cancer-related fatigue causes disruption in all aspects of Quality of Life and may be a risk factor for reduced survival [119]. A mobile phone-based, symptom management system can assist in the management of chemotherapy-related toxicity in patients with breast, lung and colorectal cancer [109]. This system prompts patients to complete an electronic symptom questionnaire on their mobile phone twice a day. A systematic review of mobile apps for bipolar disorder [110] identified thirty-five symptom monitoring apps aiming at assisting users with symptom tracking.
Objective Fatigue and Energy Measures
Fatigability is primarily measured by quantifying the decline in one or more aspects of performance during the continuous performance of a prolonged task or comparing performance before and immediately after a prolonged performance of a separate fatigue-inducing task [8]. In pathological cases, individuals may experience fatigue even in activities of daily living [120]. When objectively measuring fatigue, it is important to indicate the domain examined and the task used to induce fatigability.
Fatigue-related decrements in task performance can be measured by following two common approaches. Ackerman [121] provides a classification of procedures for cognitive fatigue, and we argue that these same approaches pertain to physical fatigue as well. The indirect approach consists of the assessment of cognitive ability before and after a prolonged period of time during which effort may vary. The direct approach consists of the continuous measurement of fatigue during the difficult task. The benefits of the first method are that all participants can complete the same task, while the variation lies in the difference between ex-ante and ex-post fatigue among individuals. This method does not quantify the performance decrease as a continuous function of time. Conversely, the second method can monitor fatigue accumulation, but the tasks may vary. One example is vigilance tasks, where participants are required to maintain attention for target events while ignoring other stimuli [122, 123].
There is a distinction between capacity (describing a person’s ability to execute a task in a standardized, optimized, or controlled environment), capability (describing what a person can do in their daily environment), and performance (describing what a person actually does in their daily environment) [124]. Capacity is the composite of all the physical and mental capacities that an individual can draw on and performance is what individuals do in their current environment [125]. It is beyond the scope of this chapter to classify past studies as capturing capacity, capability, performance, or a combination.
Physical Assessment
The monitoring of fatigue and energy has been examined as an approach to maintain health, assist in disease management, and improve performance, productivity, and safety. A plethora of methods have been employed in order to monitor fatigue and energy: performance-reported outcomes (PerfRO) [12] for physical and cognitive fatigability, and tech-reported outcomes (TechRO) [12] from physiological processes (cardiac, ocular, neural) and markers (biologic, behavioural).
Fatigability is usually quantified as a decline in peak force (torque), power (velocity of muscle contraction), speed, fatigue index (force change over time), sense of effort, perception of effort, or accuracy of performance after performing a task, which requires physical effort [7]. Characteristics of tasks include exercise type, intensity, load, tested muscle, and physical environment [28].
The first dimension of physical performance fatigue is “physical capacity” (i.e., maximum performance). The two most common indicators of physical capacity are (1) the aerobic capacity and (2) the power output capacity. Measures of aerobic capacity include the maximal oxygen volume (VO2-max). Measures of power output include the peak power output. Momentary exercises leading to the assessment of these measures include aerobic and resistance training [98]. Example exercises routinely used, e.g., in professional sports players include various jump protocols, including squat and countermovement jumps, which can lead to indirect assessments of fatigability [24]. Direct measures of fatigue include a joint range of motion or flexibility of appendages such as the knee, hip, groin, and other joints during the exercise.
The second measured dimension of fatigue is “muscular strength.” Studies measuring muscular strength included momentary resistance training of various types (weight machines, free weights, resistance bands, cycling ergometers) and other strength training (specialized locomotor training, cycling, aquatics) [98], muscular oxygen consumption (mVO2), or electromyography (EMG).
The third dimension of fatigue is “mobility,” which is more commonly measured in cases of pathological fatigue. Mobility measures include the momentary 6-Minute Timed Walk (6MTW) [126], the Timed 25-Foot Walk [127], and the Timed Up & Go [128].
Exercise-specific hardware used for such exercises include treadmills, weight machines, free weights, and resistance bands. Technology-enhanced exercises include the robotic-assisted treadmill and functional electrical stimulation-assisted cycling [98], and transcranial magnetic stimulation [7]. Figure 4.2 depicts an example of hardware used to measure physical performance.
Hardware for physical performance example (ergometer). © Laufband Ergometer by Robowalk licensed under CC-BY-SA-4.0
Studies assessing non-pathological physical performance as a proxy for physical fatigue involved segments of the general population, e.g., physical fatigue in young adults using POMS, trail-making test on an iPad and mVO2 [129], physical fatigue during a sit-to-stand physical test by using EMG and accelerometer (Samsung) in the lab [130], or PhysioLab, a physiological computing toolbox measuring multiple signals (ECG, EMG, and EDA) to study cardiorespiratory fitness in elderly populations [131], all momentary.
Other observational studies assessed physical fatigue in a pathological context with individuals with health conditions or diseases; assessments include the effects of caloric restriction on cardiorespiratory fitness and fatigue in older adults with obesity by using graded exercise tests measuring VO2-max [132], the differences in motor fatigue between patients with stroke and patients with multiple sclerosis by using self-reported SF-36 and 6MWT [133], physical fatigue in lumbar disc herniation by using EMG [134].
Continuous monitoring studies assessed the effects of disease on fatigue, e.g., a rehabilitation program on aerobic fitness, cancer-related fatigue, and quality of life using subjective MFI and objective energy expenditure armbands (SenseWear) [135], or the fatigue monitoring system (FAMOS) which can monitor physiological parameters from multiple sclerosis patients and controls, all pathological.
Cognitive Assessment
In the cognitive domain , fatigue leads to the degradation of cognitive performance [122], as reflected by degradations in verbal, visual, short, and long-term memory, processing speed, primary and divided attention, verbal fluency, motor speed, reading speed, visual scanning, orientation, calculation, success rate, and other measures.
Cognitive assessments were measured by using numerous momentary measures, which collectively assess the above degradations. Table 4.3 reviews several task-based tests yielding cognitive performance-reported outcomes [12].
Cognitive performance studies included fatigue assessment in non-pathological segments of the general population, e.g., alertness, vitality, and sleepiness by using Psychomotor Vigilance Task (PVT) and other tasks in different lighting settings [146], occupational fatigue, e.g., in healthcare and medical staff by using the rate of error [147], or airline pilots on the flight deck by using PVT [148].
Cognitive performance studies also included fatigue assessment in pathological settings, e.g., the relationships between health-related Quality of Life, fatigue, and exercise capacity in coronary artery disease individuals using MFI and a bicycle ergometer test [149].
Technology-driven studies include assessments of mental fatigue in a non-pathological context by performing tasks with a computer, e.g., keyboard and mouse interaction patterns [150] recovery from work exhaustion by use of Twitter [151], or in a pathological context. For example, those living with an acquired brain injury often have issues with cognitive fatigue due to factors resulting from the injury. Studies have shown fatigue to be one of the most disabling symptoms, regardless of the severity of brain injury [152,153,154]. Researchers presented a smartphone application for the evaluation of cognitive fatigue, which can be used daily to track cognitive performance in order to assess the influence of fatigue [155]. Researchers concluded that the presented smartphone application for the evaluation of cognitive fatigue could be utilized in everyday life.
Cardiac Physiology
Cardiac activity measures used to assess fatigue include the resting heart rate (HR), exercise heart rate (HRex), heart rate variability (HRV), and the heart rate recovery (HRR). The heart rate may increase or decrease in response to a variety of factors including physical and mental effort, distress, and anxiety that are potentially associated with fatigue [16]. Elevated HRV was observed during strenuous tasks in individuals with chronic fatigue [156] and healthy individuals of young age while performing a task [157]. HRR may serve as a marker of acute training-load alteration, however recent studies showed inconclusive results [24]. A more detailed measure of heart activity is the electrocardiogram (ECG), an electrophysiological method , which records the electric signals of the heart and from which the HR can be derived. Figure 4.3 depicts an electrocardiogram with an electrocardiograph and electrodes placed on the human body.
Electrocardiogram. © Blausen Electrocardiogram by BruceBlaus licensed under CC-BY-3.0 [158]
Studies using the ECG to assess fatigue in a non-pathological, occupational context include airline crew [159], surgeons [160] or 3D TV watchers [161]. In these studies, the ECG was measured with electrode-based devices before and after the tiring task (i.e., via an indirect measurement approach). HRV pre- and post-task was used as a measure for fatigue in work settings, e.g., emergency and pre-hospital doctors [162].
Measurements of cardiac physiology have been performed during daily life (i.e., via a direct measurement approach) also in a non-pathological setting. A large body of research focused on assessing cardiac activity in healthcare and driving professionals. Medical interns were given Holter recorders throughout the day, measuring HR and HRV, in conjunction with resting ECG to assess fatigue [163]. Surgeon HRV (using EEG) was assessed in robot-assisted versus conventional cholecystectomy [164]. Drivers were assessed while driving, through an ECG device mounted on the steering wheel [165]. Another study assessed the impact of electroacupuncture on fatigue and Quality of Life using subjective SF-36 and objective HRV using ECG (SphygmoCor) [166]. A method aimed at estimating the perception of physical fatigue by predicting heart rate through smartphones has been proposed by estimating the oxygen consumption , using a smartphone acceleration and location (via accelerometer and GPS, respectively) [3]. The study yielded an adequate detection of fatigue when individuals performed daily-life activities under naturalistic conditions.
Ocular Physiology
Keeping the eye closed or having fixed changes in pupil diameter have been observed in a state of fatigue [167] due to monotony or sleep deprivation. Ocular physiology measures used for assessing fatigue include the spontaneous eye blink [168], pupil diameter [169], oscillations in pupil diameter (fatigue waves) [170, 171]. Another method used to detect fatigue is the electrooculogram (EOG), an electrophysiological method, which measures the resting electrical potential between the cornea and Bruch’s membrane.
Studies using ocular physiology measures were primarily done to assess fatigue in non-pathological, occupational settings, e.g., in the military detecting sleep deprivation-induced fatigue by saccade peak velocity in the Navy using questionnaires (on PDAs), actigraphy (Actiwatch), and EOG (Natus, then Embla) during a saccade task [172] or assessing fatigue in the Air Force through saccadic velocity using software (Eyelink) in a dark room before and after a long flight [22]. For driver drowsiness, studies assessed fatigue by EOG using a device mounted next to the eyes for brief periods [21].
Smartphones have been utilized and applied to drivers as well. Researchers have presented an app, which uses information from both front and back cameras and others embedded sensors on the phone to detect and alert drivers to dangerous driving conditions inside and outside the car [173]. Researchers used computer vision and machine learning algorithms on the phone to monitor and detect whether the driver is tired or distracted using the front camera while at the same time tracking road conditions using the back camera. The front camera pipeline tracks the driver’s head pose and direction as well as eyes and blinking rate as a means to infer drowsiness and distraction. Specifically, researchers used blink detection algorithms to detect periods of micro-sleep, fatigue and drowsiness. A more recent study improved EOG by mounting the device on the forehead to increase the duration of comfortable measurement [174].
Neural Physiology
Neural electrophysiological measures used to assess fatigue include the electroencephalogram (EEG), the evoked response potential (ERP), the Error Related Negativity, and lateralized readiness potential [16]. Magnetic resonance imaging (MRI) was also used to identify factors of fatigue [175]. This type of objective measure focuses on cognitive performance, described in a preceding section, by requiring the participants to conduct a task while monitoring takes place.
Studies have assessed neural physiology of fatigue in a non-pathological context by using EEG or ERP in the general population [176, 177], as well as EEG on occupational fatigue, e.g., drivers [178, 179], and surgeons while conducting a demanding task. For surgeons, Kahol [180] studied the impact of fatigue in surgical residents, which used a demanding task and measurement by EEG using a B-Alert device while Guru [181] assessed cognitive performance during robot-assisted surgery by EEG using a B-Alert device. Other studies which used electrophysiological measures in conjunction with other methods are elaborated on in the objective measures section of mix methods.
Biologic Markers
Fatigue-related biologic markers were studied in the pathological context of chronic disease: plasma glucose, associated with variations in transient physical and mental energy, effort, and fatigue with variable degrees of success [182, 183]; cortisol, an indirect marker of fatigue through stress level and energy expenditure associated with fatigue [184]; salivary alpha-amylase (sAA) associated with surrogate markers of nervous system activity [185] and task engagement/disengagement [186], with variable degrees of success; and melatonin following circadian patterns and disrupted in individuals with chronic disease and recurrent fatigue [187], used for sleep-related fatigue. In elite athletes, creatine kinase (CK), C-reactive protein (CRP), uric acid, testosterone, salivary immunoglobulin (S-IgA) were used as indirect markers of fatigue in the recovery period following intense physical activity. Biologic systems involved in the regulation of motor activity are intricately linked with sleep, feeding behaviour, energy, and mood [188].
Behavioural Markers
Common behavioural markers utilized to assess fatigue include sleep and physical activity. These markers can be assessed by research-grade devices and consumer devices alike, with various degrees of validated accuracy, wear comfort, and presence in the research lab for the procedure. Figures 4.4 and 4.5 depict research and consumer wearable devices, respectively. As opposed to the momentary measures above, the behavioural markers can also be monitored continuously (with very high frequency, e.g., seconds or milliseconds) and longitudinally (for an extended duration, e.g., weeks to years) in time.
Sleep can be assessed using polysomnography and actigraphy. Polysomnography (PSG) [189] is an electrophysiological sleep study, which assesses brain waves (EEG), oxygen levels in the blood, heart rate (ECG), eye movements (EOG), and muscle and skeletal muscle activation and movements (EMG), breathing functions, respiratory airflow, respiratory effort, and pulse oximetry (SpO2). Polysomnography quantifies sleep duration, interruptions, stages (e.g., light, deep, rapid eye movement (REM)) and waking states (e.g., awake, asleep). Actigraphy [190] is a non-invasive electrophysiological method that assesses movement and is used to monitor humans at rest or during various types of physical activity. Examples of research-grade wearable actigraph devices are ActiWatchFootnote 1 and ActiGraph.Footnote 2 The actigraph can be worn on the wrist or ankle during daily life, for several weeks. The actigraph allows for the continuous collection of data due to its non-invasive nature, however, widespread and longitudinal use is limited by its specific purpose of researching physical activity with limited considerations to the user experience and price.
More recent consumer wearable monitors, in the form of wristbands, smartwatches, sleep mattresses, or finger rings from manufacturers such as Fitbit,Footnote 3 Oura,Footnote 4 and WithingsFootnote 5 [191] monitor sleep continuously by using a combination of movement, measured by a triaxial accelerometer, and HR/HRV, measured by photoplethysmography (PPG), non-invasive optical measurement of the volumetric variability of blood in the vessels under the skin. Consumer wearables can also measure behavioural markers pertaining to physical activity , e.g., duration, intensity (classified as, e.g., sedentary, low, moderate, and vigorous), type (using activity class recognition), effort (in metabolic equivalent of tasks (METs)), distance, elevation, step count, workouts, and other measures derived from the continuous multivariate data obtained from triaxial accelerometer and gyroscope sensors inside the device.
Studies assessing non-pathologic fatigue, sleep, and physical activity have been performed in segments of the general population and for several occupations, usually by combining subjective and objective measurements. In segments of the general population, Ellingson [17] studied the influence of active and sedentary behaviours on perceived energy and fatigue in women by using subjective POMS and SF-36 and objective physical activity by an accelerometer (Actigraph). For occupations, Rizzo [192] assessed the role of fatigue and sleepiness in drivers with obstructive sleep apnea by using subjective SF-36 and objective PSG. De Araújo Fernandes Jr. [193] quantified the impact of shift work on train drivers by using PVT and actigraphy (Actiwatch). Fernandes-Junior [193] assessed sleep, fatigue, and Quality of Life in night shift workers using subjective scale and actigraphy (Actiwatch). Towards the pathologic type of fatigue, Campbell [194] assessed fatigue and sleep in individuals having unexplained chronic fatigue by using subjective scales and objective PSG; Maher [195] quantified the relationships between fatigue, physical activity, and socio-demographic characteristics in children and adolescents with physical disabilities by using objective physical activity measurement using an accelerometer (Actigraph).
Numerous other studies have assessed pathologic fatigue in the context of a specific disease using PSG or actigraphy. Attarian [196], Kaynak [197], Veauthier [198], and Kaminska [199] studied relationships between sleep and fatigue in multiple sclerosis patients. Keefer (2006) and Shitrit [200] assessed sleep and fatigue in inflammatory bowel disease. Merikangas [188] used a combination of EMA and actigraphy to assess energy, mood, and activity in individuals with depressive disorders. Sun [201] assessed the relationships between daytime napping and fatigue and Quality of Life in cancer individuals by using subjective scale and objective sleep quality (Actigraph). Ancoli-Israel [202] assessed sleep, fatigue, and circadian activity in women with breast cancer by using subjective scale and objective circadian rhythms using actigraphy (Actiwatch). Holliday [203] assessed fatigue and sleep quality in prostate cancer patients by using a subjective scale of Quality of Life and actigraphy (Actiwatch). Cambras [204] studied circadian rhythm in patients of encephalomyelitis using actigraphy (ActTrust). Nicklas [205] assessed physical activity behaviours (using accelerometers) and fatigue (using SF-36) in adults of middle and old age with chronic inflammations. Nilsson [206] studied intensity levels of physical activity and fatigue in cancer patients by using an accelerometer (SenseWear). Vancampfort [207] studied the relationships between cardio-respiratory fitness and increased quality of life in people with bipolar disorder using, among others, the subjective SF-36 and an armband (SenseWear) for objective physical activity and sedentary behaviour measurement. Sheshadri [208] assessed the relationship between intensity levels of physical activity and fatigue in patients on dialysis by using step count from a pedometer (Accusplit).
More recent studies used wearables to assess wearable-measured sleep and physical activity in a pathologic context. Qazi [209] studied fatigue in patients with inflammatory bowel disease by using a Fitbit Charge HR. Sofia et al. [210] used the same wearable to associate sleep fragmentation with individuals having clinically active disease. Abbott [211] conducted an intervention study for physical activity in case of cancer-related fatigue patients by using activity trackers (undisclosed brand) without reporting measurements but reporting that the activity tracker was deemed helpful.
Mixed Methods
In our literature review, we identified numerous studies which combined two or more objective measures of fatigue. These studies focused on either cognitive or physical fatigue in the general population or specific occupations, or physical fatigue in specific segments of the population.
For non-pathologic cognitive fatigue in the general population, Zhang [174] estimated mental fatigue based on EEG (Neuroscan) and HRV from ECG while performing an arithmetic task using a personal computer, Ren [212] studied various degrees of mental fatigue by using multiple types of measurements: EEG, ECG as well as galvanic skin response (GSR), Smith [213] quantified the effects on cognitive tasks on mental fatigue indicators, using PVT and other two tasks and assessing fatigue through subjective VAS and objective HRV from EEG, and Brown [214] studied the effects of mental fatigue on exercise intentions and behaviour using cognitive and then physical exercises by using a cycle ergometer.
In the area of non-pathological physical fatigue, Kanitz [215] assessed the impact on eurythmy therapy on fatigue by using subjective MFI and objective HRV by ECG. For occupational fatigue, Smolders [216] studied the alertness during office hours induced by higher luminosity by using subjective measures, task performance (PVT, letter substitution test), and heart rate measures (ECG), Oriyama [217] studied fatigue in shift nurses by measuring objective HRV from ECG, and subjective EMA using VAS, and Singh [218] assessed the technical performance of surgeons when using robotic surgery where the task was a suture under time pressure, measured with a subjective surgical task scale and objective HR, and objective functional near-infrared spectroscopy (fNIRS).
In the area of pathological fatigue, Dishman [219] studied the effects of cycling exercise on fatigue among young adults who report persistent fatigue using incremental exercise test on an electronically braked, computer-driven cycle ergometer (Lode), and providing subjective POMS and objective HR (Polar), VO2-max and expired gas (Parvo Medics), and EEG (Electrical Geodesics).
Property Spectrums of Energy and Fatigue Measures
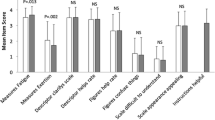
The findings from our literature review classify the energy and fatigue measurements by type (subjective and objective), location (clinician’s office, daily life, or both/mixed), source (self-, performance/capacity-, and technology-reported, using the taxonomy by Mayo [12]), and administration (scales, prompts, tasks, and devices). In Table 4.4, we place each such measurement on spectrums for the following properties:
-
1.
Validated: fatigue outcome reliability assessed by statistical analysis on the target population and scientific publication.
-
2.
Quantifiable: fatigue outcomes interval or ratio at a minute or higher precision.
-
3.
Frequent: often repeated administrations with one day or less between administrations.
-
4.
Continuous: fatigue proxy variable measured on a time series with a minute or higher granularity.
-
5.
Judgment-free: bias-free from the perception of judgment from the administrator; tasks and research devices allow some refraining.
-
6.
Mood-free: bias-free from the voluntary or involuntary perception of self.
-
7.
Memory-free: bias-free from the remembrance of the past; prompts allow for long-term memory loss.
-
8.
Owned: whether the participant owns the device; scales and prompts are marked as partial in case they are delivered to a device owned by the participant.
-
9.
Contextual: collected from settings daily life; research devices can be borrowed to the participant for a short time to wear in daily life context.
Discussion
Key Findings
Fatigue or lack of energy is a universal symptom experienced by those suffering from different medical and psychological illnesses as well as by healthy individuals in the general population. Overall, fatigue is a ubiquitous and multifaceted symptom that is challenging to define and measure. Fatigue may be classified as pathological or non-pathological, physical or mental, and can be measured subjectively or objectively.
Different approaches have been employed in order to measure energy and fatigue including scales, prompts, physical measures, cognitive measures, physiological markers, biological markers, behavioural markers, and mixed methods. Some measurement methods assess the effects of fatigue (e.g. performance decrements), some attempt to identify the source of fatigue (e.g. muscle dysfunction), while others adopt a behavioural perspective (e.g. decreased physical activity or prolonged sleep). Some methods focus on capacity while others assess performance. These varied methods each contain advantages and disadvantages in terms of traditional validation, access to continuous data, and ecological validity.
Subjective instruments instantiating self-reported outcomes [12] suffer from inherent shortcomings, in particular, they are infrequent and subjective. Furthermore, self-report by recall has an intrinsic problem: due to biases, such as mood states or sleepiness, individuals are not able to accurately recall past experience, particularly experiences that are frequent, mundane, and/or irregular [220]. In addition, the potential discrepancy between how one feels and how one thinks one should feel contributes to lack of ecological validity in self-reports of fatigue and requires further research [15]. Incorporating a real-time collection of fatigue data in naturalistic settings may reduce problems associated with retrospective recall of events, summarization of events, and artificial contexts or settings [118].
Objective measures obtained by tech-reported outcomes can be collected continuously from individuals in the context of daily life. To this end, both academia and industry are increasing their efforts to develop technological solutions, such as sensors which can measure, models which can assess, and artefacts which can manage energy and fatigue. Recent technological methods to monitor and manage energy and fatigue include sensors, smartphones and their applications, and research- and consumer-grade wearables. Technology-based monitoring of energy and fatigue could assist in the initial diagnosis and the early detection of diseases could enable one to monitor post-treatment evolution and could help assess the risk of certain medications on patients [3]. Furthermore, technology-based monitoring of energy and fatigue could assist healthy individuals in enhancing work performance, conserving and managing energy levels, and maintaining health.
Energy and fatigue are of great importance to diseased individuals. The connection between pathological fatigue and disease is well established in the literature. Fatigue frequently foreshadows conditions like multiple sclerosis [221], cancer [28], and HIV infection [222], among other diseases. Furthermore, fatigue, as well as increased energy, has been identified as a core symptom of mental health disorders including depressive disorders and bipolar disorders. Current literature on energy and fatigue is biased towards pathological, rather than healthy, populations. In addition, it is possible that the existence of healthy fatigue is a barrier to full comprehension of the impact of pathological fatigue, as pathological fatigue is more extreme and different. This highlights the importance of further research on both non pathological and pathological fatigue.
In addition to the comprehensive literature examining fatigue and disease, the monitoring of energy and fatigue has also been highlighted for specific vocational and occupational populations, such as professional athletes [24], police [25], and drivers [165]. The literature aims to gain an understanding of health, safety, occupational functioning, burnout, performance, and capacity. More efforts could be put toward studying healthy general populations, as in addition to affecting an individual’s quality of life, fatigue impacts the economy because of the connection to productivity and illness.
Insights into the classification and measurement of energy and fatigue may also be applied broadly to the general population as mobile monitoring technology allows the assessment of these homeostatic systems in real-time [188]. Quality of Life Technologies (QoLT) refers to technologies for assessment or improvement of the individual’s quality of life [223]. Optimal measurement of energy and fatigue would be moved out of the lab and into the real world, continuous rather than infrequent, and based on accurate, validated, yet minimally intrusive measures and devices. Future research could establish traditional validity for the continuous, daily life, measurement of energy and fatigue.
Assessing energy and fatigue could also contribute to the quantified self. The quantified self (QS) is any individual engaged in the self-tracking of any kind of biological, physical, behavioural, or environmental information. QS promotes a proactive stance toward obtaining information and acting on it [224]. One of the earliest recorded examples of quantified self-tracking is that of Sanctorius of Padua, who studied energy expenditure by tracking his food intake, weight, and elimination for 30 years in the sixteenth century [225]. State of the art energy and fatigue assessment could contribute meaningfully to the quantified self.
Limitations
A limitation of the current chapter stems from the pathological bias in the field. Namely, because the existing literature is biased toward pathological fatigue, we built the non-pathological (also referred to as physiological) classification system arm based on existing pathological models. This limitation is also related to our literature search strategy. Our method of reviewing the literature was based on a scoping review approach rather than a structured systematic review. We did not exclude studies based on methodologies used or populations studied.
Subjective measures discussed in this chapter contain limitations including being infrequent, involving recalls, and potential to be influenced by mood states, memory, and expectations. Wearable measurements also contain limitations related to the population that uses wearables. Specifically, device owners are more likely to be young individuals with disposable incomes who already lead healthy lifestyles and want to quantify their progress [226]. Future work should ensure that wearable data is representative and note this bias in current wearable data.
An additional limitation of the field is that there is not yet a validated calibration between objective measures and the concept of energy and fatigue. Therefore, much of our discussion is speculative. A major impediment in the understanding of fatigue and energy lies in the fact that for over 100 years, research has shown little relationship between self-report and actual, objective measurements of fatigue [167]. There are several definitions of energy and fatigue and these have not been conclusively associated with objective measures. This doesn’t invalidate subjective or objective measures of fatigue but rather indicates that they may be describing something that is more complicated and cannot be whittled down to a single biological measure. Therefore, both subjective experience and objective measurements are being considered in the context of energy and fatigue, as they are important indicators for health and quality of life. Future research could aim to bridge the gap between subjective and objective measures by accounting for multiple variables and conducting calibration studies.
Opportunities
Energy and fatigue is a Quality of Life facet in which the successful assessment, exclusively through Quality of Life Technologies [223], has promising likelihood. The mass adoption of miniaturized devices in daily life (with large scale and diversity in personal and contextual characteristics of the data), the availability of relevant predictors of energy and fatigue in large scale data, and the presence of platforms that facilitate participation in research at scale contribute to the feasibility of the operationalization of this facet.
Currently, research is progressing in assessing pathological and non-pathological energy and fatigue by using subjective, objective, and mixed methods. Miniaturized devices, such as smartphones and wearables, increasingly accurately monitor daily life behaviours (e.g., physical activity and sleep), sense signals (e.g., heart rate, momentary electrocardiogram, etc.) and administer prompts (e.g., validated scales, items, and tasks). As the line between consumer health wearables and medical devices continues to blur, it is possible for a single wearable device to monitor a range of medical risk factors [227]. Adoption of wearables is increasing; 21% of Americans own a wearable [228], there are more than 200 models of wearablesFootnote 6 and the market is expected to continue to increase by 2022 [229] towards available objective behavioural data at scale. Open health platforms are being employed to facilitate scalable participation and manage subjective, objective, and mixed data [230].
Co-calibrations of (1) subjective validated scales of energy and fatigue and (2) objective measures of daily life behaviours may rigorously validate objective measures of energy and fatigue and meet the aim of assessing energy and fatigue using QoLT. For example, a study aiming to co-calibrate subjective scales and objective behaviours for occupational fatigue may collect multiple behavioural markers passively and continuously (e.g., physical activity, sleep, heart rate) from tens to hundreds of drivers for several months to years, during driving and daily living, and regularly administering validated energy and fatigue scales such that their recall periods cover the duration. Such a study may observe trends of fatigue longitudinally in time. Within a smaller sample size, a purely statistical approach would allow for the assessment of validity (e.g., by correlating the corresponding subjective and objective measures) and reliability (e.g., by measuring the same person’s fatigue in similar days of week, months, or seasons) of the objective measure. Within a larger sample, a predictive approach would learn the subjective measures of energy and fatigue by using the objective measures of behaviours. These approaches can iteratively reduce the number of scale items. One step further, continuous behaviour monitoring during daily life facilitates the trigger of momentary assessments upon changes in objective behaviours that associate with changes in energy and fatigue. Such an approach may increase the accuracy of the co-calibration. Furthermore, alternative statistical or predictive risk scenarios can maintain energy (“if you continue working at this pace, you will likely not get tired”), prevent fatigue (“if you continue working at this pace, you will likely accumulate occupational fatigue in two weeks”), and compensate for the losses induced by fatigue (“consider taking a break of one week to restore your productivity from three months ago”).
Initially, co-calibrations may suffer from lower accuracy (e.g., revealing only basic trends and associations) or limited extent (e.g., applying for specific scale items, collecting limited objective behaviours, applying for limited energy and fatigue types) as the measured objective measures or available sample may not explain the energy and fatigue directly. In such cases, a directed graph of co-calibrations with additional Quality of Life facets (e.g., stress, health outcomes), using additional objective measures, may need to be constructed to represent the relationships accurately such that energy and fatigue are explained through a series of directed co-calibration paths originating exclusively from objective measures, essentially assessing energy and fatigue through QoLT exclusively.
A successful energy and fatigue assessment using QoLT would contribute to the “Internet of everything” 50-year vision of a digital future where “internet use will be nearly as pervasive and necessary as oxygen” [231]. Specifically, such an assessment would contribute to three of Stansberry’s five hopeful visions of 2069. The first vision, living longer and feeling better where “internet-enabled technology will help people live longer and healthier lives; scientific advances will continue to blur the line between human and machine” [231] will be enabled by quantifying the relationships between energy, fatigue, behaviours, health, and Quality of Life outcomes. The second vision, less work, more leisure where “artificial intelligence tools will take over repetitive, unsafe and physically taxing labour, leaving humans with more time for leisure” [231] will be enabled through (short-term) the transition to increasingly passive reported outcomes that reduce the burden of participation in research and (longer-term) statistical and predictive optimization of physical and mental effort allocation for the occupations where energy and fatigue are prevalent. The third vision, individualized experiences where “digital life will be tailored to each user” [230] will be enabled by interventions leveraging large scale data, accurate models, and alternative personalized scenarios addressing fatigue prevention, before management, and before compensation.
Conclusive Remarks
Energy and fatigue impact physical, cognitive, emotional, social, and occupational functioning and carry important implications for an individual’s health and overall Quality of Life. Lacking energy carries consequences for an individual’s routine functioning. Everyday activities, including work performance and self-care activities, can be impeded or even curtailed. Energy is required to sustain life and efficient spending of energy results in overall vitality. Paradoxically, one tends to think of energy of a resource that is depleted and then restored with rest, while at the same time, many observe that using energy generates additional energy. This curious paradox highlights the importance of future research and clarity. In addition, the classification of energy and fatigue is critical as it is possible that the existence of non pathological fatigue inhibits true appreciation of the impact of pathological fatigue.
The contributions of this chapter include a semi-structured literature review on energy and fatigue assessment and its potential within Quality of Life Technologies, a taxonomy of the field of energy and fatigue, and the identification of a research validation gap between subjective and objective measures of energy and fatigue. We foresee the necessity to conduct studies of increasing size in order to co-calibrate the subjective and objective measures towards the integration of exclusively objective measures in research and clinical practice.
The measurement of energy and fatigue has been complicated by difficulties in definition and assessment. We conclude that optimal classification and measurement of energy and fatigue would occur in the real world, continuously and in real-time, while being ecologically valid and informing the design of interventions aimed at maintaining energy and monitoring fatigue towards positive outcomes of health and Quality of Life.
References
“WHO | WHOQOL: Measuring quality of life,” WHO. https://www.who.int/healthinfo/survey/whoqol-qualityoflife/en/index4.html. Accessed Jun. 24, 2020.
Stahl SM. The psychopharmacology of energy and fatigue. J Clin Psychiatry. 2002, Jan;63(1):7–8. https://doi.org/10.4088/jcp.v63n0102.
Hernández N, Favela J. Assessing the perception of physical fatigue using Mobile sensing. In: Wister M, Pancardo P, Acosta F, Hernández JA, editors. Intelligent data sensing and processing for health and Well-being applications. Academic; 2018. p. 161–73.
Boksem MAS, Tops M. Mental fatigue: costs and benefits. Brain Res Rev. 2008, Nov;59(1):125–39. https://doi.org/10.1016/j.brainresrev.2008.07.001.
Marcora SM, Staiano W, Manning V. Mental fatigue impairs physical performance in humans. J Appl Physiol. 2009, Mar;106(3):857–64. https://doi.org/10.1152/japplphysiol.91324.2008.
Al-Mulla MR, Sepulveda F, Colley M. A review of non-invasive techniques to detect and predict localised muscle fatigue. Sensors. 2011;11(4):4. https://doi.org/10.3390/s110403545.
Finsterer J, Mahjoub SZ. Fatigue in healthy and diseased individuals. Am J Hosp Palliat Med. 2014, Aug;31(5):562–75. https://doi.org/10.1177/1049909113494748.
Kluger BM, Krupp LB, Enoka RM. Fatigue and fatigability in neurologic illnesses. Neurology. 2013, Jan;80(4):409–16. https://doi.org/10.1212/WNL.0b013e31827f07be.
Chaudhuri A, Behan PO. Fatigue in neurological disorders. Lancet. 2004;363(9413):978–88. https://doi.org/10.1016/S0140-6736(04)15794-2.
Mollayeva T, Kendzerska T, Mollayeva S, Shapiro CM, Colantonio A, Cassidy JD. A systematic review of fatigue in patients with traumatic brain injury: the course, predictors and consequences. Neurosci Biobehav Rev. 2014, Nov;47:684–716. https://doi.org/10.1016/j.neubiorev.2014.10.024.
Ream E, Richardson A. Fatigue: a concept analysis. Int J Nurs Stud. 1996, Oct;33(5):519–29. https://doi.org/10.1016/0020-7489(96)00004-1.
Mayo NE, Figueiredo S, Ahmed S, Bartlett SJ. Montreal accord on patient-reported outcomes (PROs) use series–paper 2: terminology proposed to measure what matters in health. J Clin Epidemiol. 2017, Sep;89:119–24. https://doi.org/10.1016/j.jclinepi.2017.04.013.
Dittner AJ, Wessely SC, Brown RG. The assessment of fatigue: a practical guide for clinicians and researchers. J Psychosom Res. 2004, Feb;56(2):157–70. https://doi.org/10.1016/S0022-3999(03)00371-4.
Whitehead L. The measurement of fatigue in chronic illness: a systematic review of unidimensional and multidimensional fatigue measures. J Pain Symptom Manag. 2009, Jan;37(1):107–28. https://doi.org/10.1016/j.jpainsymman.2007.08.019.
Aaronson LS, et al. Defining and measuring fatigue. Image J Nurs Sch. 1999;31(1):45–50. https://doi.org/10.1111/j.1547-5069.1999.tb00420.x.
Hornsby BWY, Naylor G, Bess FH. A taxonomy of fatigue concepts and their relation to hearing loss. Ear Hear. 2016;37(Suppl 1):136S–44S. https://doi.org/10.1097/AUD.0000000000000289.
Ellingson L, Ae K, Vack N, Cook D. Active and sedentary behaviors influence feelings of energy and fatigue in women. Med Sci Sports Exerc. 2014, Jan;46(1):192–200. https://doi.org/10.1249/mss.0b013e3182a036ab.
Abdel-Kader K, et al. Ecological momentary assessment of fatigue, sleepiness, and exhaustion in ESKD. BMC Nephrol. 2014, Feb;15(1):29. https://doi.org/10.1186/1471-2369-15-29.
Cochran A, Belman-Wells L, McInnis M. Engagement strategies for self-monitoring symptoms of bipolar disorder with Mobile and wearable technology: protocol for a randomized controlled trial. JMIR Res Protoc. 2018;7(5):e130. https://doi.org/10.2196/resprot.9899.
Curran SL, Beacham AO, Andrykowski MA. Ecological momentary assessment of fatigue following breast cancer treatment. J Behav Med. 2004, Oct;27(5):425–44. https://doi.org/10.1023/B:JOBM.0000047608.03692.0c.
Chieh TC, Mohd M, Mustafa AH, Hendi SF, Majlis BY. Development of vehicle driver drowsiness detection system using electrooculogram (EOG). In: 2005 1st International Conference on Computers, Communications, Signal Processing with Special Track on Biomedical Engineering; 2005, Nov. p. 165–8. https://doi.org/10.1109/CCSP.2005.4977181.
Diaz-Piedra C, Rieiro H, Suárez J, Rios-Tejada F, Catena A, Stasi LLD. Fatigue in the military: towards a fatigue detection test based on the saccadic velocity. Physiol Meas. 2016, Aug;37(9):N62–75. https://doi.org/10.1088/0967-3334/37/9/N62.
Dinges DF, Powell JW. Microcomputer analyses of performance on a portable, simple visual RT task during sustained operations. Behav Res Methods Instrum Comput. 1985, Nov;17(6):652–5. https://doi.org/10.3758/BF03200977.
Thorpe RT, Atkinson G, Drust B, Gregson W. Monitoring fatigue status in elite team-sport athletes: implications for practice. Int J Sports Physiol Perform. Apr, 2017;12(s2):S2-27–34. https://doi.org/10.1123/ijspp.2016-0434.
Vila, Bryan, “Tired cops: the importance of managing police fatigue,” Police Exec Res Forum, 2000.
Glaus A. Fatigue in patients with cancer: analysis and assessment. Springer Science & Business Media; 2012.
Jason LA, Evans M, Brown M, Porter N. What is fatigue? Pathological and nonpathological fatigue. PM&R. 2010, May;2(5):327–31. https://doi.org/10.1016/j.pmrj.2010.03.028.
Davis MP, Khoshknabi D, Yue GH. Management of fatigue in cancer patients. Curr Pain Headache Rep. 2006;10(4):260–9. https://doi.org/10.1007/s11916-006-0030-2.
Tanaka M, Watanabe Y. Supraspinal regulation of physical fatigue. Neurosci Biobehav Rev. 2012, Jan;36(1):727–34. https://doi.org/10.1016/j.neubiorev.2011.10.004.
Bogdanis GCP. Effects of physical activity and inactivity on muscle fatigue. Front Physiol. 2012;3 https://doi.org/10.3389/fphys.2012.00142.
Bloomfield SA. Changes in musculoskeletal structure and function with prolonged bed rest. Med Sci Sports Exerc. 1997;29(2):197–206.
Rimmer JH, Schiller W, Chen M-D. Effects of disability-associated low energy expenditure deconditioning syndrome. Exerc Sport Sci Rev. 2012, Jan;40(1):22–9. https://doi.org/10.1097/JES.0b013e31823b8b82.
Dantzer R, et al. Identification and treatment of symptoms associated with inflammation in medically ill patients. Psychoneuroendocrinology. 2008, Jan;33(1):18–29. https://doi.org/10.1016/j.psyneuen.2007.10.008.
Linnhoff S, Fiene M, Heinze H-J, Zaehle T. Cognitive fatigue in multiple sclerosis: An objective approach to diagnosis and treatment by transcranial electrical stimulation. Brain Sci. 2019, May;9(5):5. https://doi.org/10.3390/brainsci9050100.
Valentine AD, Meyers CA. Cognitive and mood disturbance as causes and symptoms of fatigue in cancer patients. Cancer. 2001;92(S6):1694–8. https://doi.org/10.1002/1097-0142(20010915)92:6+<1694::AID-CNCR1499>3.0.CO;2-S.
Kohl AD, Wylie GR, Genova HM, Hillary FG, DeLuca J. The neural correlates of cognitive fatigue in traumatic brain injury using functional MRI. Brain Inj. 2009, Jan;23(5):420–32. https://doi.org/10.1080/02699050902788519.
Byun E, Gay CL, Lee KA. Sleep, fatigue, and problems with cognitive function in adults living with HIV. J Assoc Nurses AIDS Care JANAC. 2016;27(1):5–16. https://doi.org/10.1016/j.jana.2015.10.002.
Wong WS, Fielding R. Prevalence of chronic fatigue among Chinese adults in Hong Kong: a population-based study. J Affect Disord. 2010, Dec;127(1):248–56. https://doi.org/10.1016/j.jad.2010.04.029.
Hockey B, Hockey R. The psychology of fatigue: work, effort and control. Cambridge University Press; 2013.
Light AR, White AT, Hughen RW, Light KC. Moderate exercise increases expression for sensory, adrenergic and immune genes in chronic fatigue syndrome patients, but not in normal subjects. J Pain Off J Am Pain Soc. 2009, Oct;10(10):1099–112. https://doi.org/10.1016/j.jpain.2009.06.003.
Schwartz JE, Jandorf L, Krupp LB. The measurement of fatigue: a new instrument. J Psychosom Res. 1993, Oct;37(7):753–62. https://doi.org/10.1016/0022-3999(93)90104-N.
Edwards RH. Human muscle function and fatigue. Ciba Found Symp. 1981;82:1–8.
Friedman JH, et al. Fatigue in Parkinson’s disease: a review. Mov Disord. 2007;22(3):297–308. https://doi.org/10.1002/mds.21240.
Cairns SP, Knicker AJ, Thompson MW, Sjøgaard G. Evaluation of models used to study neuromuscular fatigue. Exerc Sport Sci Rev. 2005, Jan;33(1):9–16.
Abd-Elfattah HM, Abdelazeim FH, Elshennawy S. Physical and cognitive consequences of fatigue: a review. J Adv Res. 2015, May;6(3):351–8. https://doi.org/10.1016/j.jare.2015.01.011.
Kamijo K, Nishihira Y, Higashiura T, Kuroiwa K. The interactive effect of exercise intensity and task difficulty on human cognitive processing. Int J Psychophysiol. 2007, Aug;65(2):114–21. https://doi.org/10.1016/j.ijpsycho.2007.04.001.
Tomporowski PD. Effects of acute bouts of exercise on cognition. Acta Psychol. 2003, Mar;112(3):297–324. https://doi.org/10.1016/S0001-6918(02)00134-8.
Cian C, Barraud PA, Melin B, Raphel C. Effects of fluid ingestion on cognitive function after heat stress or exercise-induced dehydration. Int J Psychophysiol. 2001, Nov;42(3):243–51. https://doi.org/10.1016/S0167-8760(01)00142-8.
Falup-Pecurariu C. Fatigue assessment of Parkinson’s disease patient in clinic: specific versus holistic. J Neural Transm. 2013, Apr;120(4):577–81. https://doi.org/10.1007/s00702-013-0969-1.
Persson J, Welsh KM, Jonides J, Reuter-Lorenz PA. Cognitive fatigue of executive processes: interaction between interference resolution tasks. Neuropsychologia. 2007, Apr;45(7):1571–9. https://doi.org/10.1016/j.neuropsychologia.2006.12.007.
van der Linden D, Eling P. Mental fatigue disturbs local processing more than global processing. Psychol Res. 2006, Sep;70(5):395–402. https://doi.org/10.1007/s00426-005-0228-7.
Lorist MM. Impact of top-down control during mental fatigue. Brain Res. 2008, Sep;1232:113–23. https://doi.org/10.1016/j.brainres.2008.07.053.
Cook DB, O’Connor PJ, Lange G, Steffener J. Functional neuroimaging correlates of mental fatigue induced by cognition among chronic fatigue syndrome patients and controls. NeuroImage. 2007,May;36(1):108–22. https://doi.org/10.1016/j.neuroimage.2007.02.033.
Lal SKL, Craig A. A critical review of the psychophysiology of driver fatigue. Biol Psychol. 2001,Feb;55(3):173–94. https://doi.org/10.1016/S0301-0511(00)00085-5.
Goode JH. Are pilots at risk of accidents due to fatigue? J Saf Res. 2003, Aug;34(3):309–13. https://doi.org/10.1016/S0022-4375(03)00033-1.
Van Cutsem J, Marcora S, De Pauw K, Bailey S, Meeusen R, Roelands B. The effects of mental fatigue on physical performance: a systematic review. Sports Med. 2017, Aug;47(8):1569–88. https://doi.org/10.1007/s40279-016-0672-0.
Grillon C, Quispe-Escudero D, Mathur A, Ernst M. Mental fatigue impairs emotion regulation. Emot Wash DC. 2015, Jun;15(3):383–9. https://doi.org/10.1037/emo0000058.
Chen MK. The epidemiology of self-perceived fatigue among adults. Prev Med. 1986, Jan;15(1):74–81. https://doi.org/10.1016/0091-7435(86)90037-X.
Hardy GE, Shapiro DA, Borrill CS. Fatigue in the workforce of national health service trusts: levels of symptomatology and links with minor psychiatric disorder, demographic, occupational and work role factors. J Psychosom Res. 1997, Jul;43(1):83–92. https://doi.org/10.1016/S0022-3999(97)00019-6.
Hickie IB, Hooker AW, Bennett BK, Hadzi-Pavlovic D, Wilson AJ, Lloyd AR. Fatigue in selected primary care settings: sociodemographic and psychiatric correlates. Med J Aust. 1996;164(10):585–8. https://doi.org/10.5694/j.1326-5377.1996.tb122199.x.
Loge JH, Ekeberg Ø, Kaasa S. Fatigue in the general norwegian population: normative data and associations. J Psychosom Res. 1998, Jul;45(1):53–65. https://doi.org/10.1016/S0022-3999(97)00291-2.
Pawlikowska T, Chalder T, Hirsch SR, Wallace P, Wright DJM, Wessely SC. Population based study of fatigue and psychological distress. BMJ. 1994, Mar;308(6931):763–6. https://doi.org/10.1136/bmj.308.6931.763.
David A, et al. Tired, weak, or in need of rest: fatigue among general practice attenders. BMJ. 1990, Nov;301(6762):1199–202.
Bultmann U, Kant I, Kasl SV. Fatigue and psychological distress in the working population psychometrics, prevalence, and correlates. U Bu. 2002:8.
Van Mens-Verhulst J, Bensing J. Distinguishing between chronic and nonchronic fatigue, the role of gender and age. Soc Sci Med. 1998, Sep;47(5):621–34. https://doi.org/10.1016/S0277-9536(98)00116-6.
Dement WC, Carskadon MA. Current perspectives on daytime sleepiness: the issues. Sleep. 1982, Sep;5(suppl_2):S56–66. https://doi.org/10.1093/sleep/5.S2.S56.
Shahid A, Shen J, Shapiro CM. Measurements of sleepiness and fatigue. J Psychosom Res. 2010, Jul;69(1):81–9. https://doi.org/10.1016/j.jpsychores.2010.04.001.
Dijk D, Czeisler C. Contribution of the circadian pacemaker and the sleep homeostat to sleep propensity, sleep structure, electroencephalographic slow waves, and sleep spindle activity in humans. J Neurosci. 1995, May;15(5):3526–38. https://doi.org/10.1523/JNEUROSCI.15-05-03526.1995.
Rey A. “L’examen clinique en psychologie.” 1958.
Michielsen HJ, De Vries J, Van Heck GL. Psychometric qualities of a brief self-rated fatigue measure: the fatigue assessment scale. J Psychosom Res. 2003, Apr;54(4):345–52. https://doi.org/10.1016/S0022-3999(02)00392-6.
Webster K, Odom L, Peterman A, Lent L, Cella D. The functional assessment of chronic illness therapy (FACIT) measurement system: validation of version 4 of the core questionnaire. Qual Life Res. 1999;
Fisk JD, Ritvo PG, Ross L, Haase DA, Marrie TJ, Schlech WF. Measuring the functional impact of fatigue: initial validation of the fatigue impact scale. Clin Infect Dis. 1994, Jan;18(Suppl_1):S79–83. https://doi.org/10.1093/clinids/18.Supplement_1.S79.
Chalder T, et al. Development of a fatigue scale. J Psychosom Res. 1993, Feb;37(2):147–53. https://doi.org/10.1016/0022-3999(93)90081-P.
Krupp LB, LaRocca NG, Muir-Nash J, Steinberg AD. The fatigue severity scale: application to patients with multiple sclerosis and systemic lupus erythematosus. Arch Neurol. 1989, Oct;46(10):1121–3. https://doi.org/10.1001/archneur.1989.00520460115022.
Tack BB. “Dimensions and correlates of fatigue in older adults with rheumatoid arthritis.,” Accessed: Jun. 24, 2020. [Online]. Available: https://elibrary.ru/item.asp?id=5833962.
Smets EMA, Garssen B, Bonke B, De Haes JCJM. The multidimensional fatigue inventory (MFI) psychometric qualities of an instrument to assess fatigue. J Psychosom Res. 1995, Apr;39(3):315–25. https://doi.org/10.1016/0022-3999(94)00125-O.
Ware JE Jr, Sherbourne CD. The MOS 36-item short-form health survey (SF-36): I. conceptual framework and item selection. Med Care. 1992:473–83.
Lai J-S, et al. How item banks and their application can influence measurement practice in rehabilitation medicine: a PROMIS fatigue item Bank example. Arch Phys Med Rehabil. 2011, Oct;92(10):S20–7. https://doi.org/10.1016/j.apmr.2010.08.033.
McNair D, Lorr M, Droppleman L. POMS manual for the profile of mood states. Educ Ind Test Serv. 1971;
Lee KA, Hicks G, Nino-Murcia G. Validity and reliability of a scale to assess fatigue. Psychiatry Res. 1991, Mar;36(3):291–8. https://doi.org/10.1016/0165-1781(91)90027-M.
Junghaenel DU, Christodoulou C, Lai J-S, Stone AA. Demographic correlates of fatigue in the US general population: results from the patient-reported outcomes measurement information system (PROMIS) initiative. J Psychosom Res. 2011, Sep;71(3):117–23. https://doi.org/10.1016/j.jpsychores.2011.04.007.
Alemohammad ZB, Sadeghniiat-Haghighi K. Risk of fatigue at work. In: Sharafkhaneh A, Hirshkowitz M, editors. Fatigue management: principles and practices for improving workplace safety. New York, NY: Springer; 2018. p. 181–91.
Sharafkhaneh A, Hirshkowitz M, editors. Fatigue management: principles and practices for improving workplace safety. New York, NY: Springer New York; 2018.
Xianglong S, Hu Z, Shumin F, Zhenning L. Bus drivers’ mood states and reaction abilities at high temperatures. Transp. Res. Part F Traffic Psychol. Behav. 2018, Nov;59:436–44. https://doi.org/10.1016/j.trf.2018.09.022.
Mitchell SA. Cancer-related fatigue: state of the science. PM&R. 2010, May;2(5):364–83. https://doi.org/10.1016/j.pmrj.2010.03.024.
Pearson EJM, Morris ME, di Stefano M, McKinstry CE. Interventions for cancer-related fatigue: a scoping review. Eur J Cancer Care (Engl). 2018, Jan;27(1):e12516. https://doi.org/10.1111/ecc.12516.
Cohen R, Bavishi C, Haider S, Thankachen J, Rozanski A. Meta-analysis of relation of vital exhaustion to cardiovascular disease events. Am J Cardiol. 2017, Apr;119(8):1211–6. https://doi.org/10.1016/j.amjcard.2017.01.009.
Nagy A, et al. Association of Exercise Capacity with physical functionality and various aspects of fatigue in patients with coronary artery disease. Behav Med. 2018, Jan;44(1):28–35. https://doi.org/10.1080/08964289.2016.1189395.
Lewko A, Bidgood P, Jewell A, Garrod R. A comprehensive literature review of COPD-related fatigue. Curr Respir Med Rev. 2012, Nov;8(5):370–82. https://doi.org/10.2174/157339812803832476.
Jensen Ø, Bernklev T, Jelsness-Jørgensen L-P. Fatigue in type 1 diabetes: a systematic review of observational studies. Diabetes Res Clin Pract. 2017, Jan;123:63–74. https://doi.org/10.1016/j.diabres.2016.11.002.
Vincent A, Benzo RP, Whipple MO, McAllister SJ, Erwin PJ, Saligan LN. Beyond pain in fibromyalgia: insights into the symptom of fatigue. Arthritis Res Ther. 2013, Nov;15(6):221. https://doi.org/10.1186/ar4395.
Czuber-Dochan W, Ream E, Norton C. Review article: description and management of fatigue in inflammatory bowel disease. Aliment Pharmacol Ther. 2013;37(5):505–16. https://doi.org/10.1111/apt.12205.
Han CJ, Yang GS. Fatigue in irritable bowel syndrome: a systematic review and meta-analysis of pooled frequency and severity of fatigue. Asian Nurs Res. 2016, Mar;10(1):1–10. https://doi.org/10.1016/j.anr.2016.01.003.
Nocerino A, Nguyen A, Agrawal M, Mone A, Lakhani K, Swaminath A. Fatigue in inflammatory bowel diseases: etiologies and management. Adv Ther. 2020, Jan;37(1):97–112. https://doi.org/10.1007/s12325-019-01151-w.
Moldovan I, et al. Pain and depression predict self-reported fatigue/energy in lupus. Lupus. 2013, Jun;22(7):684–9. https://doi.org/10.1177/0961203313486948.
Ghanean H, Ceniti AK, Kennedy SH. Fatigue in patients with major depressive disorder: prevalence, burden and pharmacological approaches to management. CNS Drugs. 2018, Jan;32(1):65–74. https://doi.org/10.1007/s40263-018-0490-z.
Charvet L, Serafin D, Krupp LB. Fatigue in multiple sclerosis. Fatigue Biomed Health Behav. 2014, Jan;2(1):3–13. https://doi.org/10.1080/21641846.2013.843812.
Latimer-Cheung AE, et al. Effects of exercise training on fitness, mobility, fatigue, and health-related quality of life among adults with multiple sclerosis: a systematic review to inform guideline development. Arch Phys Med Rehabil. 2013, Sep;94(9):1800–1828.e3. https://doi.org/10.1016/j.apmr.2013.04.020.
Newland P, Starkweather A, Sorenson M. Central fatigue in multiple sclerosis: a review of the literature. J Spinal Cord Med. 2016, Jul;39(4):386–99. https://doi.org/10.1080/10790268.2016.1168587.
Skoie IM, et al. Fatigue in psoriasis: a controlled study. Br J Dermatol. 2017;177(2):505–12.
Weinstein AA, et al. Effect of aerobic exercise training on fatigue and physical activity in patients with pulmonary arterial hypertension. Respir Med. 2013, May;107(5):778–84. https://doi.org/10.1016/j.rmed.2013.02.006.
Artom M, Moss-Morris R, Caskey F, Chilcot J. Fatigue in advanced kidney disease. Kidney Int. 2014, Sep;86(3):497–505. https://doi.org/10.1038/ki.2014.86.
Stebbings S, Treharne GJ. Fatigue in rheumatic disease: an overview. Int J Clin Rheumatol. 2010, Aug;5(4):487–502. https://doi.org/10.2217/ijr.10.30.
do Espírito Santo RC, et al. Neuromuscular fatigue is weakly associated with perception of fatigue and function in patients with rheumatoid arthritis. Rheumatol Int. 2018, Mar;38(3):415–23. https://doi.org/10.1007/s00296-017-3894-z.
Bailes S, et al. Fatigue: the forgotten symptom of sleep apnea. J Psychosom Res. 2011, Apr;70(4):346–54. https://doi.org/10.1016/j.jpsychores.2010.09.009.
Aarnes R, Stubberud J, Lerdal A. A literature review of factors associated with fatigue after stroke and a proposal for a framework for clinical utility. Neuropsychol Rehabil. 2019, Mar;0(0):1–28. https://doi.org/10.1080/09602011.2019.1589530.
Duncan F, Wu S, Mead GE. Frequency and natural history of fatigue after stroke: a systematic review of longitudinal studies. J Psychosom Res. 2012, Jul;73(1):18–27. https://doi.org/10.1016/j.jpsychores.2012.04.001.
Newland P, Oliver B, Newland JM, Thomas FP. Testing feasibility of a Mobile application to monitor fatigue in people with multiple sclerosis. J Neurosci Nurs. 2019, Dec;51(6):331–4. https://doi.org/10.1097/JNN.0000000000000479.
Maguire R, McCann L, Miller M, Kearney N. Nurse’s perceptions and experiences of using of a mobile-phone-based advanced symptom management system (ASyMS©) to monitor and manage chemotherapy-related toxicity. Eur J Oncol Nurs. 2008, Sep;12(4):380–6. https://doi.org/10.1016/j.ejon.2008.04.007.
Nicholas J, Larsen ME, Proudfoot J, Christensen H. Mobile apps for bipolar disorder: a systematic review of features and content quality. J Med Internet Res. 2015;17(8):e198. https://doi.org/10.2196/jmir.4581.
Shiffman S, Stone AA, Hufford MR. Ecological momentary assessment. Annu Rev Clin Psychol. 2008;4(1):1–32. https://doi.org/10.1146/annurev.clinpsy.3.022806.091415.
Larson R, Csikszentmihalyi M. The experience sampling method. In: Flow and the foundations of positive psychology. Dordrecht: Springer Netherlands; 2014. p. 21–34.
van Berkel N, Ferreira D, Kostakos V. The experience sampling method on Mobile devices. ACM Comput Surv. 2018, Jan;50(6):1–40. https://doi.org/10.1145/3123988.
Guérin E, Fortier MS, Williams T. ‘I just NEED to move…’: examining women’s passion for physical activity and its relationship with daily affect and vitality. Psychol Well- Theory Res Pract. 2013, Nov;3(1):4. https://doi.org/10.1186/2211-1522-3-4.
Zacher H, Brailsford HA, Parker SL. Micro-breaks matter: a diary study on the effects of energy management strategies on occupational Well-being. J Vocat Behav. 2014, Dec;85(3):287–97. https://doi.org/10.1016/j.jvb.2014.08.005.
Rhee H, Kim S. Effects of breaks on regaining vitality at work: An empirical comparison of ‘conventional’ and ‘smart phone’ breaks. Comput Hum Behav. 2016, Apr;57:160–7. https://doi.org/10.1016/j.chb.2015.11.056.
Murphy SL, Smith DM. Ecological measurement of fatigue and fatigability in older adults with osteoarthritis. J Gerontol Ser A. 2010, Feb;65A(2):184–9. https://doi.org/10.1093/gerona/glp137.
Hacker ED, Ferrans CE. Ecological momentary assessment of fatigue in patients receiving intensive cancer therapy. J Pain Symptom Manag. 2007, Mar;33(3):267–75. https://doi.org/10.1016/j.jpainsymman.2006.08.007.
Bower JE. Cancer-related fatigue: mechanisms, risk factors, and treatments. Nat Rev Clin Oncol. 2014, Oct;11(10):597–609. https://doi.org/10.1038/nrclinonc.2014.127.
van der Linden D, Frese M, Meijman TF. Mental fatigue and the control of cognitive processes: effects on perseveration and planning. Acta Psychol. 2003, May;113(1):45–65. https://doi.org/10.1016/S0001-6918(02)00150-6.
Ackerman PL. 100 years without resting. In: Cognitive fatigue: multidisciplinary perspectives on current research and future applications. Washington, DC, US: American Psychological Association; 2011. p. 11–43.
Lieberman HR. Cognitive methods for assessing mental energy. Nutr Neurosci. 2007, Oct;10(5–6):229–42. https://doi.org/10.1080/10284150701722273.
Basner M, Dinges DF. Maximizing sensitivity of the psychomotor vigilance test (PVT) to sleep loss. Sleep. 2011, May;34(5):581–91. https://doi.org/10.1093/sleep/34.5.581.
Holsbeeke L, Ketelaar M, Schoemaker MM, Gorter JW. Capacity, capability, and performance: different constructs or three of a kind? Arch Phys Med Rehabil. 2009, May;90(5):849–55. https://doi.org/10.1016/j.apmr.2008.11.015.
World Health Organization, “World report on ageing and health.,” World Health Organ., 2015.
Enright PL. The six-minute walk test. Respir Care. 2003;48(8):3.
Rudick R, et al. Recommendations from the national multiple sclerosis society clinical outcomes assessment task force. Ann Neurol. 1997;42(3):379–82. https://doi.org/10.1002/ana.410420318.
Podsiadlo D, Richardson S. The timed ‘up & go’: a test of basic functional mobility for frail elderly persons. J Am Geriatr Soc. 1991;39(2):142–8. https://doi.org/10.1111/j.1532-5415.1991.tb01616.x.
Boolani A, O’Connor PJ, Reid J, Ma S, Mondal S. Predictors of feelings of energy differ from predictors of fatigue. Fatigue Biomed. Health Behav. 2019, Jan;7(1):12–28. https://doi.org/10.1080/21641846.2018.1558733.
Roldán Jiménez C, Bennett P, Ortiz García A, Cuesta Vargas AI. Fatigue detection during sit-to-stand test based on surface electromyography and acceleration: a case study. Sensors. 2019, Jan;19(19):19. https://doi.org/10.3390/s19194202.
Muñoz JE, Gouveia ER, Cameirão MS, Badia SB. PhysioLab–a multivariate physiological computing toolbox for ECG, EMG and EDA signals: a case of study of cardiorespiratory fitness assessment in the elderly population. Multimed Tools Appl. 2018, May;77(9):11521–46. https://doi.org/10.1007/s11042-017-5069-z.
Nicklas BJ, et al. Effects of caloric restriction on cardiorespiratory fitness, fatigue, and disability responses to aerobic exercise in older adults with obesity: a randomized controlled trial. J Gerontol A Biol Sci Med Sci. 2019, Jun;74(7):1084–90. https://doi.org/10.1093/gerona/gly159.
Sehle A, Vieten M, Mündermann A, Dettmers C. Difference in motor fatigue between patients with stroke and patients with multiple sclerosis: a pilot study. Front Neurol. 2014;5 https://doi.org/10.3389/fneur.2014.00279.
Dedering Å, Gnospelius Å, Elfving B. Reliability of measurements of endurance time, electromyographic fatigue and recovery, and associations to activity limitations, in patients with lumbar disc herniation. Physiother Res Int. 2010;15(4):189–98. https://doi.org/10.1002/pri.457.
Schmitt J, Lindner N, Reuss-Borst M, Holmberg H-C, Sperlich B. A 3-week multimodal intervention involving high-intensity interval training in female cancer survivors: a randomized controlled trial. Physiol Rep. 2016;4(3):e12693. https://doi.org/10.14814/phy2.12693.
Folstein MF, Robins LN, Helzer JE. The mini-mental state examination. Arch Gen Psychiatry. 1983, Jul;40(7):812. https://doi.org/10.1001/archpsyc.1983.01790060110016.
U. S. Army, “Army individual test battery,” Man. Dir. Scoring, 1944.
Hannay HJ, Levin HS. Selective reminding test: An examination of the equivalence of four forms. J Clin Exp Neuropsychol. 1985, Jun;7(3):251–63. https://doi.org/10.1080/01688638508401258.
Barbizet J, Cany E. Clinical and psychometrical study of a patient with memory disturbances. Int J Neurol. 1967;7(1):44–54.
Rao SM, Hammeke TA, McQuillen MP, Khatri BO, Lloyd D. Memory disturbance in chronic progressive multiple sclerosis. Arch Neurol. 1984, Jun;41(6):625–31. https://doi.org/10.1001/archneur.1984.04210080033010.
A. Smith, Symbol digit modalities test. Western Psychological Services Los Angeles, 1973.
Gronwall DMA. Paced auditory serial-addition task: a measure of recovery from concussion. Percept Mot Skills. 1977, Apr;44(2):367–73. https://doi.org/10.2466/pms.1977.44.2.367.
Barr A, Brandt J. Word-list generation deficits in dementia. J Clin Exp Neuropsychol. 1996, Dec;18(6):810–22. https://doi.org/10.1080/01688639608408304.
Obrist PA, Webb RA, Sutterer JR. Heart rate and somatic changes during aversive conditioning and a simple reaction time task. Psychophysiology. 1969;5(6):696–723.
Bever CT Jr, Grattan L, Panitch HS, Johnson KP. The brief repeatable battery of neuropsychological tests for multiple sclerosis: a preliminary serial study. Mult Scler J. 1995;1(3):165–9.
Smolders KC, de Kort YA. Bright light and mental fatigue: effects on alertness, vitality, performance and physiological arousal. J Environ Psychol. 2014;39:77–91.
Westbrook JI, Raban MZ, Walter SR, Douglas H. Task errors by emergency physicians are associated with interruptions, multitasking, fatigue and working memory capacity: a prospective, direct observation study. BMJ Qual Saf. 2018;27(8):655–63.
Hartzler BM. Fatigue on the flight deck: the consequences of sleep loss and the benefits of napping. Accid Anal Prev. 2014;62:309–18.
Staniute M, Bunevicius A, Brozaitiene J, Bunevicius R. Relationship of health-related quality of life with fatigue and exercise capacity in patients with coronary artery disease. Eur J Cardiovasc Nurs. 2014, Aug;13(4):338–44. https://doi.org/10.1177/1474515113496942.
Pimenta A, Carneiro D, Novais P, Neves J. Monitoring mental fatigue through the analysis of keyboard and mouse interaction patterns. In: International Conference on Hybrid Artificial Intelligence Systems; 2013. p. 222–31.
Foti K, Xanthopoulou D, Papagiannidis S, Kafetsios K. The role of tweet-related emotion on the exhaustion–recovery from work relationship. In: Conference on e-Business, e-Services and e-Society; 2019. p. 380–91.
Dikmen S, Machamer J, Temkin N, McLean A. Neuropsychological recovery in patients with moderate to severe head injury: 2 year follow-up. J Clin Exp Neuropsychol. 1990;12(4):507–19.
Ponsford JL, Olver JH, Curran C. A profile of outcome: 2 years after traumatic brain injury. Brain Inj. 1995;9(1):1–10.
Van Zomeren AH, Van den Burg W. Residual complaints of patients two years after severe head injury. J Neurol Neurosurg Psychiatry. 1985;48(1):21–8.
Price E, Moore G, Galway L, Linden M. Towards a mobile assistive technology for monitoring and assessing cognitive fatigue in individuals with acquired brain injury. In: 2015 IEEE International Conference on Computer and Information Technology; Ubiquitous Computing and Communications; Dependable, Autonomic and Secure Computing; Pervasive Intelligence and Computing; 2015. p. 1487–91.
Tran Y, Wijesuriya N, Tarvainen M, Karjalainen P, Craig A. The relationship between spectral changes in heart rate variability and fatigue. J Psychophysiol. 2009;23(3):143–51.
Segerstrom SC, Nes LS. Heart rate variability reflects self-regulatory strength, effort, and fatigue. Psychol Sci. 2007;18(3):275–81.
Blausen.com staff. Medical gallery of Blausen medical 2014. WikiJournal of Medicine. 2014;1(2)
Samel A, Wegmann H-M, Vejvoda M. Aircrew fatigue in long-haul operations. Accid Anal Prev. 1997;29(4):439–52.
Goldman LI, McDonough MT, Rosemond GP. Stresses affecting surgical performance and learning: I. correlation of heart rate, electrocardiogram, and operation simultaneously recorded on videotapes. J Surg Res. 1972;12(2):83–6.
Chen C, Li K, Wu Q, Wang H, Qian Z, Sudlow G. EEG-based detection and evaluation of fatigue caused by watching 3DTV. Displays. 2013;34(2):81–8.
Holdsworth L, Evens T. Is heart rate variability a useful marker of stress and fatigue in emergency and pre-hospital clinicians?–a systematic review. Resuscitation. 2017;118:e95.
Stamler JS, Goldman ME, Gomes J, Matza D, Horowitz SF. The effect of stress and fatigue on cardiac rhythm in medical interns. J Electrocardiol. 1992;25(4):333–8.
Heemskerk J, et al. Relax, it’s just laparoscopy! A prospective randomized trial on heart rate variability of the surgeon in robot-assisted versus conventional laparoscopic cholecystectomy. Dig Surg. 2014;31(3):225–32.
Jung S-J, Shin H-S, Chung W-Y. Driver fatigue and drowsiness monitoring system with embedded electrocardiogram sensor on steering wheel. IET Intell Transp Syst. 2014;8(1):43–50.
Díaz-Toral LG, Banderas-Dorantes TR, Rivas-Vilchis JF. Impact of electroacupuncture treatment on quality of life and heart rate variability in fibromyalgia patients. J Evid-Based Complement Altern Med. 2017;22(2):216–22.
DeLuca J. “19 Fatigue: its definition, its study, and its future,” Fatigue Window Brain, p. 319, 2005.
Stern JA, Boyer D, Schroeder D. Blink rate: a possible measure of fatigue. Hum Factors. 1994;36(2):285–97.
Sirois S, Brisson J. Pupillometry. Wiley Interdiscip Rev Cogn Sci. 2014;5(6):679–92.
Eggert T, et al. The pupillographic sleepiness test in adults: effect of age, gender, and time of day on pupillometric variables. Am J Hum Biol. 2012;24(6):820–8.
Lowenstein O, Feinberg R, Loewenfeld IE. Pupillary movements during acute and chronic fatigue: a new test for the objective evaluation of tiredness. Invest Ophthalmol Vis Sci. 1963;2(2):138–57.
Hirvonen K, Puttonen S, Gould K, Korpela J, Koefoed VF, Müller K. Improving the saccade peak velocity measurement for detecting fatigue. J Neurosci Methods. 2010;187(2):199–206.
You C-W, et al. CarSafe: a driver safety app that detects dangerous driving behavior using dual-cameras on smartphones. In: Proceedings of the 2012 ACM Conference on Ubiquitous Computing; 2012. p. 671–2.
Zhang Y-F, Gao X-Y, Zhu J-Y, Zheng W-L, Lu B-L. A novel approach to driving fatigue detection using forehead EOG. In: 2015 7th International IEEE/EMBS Conference on Neural Engineering (NER); 2015. p. 707–10.
Morris G, Maes M. Myalgic encephalomyelitis/chronic fatigue syndrome and encephalomyelitis disseminata/multiple sclerosis show remarkable levels of similarity in phenomenology and neuroimmune characteristics. BMC Med. 2013;11(1):1–23.
Lorist MM, Bezdan E, ten Caat M, Span MM, Roerdink JB, Maurits NM. The influence of mental fatigue and motivation on neural network dynamics; an EEG coherence study. Brain Res. 2009;1270:95–106.
Sheng Y, Huang K, Zou J, Wang L, Wei P. Exploring the relationship between neural mechanism and detection in mental fatigue by genetic algorithm and hierarchical clustering. In: 2019 IEEE 7th International Conference on Bioinformatics and Computational Biology (ICBCB); 2019. p. 120–4.
Craig A, Tran Y, Wijesuriya N, Nguyen H. Regional brain wave activity changes associated with fatigue. Psychophysiology. 2012;49(4):574–82.
Zhao C, Zheng C, Zhao M, Tu Y, Liu J. Multivariate autoregressive models and kernel learning algorithms for classifying driving mental fatigue based on electroencephalographic. Expert Syst Appl. 2011;38(3):1859–65.
Kahol K, Smith M, Brandenberger J, Ashby A, Ferrara JJ. Impact of fatigue on neurophysiologic measures of surgical residents. J Am Coll Surg. 2011;213(1):29–34.
Guru KA, Shafiei SB, Khan A, Hussein AA, Sharif M, Esfahani ET. Understanding cognitive performance during robot-assisted surgery. Urology. 2015;86(4):751–7.
Gold AE, MacLeod KM, Deary IJ, Frier BM. Hypoglycemia-induced cognitive dysfunction in diabetes mellitus: effect of hypoglycemia unawareness. Physiol Behav. 1995;58(3):501–11.
Newsholme EA, Blomstrand E, Ekblom B. Physical and mental fatigue: metabolic mechanisms and importance of plasma amino acids. Br Med Bull. 1992;48(3):477–95.
Olsson EM, Roth WT, Melin L. Psychophysiological characteristics of women suffering from stress-related fatigue. Stress Health J Int Soc Investig Stress. 2010;26(2):113–26.
Kuebler U, et al. Norepinephrine infusion with and without alpha-adrenergic blockade by phentolamine increases salivary alpha amylase in healthy men. Psychoneuroendocrinology. 2014;49:290–8.
Hopstaken JF, van der Linden D, Bakker AB, Kompier MA. The window of my eyes: task disengagement and mental fatigue covary with pupil dynamics. Biol Psychol. 2015;110:100–6.
Van Heukelom RO, Prins JB, Smits MG, Bleijenberg G. Influence of melatonin on fatigue severity in patients with chronic fatigue syndrome and late melatonin secretion. Eur J Neurol. 2006;13(1):55–60.
Merikangas KR, et al. Real-time mobile monitoring of the dynamic associations among motor activity, energy, mood, and sleep in adults with bipolar disorder. JAMA Psychiatry. 2019;76(2):190–8.
Bloch KE. Polysomnography: a systematic review. Technol Health Care. 1997;5(4):285–305.
Sadeh A, Hauri PJ, Kripke DF, Lavie P. The role of actigraphy in the evaluation of sleep disorders. Sleep. 1995;18(4):288–302.
Wac K. From quantified self to quality of life. In: Digital health. Springer; 2018. p. 83–108.
Rizzo D, et al. The role of fatigue and sleepiness in drivers with obstructive sleep apnea. Transp Res Part F Traffic Psychol Behav. 2019;62:796–804.
Fernandes-Junior SA, Ruiz FS, Antonietti LS, Tufik S, Túlio de Mello M. Sleep, fatigue and quality of life: a comparative analysis among night shift workers with and without children. PLoS One. 2016;11(7):e0158580.
Campbell R, Tobback E, Delesie L, Vogelaers D, Mariman A, Vansteenkiste M. Basic psychological need experiences, fatigue, and sleep in individuals with unexplained chronic fatigue. Stress Health. 2017;33(5):645–55.
Maher C, et al. Fatigue is a major issue for children and adolescents with physical disabilities. Dev Med Child Neurol. 2015;57(8):742–7.
Attarian HP, Brown KM, Duntley SP, Carter JD, Cross AH. The relationship of sleep disturbances and fatigue in multiple sclerosis. Arch Neurol. 2004, Apr;61(4):525–8. https://doi.org/10.1001/archneur.61.4.525.
Kaynak H, et al. Fatigue and sleep disturbance in multiple sclerosis. Eur J Neurol. 2006;13(12):1333–9.
Veauthier C, et al. Fatigue in multiple sclerosis is closely related to sleep disorders: a polysomnographic cross-sectional study. Mult Scler J. 2011;17(5):613–22.
Kaminska M, et al. Obstructive sleep apnea is associated with fatigue in multiple sclerosis. Mult Scler J. 2012;18(8):1159–69.
Shitrit AB-G, et al. Sleep disturbances can be prospectively observed in patients with an inactive inflammatory bowel disease. Dig Dis Sci. 2018;63(11):2992–7.
Sun J-L, Lin C-C. Relationships among daytime napping and fatigue, sleep quality, and quality of life in cancer patients. Cancer Nurs. 2016;39(5):383–92.
Ancoli-Israel S, et al. Sleep, fatigue, depression, and circadian activity rhythms in women with breast cancer before and after treatment: a 1-year longitudinal study. Support Care Cancer. 2014, Sep;22(9):2535–45. https://doi.org/10.1007/s00520-014-2204-5.
Holliday EB, Dieckmann NF, McDonald TL, Hung AY, Thomas CR Jr, Wood LJ. Relationship between fatigue, sleep quality and inflammatory cytokines during external beam radiation therapy for prostate cancer: a prospective study. Radiother Oncol. 2016;118(1):105–11.
Cambras T, Castro-Marrero J, Zaragoza MC, Díez-Noguera A, Alegre J. Circadian rhythm abnormalities and autonomic dysfunction in patients with chronic fatigue syndrome/Myalgic encephalomyelitis. PLoS One. 2018;13(6):e0198106.
Nicklas BJ, Beavers DP, Mihalko SL, Miller GD, Loeser RF, Messier SP. Relationship of objectively-measured habitual physical activity to chronic inflammation and fatigue in middle-aged and older adults. J Gerontol Ser Biomed Sci Med Sci. 2016;71(11):1437–43.
Nilsson M, Arving C, Thormodsen I, Assmus J, Berntsen S, Nordin K. Moderate-to-vigorous intensity physical activity is associated with modified fatigue during and after cancer treatment. Support Care Cancer. 2019:1–8.
Vancampfort D, et al. Higher cardio-respiratory fitness is associated with increased mental and physical quality of life in people with bipolar disorder: a controlled pilot study. Psychiatry Res. 2017;256:219–24.
Sheshadri A, Kittiskulnam P, Johansen KL. Higher physical activity is associated with less fatigue and insomnia among patients on hemodialysis. Kidney Int Rep. 2019;4(2):285–92.
Qazi T, Farraye FA. Sleep and inflammatory bowel disease: an important bi-directional relationship. Inflamm Bowel Dis. 2019;25(5):843–52.
Sofia MA, Andersen M, Rubin DT. Sleep dysfunction and inflammatory bowel disease. In: Sleep effect on gastrointestinal health and disease: translational opportunities for promoting health and optimizing disease management. Nova Science Publishers, Inc; 2018. p. 177–99.
Abbott L. Energy through motion\copyright: An activity intervention for cancer-related fatigue in an ambulatory infusion center. Clin J Oncol Nurs. 2017;21(5):618.
Ren D, An Y, Li Z. The discriminative model of mental fatigue based on comprehensive parameter analysis. In: 2019 Prognostics and System Health Management Conference (PHM-Qingdao); 2019. p. 1–6.
Smith MR, Chai R, Nguyen HT, Marcora SM, Coutts AJ. Comparing the effects of three cognitive tasks on indicators of mental fatigue. J Psychol. 2019;153(8):759–83.
Brown DM, Bray SR. Effects of mental fatigue on exercise intentions and behavior. Ann Behav Med. 2019;53(5):405–14.
Kanitz JL, et al. The impact of eurythmy therapy on fatigue in healthy adults–a controlled trial. Eur J Integr Med. 2012;4(3):e289–97.
Smolders KC, De Kort YA, Cluitmans PJM. A higher illuminance induces alertness even during office hours: findings on subjective measures, task performance and heart rate measures. Physiol Behav. 2012;107(1):7–16.
Oriyama S, Miyakoshi Y, Kobayashi T. Effects of two 15-min naps on the subjective sleepiness, fatigue and heart rate variability of night shift nurses. Ind Health. 2013;
Singh H, et al. Robotic surgery improves technical performance and enhances prefrontal activation during high temporal demand. Ann Biomed Eng. 2018;46(10):1621–36.
Dishman RK, Thom NJ, Puetz TW, O’Connor PJ, Clementz BA. Effects of cycling exercise on vigor, fatigue, and electroencephalographic activity among young adults who report persistent fatigue. Psychophysiology. 2010;47(6):1066–74.
Zeng Z, Pantic M, Roisman GI, Huang TS. A survey of affect recognition methods: audio, visual, and spontaneous expressions. IEEE Trans Pattern Anal Mach Intell. 2008;31(1):39–58.
Braley TJ, Chervin RD. Fatigue in multiple sclerosis: mechanisms, evaluation, and treatment. Sleep. 2010;33(8):1061–7.
Adinolfi A. Assessment and treatment of HIV-related fatigue. J Assoc Nurses AIDS Care. 2001, Sep;12:29–34. https://doi.org/10.1016/S1055-3290(06)60155-6.
Wac K. Quality of life technologies. NY USA: Encycl. Behav. Med. Springer N. Y; 2020.
Swan M. The quantified self: fundamental disruption in big data science and biological discovery. Big Data. 2013;1(2):85–99.
Neuringer A. Self-experimentation: a call for change. Behaviorism. 1981;9(1):79–94.
Jones S. “Health & Fitness Wearables,” 2014. https://www.juniperresearch.com/researchstore/devices-technology/digital-health-wearables-research-report. Accessed Jun. 19, 2020.
Piwek L, Ellis DA, Andrews S, Joinson A. The rise of consumer health wearables: promises and barriers. PLoS Med. 2016;13(2):e1001953.
Vogels EA. About one-in-five Americans use a smart watch or fitness tracker. Wash. DC Pew Res. Cent; 2019.
Ubrani J, Llamas R, Shirer M. “IDC forecasts sustained double-digit growth for wearable devices led by steady adoption of smart-watches,” International Data Corporation, 2020. https://www.idc.com/getdoc.jsp?containerId=p. Accessed Jun. 15, 2020.
Estrada-Galiñanes V, Wac K. “Collecting, exploring and sharing personal data: why, how and where,” Data Sci., no. Preprint, pp. 1–28.
Stansberry K, Anderson J, Rainie L. Experts optimistic about the next 50 years of digital life. Pew Research Center: Internet, Science & Tech; 2019. https://www.pewresearch.org/internet/2019/10/28/experts-optimistic-about-the-next-50-years-of-digital-life/ (accessed Jun. 25, 2020)
Author information
Authors and Affiliations
Editor information
Editors and Affiliations
Rights and permissions
Open Access This chapter is licensed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license and indicate if changes were made.
The images or other third party material in this chapter are included in the chapter's Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the chapter's Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder.
Copyright information
© 2022 The Author(s)
About this chapter
Cite this chapter
Solomon, N.L., Manea, V. (2022). Quantifying Energy and Fatigue: Classification and Assessment of Energy and Fatigue Using Subjective, Objective, and Mixed Methods towards Health and Quality of Life. In: Wac, K., Wulfovich, S. (eds) Quantifying Quality of Life. Health Informatics. Springer, Cham. https://doi.org/10.1007/978-3-030-94212-0_4
Download citation
DOI: https://doi.org/10.1007/978-3-030-94212-0_4
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-94211-3
Online ISBN: 978-3-030-94212-0
eBook Packages: MedicineMedicine (R0)