Abstract
Given the serious adverse effects of hypothermia in term and preterm infants, thermal protection is of paramount importance in neonatal care. To compare potential benefits of wIRA radiators with conventional radiant warmers in neonatology, physical investigations (agar phantoms) and clinical observations (term and preterm neonates) were performed. Physical investigations revealed a fundamental difference in the mode of action between the two types of radiation: Whereas with conventional radiant warmers, the increase in core temperature (phantoms) is preceded by marked elevations in surface temperature, wIRA leads to more direct rises in core temperature and results in smaller amounts of evaporative water loss from the surface. Clinical observations reveal that wIRA causes less skin surface warming than conventional heat irradiation at equal power densities (irradiances). wIRA used as a supplementary source of heat during primary care in the delivery room was found to exert a preventive effect against unintentional heat loss during the subsequent incubator transport of preterm neonates to the intensive care unit. Overall, due to its specific physical properties (“enhanced depth effect with less surface overheating”), wIRA seems to be particularly suited to replace the extra heat losses occurring in preterm or otherwise compromised neonates without undue risk of superficial burns.
You have full access to this open access chapter, Download chapter PDF
Similar content being viewed by others
Keywords
1 Risk of Hypothermia in Term and Preterm Neonates
Human neonates are at heightened risk of hypothermia. However, contrary to what is often believed, their propensity to cool down is not, or not merely, due to an “immaturity” of thermoregulation. In fact, at least term neonates are well adapted to their small body size by their comparatively high specific (i.e., weight-related) metabolic rate and by the ability to produce extra heat in their brown adipose tissue. Nevertheless, as a result of their relatively large surface-to-volume ratio and the steeply increasing heat loss with decreasing ambient temperatures, their maximal thermogenic capabilities are already attained at temperatures which are still deemed to be comfortable by adults. Moreover, the “invisibility” of non-shivering thermogenesis often leads to an underestimation of the thermal stress experienced by neonates with subsequent neglect of thermal care. The risk of hypothermia is even more pronounced in preterm neonates due to their smaller body size in conjunction with a true “immaturity” of the thermoregulatory effector systems (lack of both white and brown adipose tissue, slow increase in basal metabolic rate up to a level appropriate for body size, elevated permeability of skin resulting in higher evaporative water and heat losses) [1,2,3,4].
The adverse effects of cold are primarily caused by the combination of diminished peripheral perfusion (to decrease heat loss) and elevated metabolic rate (to increase heat production). The imbalance of oxygen supply and demand results in a metabolic acidosis that triggers pulmonary vasoconstriction and leads to a “vicious cycle” of hypoxia. The indirect effects of counter-regulation are potentiated by the direct effects of cold, especially by the impairment of blood coagulation which contributes to the increased risk of brain hemorrhage in hypothermic preterm neonates. Altogether, unintentional (accidental) hypothermia is known to increase morbidity and mortality in term and even more so in preterm neonates [1, 5, 6]. This contrasts with therapeutic (induced) hypothermia which has long been used in cardiac surgery to prevent brain damage during extracorporeal circulation and has now been established as a neuroprotective treatment for posthypoxic states in both adults (cardiac arrest) and neonates (perinatal asphyxia) [7, 8]. However, the undisputable beneficial effects of a cold-induced reduction in metabolic rate are only attained if thermoregulation is pharmacologically suppressed and are thus completely different from the potentially life-threatening sequelae of accidental hypothermia to be prevented by appropriate thermal care.
1.1 Methods of Thermal Care in Neonatology
To avoid unintentional cooling in term and preterm babies, extensive precautions to prevent and, where inevitable, replace heat losses are mandatory in clinical neonatology. In delivery rooms and on neonatal wards, thermal care is basically provided by either radiant warmers or incubators [2, 3, 9, 10]. In the latter, thermal protection comes from circulating warm air (heat convection) and, even more importantly, from high saturations of water vapor to reduce evaporation from the newborn’s body surface. In radiant warmers, heat is supplied/replaced by infrared irradiation. Since radiant heat elicits evaporation on the body surface, part of its warming effect is instantaneously counteracted by heat losses so that, when directly compared, heat radiators are slightly less effective in supplying heat than humidified incubators. If, however, evaporation is inhibited (e.g., by plastic sheets used to cover the babies), radiant warmers and incubators are equivalent in their thermo-protective effects [10, 11].
Despite their heating power, radiant warmers are often insufficient to compensate for the huge heat losses occurring in extremely low birthweight neonates during delivery room care. This could theoretically be counteracted by a corresponding increase in radiant power density (irradiance). However, conventional radiant warmers have one major drawback which limits their practical use: The low-energy, long-wave infrared (IR-B and IR-C) radiation they emit has a relatively low depth of penetration. The accumulation of heat within the outer skin layers not only causes some thermal discomfort in the caregivers, but also leads to a dependency of the newborn’s heat uptake on its peripheral circulation [4, 12, 13]. If skin perfusion were to be greatly reduced (e.g., under conditions of circulatory shock), or if the irradiance were to be further increased, a local overheating would inevitably result. In fact, severe cases of burns have been observed after resuscitation of asphyctic neonates under conventional IR radiators [14].
1.2 Aim of the Studies Reported
In view of the aforementioned limitations of conventional radiant warmers, the technology of water-filtered heat radiators [12], which emit a modified IR-A spectrum and should combine an enhanced depth effect with less surface overheating, has attracted some interest in neonatal care [13]. Several studies which have tested the potential benefits of water-filtered IR-A (wIRA) irradiation in neonates will be summarized in this contribution. Briefly, these studies can be subdivided into physical investigations, conducted to elucidate the particular mode of action of wIRA in comparison with conventional IR irradiation in agar phantoms, and clinical observations that have been performed to test the efficacy and safety of either type of heat radiators in human term and preterm neonates under common hospital conditions.
2 Materials and Methods
2.1 Physical Investigations
Most of the physical investigations were carried out on agar phantoms like those used in radiotherapy [12, 13, 15, 16]. Since these are mainly composed of water and allow direct evaporation from the surface, they have thermal properties somewhat similar to human tissues, and, more specifically, to preterm neonates. The phantoms were exposed to either conventional radiant warmers from different suppliers (DR = Dräger, H&L = Heinen & Löwenstein; F&P = Fisher & Paykel) or to the water-filtered infrared-A (wIRA) radiator manufactured by Hydrosun. The radiation power density (irradiance) was uniformly adjusted to 30 mW/cm2 and the duration of irradiation amounted to 60 min. Temperature measurements were performed using customary temperature probes placed within the core and on the surface of the phantoms. Alternatively, surface temperatures were assessed by infrared thermometry. In addition to the phantom studies, a number of thermographic measurements were carried out on the skin of healthy adult volunteers.
2.2 Clinical Observations
Clinical observations were performed on term and preterm neonates who were exposed to conventional IR or to wIRA irradiation as an alternative or supplementary source of heat. They were all in typical clinical settings in which an extra heat loss could be anticipated (primary care in the delivery room, incubator care in the intensive care unit, physical examinations on the neonatal ward). Body core and/or surface temperatures were alternatively measured by customary rectal thermometers, single spot infrared thermometers, or infrared thermography (Nikon LAIRD-S270). Since the latter often yields rather qualitative results, extra effort was undertaken to quantify the thermographic records. To this end, a grid of measuring points was laid over the body. By calculating the arithmetic means of closely adjacent measuring points, a total of four regional temperatures (of head, trunk, arm, and leg) was obtained which were then weighted according to the relative contribution of the respective regions to the total body surface area. In this way, a mean body surface temperature was determined (Fig. 13.1).
Thermographic observations comparing the effects of water-filtered IR-A (wIRA) and conventional IR irradiation on human neonates during routine examinations. To quantify the results, a grid of measuring points was laid over the thermographic pictures. Regional temperatures (e.g., head temperature) were calculated as arithmetic means of several measuring points. The mean body surface temperature was determined as the weighted mean of regional temperatures (according to the contribution of the respective regions to the total body surface area)
3 Results and Discussion
3.1 Physical Investigations
The physical measurements on agar phantoms revealed a surprisingly clear difference in the effects of wIRA in comparison with conventional IR irradiation: Whereas with conventional radiators, the surface temperatures at the end of the 60-min irradiation period clearly exceeded the core temperatures, the wIRA radiator resulted not only in an improved central warming, but also in a markedly diminished superficial overheating with the surface temperature being even lower than the core temperature (Fig. 13.2). The central warming effect was uniformly augmented when plastic sheets were used to attenuate evaporation. However, whereas under conventional IR radiators this related to an excessive increase in surface temperatures, the surface temperature in the wIRA-exposed phantoms did not reach higher levels than under conventional irradiation without plastic sheets (Fig. 13.3). From the time course of the heating process, it became evident that the central warming is preceded by a superficial accumulation of heat in conventional IR irradiation, with the heat transfer occurring by “secondary” conduction (in living beings, also by convection) from the surface to the core (Fig. 13.4). In contrast, the heat seems to be primarily deposited in deeper “tissue” layers under wIRA irradiation, with the warming of the surface being due to a back-diffusion of heat rather than to a direct local effect. Therefore, a comparatively low gradient between the (higher) core and the lower (surface) temperature is established (Fig. 13.5). In both cases, a leveling of the surface temperature increase can be observed which indicates a new equilibrium between radiative heat uptake and evaporative heat loss, and thus disappears when evaporation is prevented by plastic sheets.
Surface and core temperatures of agar phantoms after 60-min exposure to different types of IR irradiation (30 mW/cm2, means of n = 3, each): Whereas conventional radiant warmers (Dräger [DR], Heinen & Löwenstein [H&L], or Fisher & Paykel [F&P]) all lead to a much higher increase in surface than core temperatures, the wIRA radiator (Hydrosun [HY]) results in a predominant, and more pronounced increase in body core temperature with markedly reduced surface warming
Effects of plastic sheets on surface (a) and core (b) warming under different types of IR irradiation (60 min, 30 mW/cm2, mean of n = 3, each): With the use of a plastic sheet, the increase in core temperature is more pronounced with all types of irradiation. However, whereas this is associated with an excessive increase in surface temperature for conventional radiators (DR, H&L, F&P), the surface temperature for wIRA irradiation (HY) is not higher than for conventional IR irradiation without a plastic sheet
Heat transfer under conventional IR irradiation: The graphs represent the time course of core and surface temperature during a 60-min exposure to conventional IR irradiation without or with the use of plastic sheets. It is obvious that under conventional IR irradiation, a primary increase in surface temperature TS (a) precedes the secondary increase in core temperature TC (b), with the heat transfer occurring by conduction. With the use of a plastic sheet, not only is the increase in surface temperature much steeper, but also the final leveling off of the surface temperature is missing (c), probably due to the lacking cooling effect of evaporative water loss
Heat transfer under wIRA irradiation: The graphs represent the time course of core and surface temperature during a 60-min exposure to wIRA irradiation without or with the use of plastic sheets. In contrast to conventional IR irradiation (see Fig. 13.4), the increase in core temperature precedes superficial warming, which thus appears to be due to the back-diffusion of heat from deeper “tissue” layers. Using of a plastic sheet results in a largely homogeneous warming of outer and inner parts of the phantom
Incidentally, in parallel to the weaker surface heating effect, the induction of evaporation was also seen to be less pronounced in wIRA irradiation. This was found in complementary studies on either agar phantoms or pieces of meat which both exhibited an approx. 20–30% smaller loss of water at equal duration of wIRA exposure compared to conventional IR irradiation.
To further complement the physical investigations, a number of thermographic measurements were carried out in adult volunteers exposed to a 20-min irradiation with conventional “baby warmers” in comparison with the wIRA radiator. Remarkably, with the conventional radiant warmers, an almost painful elevation of skin temperature by approx. 5 °C was attained at the end of the observation period, whereas the skin temperature only rose by approx. 2.5 °C with the wIRA radiator (at equal irradiances).
3.2 Clinical Observations
Clinical observations were focused on the changes in body surface temperature or on the maintenance of core temperature in term and preterm neonates subjected to either type of IR irradiation.
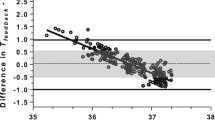
With regard to the body surface temperature, a thermographic study was performed on neonates who underwent routine examinations at a room temperature of 25 °C (i.e., without extra heat sources), under a conventional radiant heater (Weyer Ceramotherm 2000) or with the aid of a wIRA radiator (Hydrosun). At “pure” room temperature, a marked decrease in the mean body surface temperature occurred, reflecting the peripheral vasoconstriction of thermoregulating newborns. This could be prevented using radiant warmers, with the mean body surface temperature being slightly, but significantly higher in the conventional than in the wIRA group (Fig. 13.6). Although this result was biased by a slightly longer duration of examinations in the conventional IR than in the wIRA group, the study has once more demonstrated that the two types of IR irradiation differ in their surface effects. Incidentally, it has also shown that the calculation of a mean body surface temperature using a mathematical weighting algorithm is a valuable method for quantifying thermographic records.
Mean body surface temperature changes in term neonates subjected to routine clinical examinations without (room temperature, 25 °C) or with either conventional (Weyer) or wIRA radiators (Hydrosun; 15 mW/cm2 in both cases). At room temperature, a marked decrease in the mean surface temperature is to be observed as an effect of peripheral vasoconstriction. This is prevented by heat radiators, with the mean body surface temperature for conventional IR irradiation being slightly but significantly higher than for wIRA irradiation
With respect to body core temperatures, it was found that the use of two additional wIRA radiators as supplementary sources of heat did not alter the rectal temperature at the end of delivery room care, but still resulted in a smaller decrease in body temperature during the subsequent transport to the neonatal intensive care unit (Fig. 13.7). This implies that the heat deposits built up by wIRA irradiation in the depth of tissues exert a preventive effect against cooling, whereas the warming effect of conventional radiant warmers terminates as soon as the newborns are removed from the heat source.
Effective rectal temperature in preterm neonates after primary care in the delivery room (a), as compared with the temperature drop occurring during the subsequent incubator transport to the neonatal intensive care unit (b): Whereas the use of two wIRA radiators (in addition to the conventional radiant heater) did not lead to a measurable increase in rectal temperature at the end of delivery room care, the drop in temperature during the transport was significantly lower than after conventional IR irradiation alone. Apparently, the heat deposits built-up by wIRA irradiation in deeper tissue layers exert a preventive effect in terms of less subsequent cooling
In addition to these results, it has been shown that wIRA irradiation exhibits a lower absorption and better transmission rate through incubator walls so that the risk of heat-induced material damage is lower, and the thermoprotective effect of wIRA radiators used as a “back-up” to incubator care is superior to that obtained with conventional infrared “lamps” (Hanau Sollux 750) [13].
4 Current Practice and Unresolved Issues
Based on these and other results, wIRA radiators have been introduced on many neonatal wards over the past few years where they are currently used as a supplementary source of heat for use during procedures which bear a risk of cooling (primary care in the delivery room, intensive care procedures with opened incubator doors). The possibility of supplying extra heat without an increased risk of superficial burns has greatly promoted the acceptance of this novel technology.
In contrast to the short-term use of wIRA radiators, their long-term use in neonatal care (as a continuous source of heat) has, however, so far been limited by two issues:
First, concerns have been raised that near-infrared irradiation might cause retinal damage due to its ability to penetrate the posterior chamber of the eye [17, 18]. However, no IR-related injury to the newborn eye has ever been reported [19], and computational models show that even when using a wIRA radiator at short distances, the respective irradiations would remain below critical limits [20]. Furthermore, animal studies on the use of wIRA irradiation as an adjunctive treatment for chlamydial eye infections found no evidence of retinal damage [21, 22], whereas conversely, near-infrared exposure has been shown to reverse age-related visual impairment [23, 24]. Thus, although further studies are needed on the potential impact of IR irradiation on the developing eye [25], there is currently no evidence of any adverse wIRA effects that would outweigh the risk of superficial burns induced by conventional radiant warmers.
Second, the cylindrical shape of currently used wIRA radiators results in a defined beam which differs from the rectangular irradiation area of ceramic or steel tube heaters designed to be mounted over diaper changing tables. Here, further research is necessary to examine whether the natural filtering effect of water might not be imitated by artificial materials, thus enabling a flatter design of radiant warmers without loss of the specific wIRA properties.
5 Summary and Conclusions
In summary, a series of physical investigations on agar phantoms and adult volunteers, as well as several clinical observations on term and preterm babies, have shown that wIRA irradiation has surprisingly different thermal effects as compared to conventional radiant warmers used in neonatal care. Due to its specific physical properties, resulting in an “enhanced depth effect with less surface overheating,” it is especially suited as a supplementary source of heat under conditions where extra heat losses need to be replaced without an increased risk of burns. Provided some minor technical and biomedical issues are satisfactorily addressed, wIRA irradiation appears to have further potential for the thermal care of term and preterm neonates.
References
Gekle M, Singer D. Wärmehaushalt und Temperaturregulation. In: Pape H-C, Kurtz A, Silbernagl S, editors. Physiologie. Stuttgart: Thieme; 2019. p. 570–87.
Okken A, Koch J, editors. Thermoregulation of sick and low birth weight neonates: temperature control, temperature monitoring, thermal environment. Berlin: Springer; 1995.
Agren J. The thermal environment of the intensive care nursery. In: Martin RJ, Fanaroff AA, Walsh MC, editors. Fanaroff & Martin’s neonatal-perinatal medicine: diseases of the fetus and infant. 10th ed. Philadelphia: Elsevier Saunders; 2015. p. 502–12.
Singer D, van der Meer F, Perez A. What is the right temperature for a neonate? In: Herting E, Kiess W, editors. Innovations and frontiers in neonatology. Basel: Karger; 2020. p. 95–111.
Wilson E, Maier RF, Norman M, Effective Perinatal Intensive Care in Europe [EPICE] Research Group, et al. Admission hypothermia in very preterm infants and neonatal mortality and morbidity. J Pediatr. 2016;175:61–7.
Laptook AR, Bell EF, Shankaran S, NICHD (Neonatal Research Network), et al. Admission temperature and associated mortality and morbidity among moderately and extremely preterm infants. J Pediatr. 2018;192:53–59.e2.
Jacobs SE, Berg M, Hunt R, et al. Cooling for newborns with hypoxic ischaemic encephalopathy. Cochrane Database Syst Rev. 2013;2013(1):CD003311.
Wassink G, Davidson JO, Dhillon SK, et al. Therapeutic hypothermia in neonatal hypoxic-ischemic encephalopathy. Curr Neurol Neurosci Rep. 2019;19(2):2.
Flenady VJ, Woodgate PG. Radiant warmers versus incubators for regulating body temperature in newborn infants. Cochrane Database Syst Rev. 2003;4:CD000435.
McCall EM, Alderdice F, Halliday HL, et al. Interventions to prevent hypothermia at birth in preterm and/or low birth weight infants. Cochrane Database Syst Rev. 2018;2(2):CD004210.
Li S, Guo P, Zou Q, et al. Efficacy and safety of plastic wrap for prevention of hypothermia after birth and during NICU in preterm infants: a systematic review and meta-analysis. PLoS One. 2016;11(6):e0156960.
Vaupel P, Krüger W, editors. Wärmetherapie mit wassergefilterter Infrarot-A-Strahlung, Grundlagen und Anwendungsmöglichkeiten. 2nd ed. Stuttgart: Hippokrates; 1995.
Singer D, Schröder M, Harms K. Vorteile der wassergefilterten gegenüber herkömmlicher Infrarot-Strahlung in der Neonatologie. Z Geburtsh Neonatol. 2000;204:85–92.
Simonsen K, Graem N, Rothman LP, Degn H. Iatrogenic radiant heat burns in severely asphyxic newborns. Acta Paediatr. 1995;84:1438–40.
Ishida T, Kato H. Muscle equivalent agar phantom for 13.56 MHz RF-induced hyperthermia. Shimane. J Med Sci. 1980;4:134–40.
Visser AG, Deurloo IKK, Levendag PC, et al. An interstitial hyperthermia system at 27 MHz. Int J Hyperthermia. 1989;5:265–76.
Okuno T. Thermal effect of visible light and infra-red radiation (i.r.-A, i.r.-B and i.r.-C) on the eye: a study of infra-red cataract based on a model. Ann Occup Hyg. 1994;38:351–9.
International Electrotechnical Commission. International standard. Medical electrical equipment—part 2–21: particular requirements for the basic safety and essential performance of infant radiant warmers (IEC 60601–2-21). 3rd ed. Geneva: IEC; 2020.
Baumgart S, Knauth A, Casey FX, Quinn GE. Infrared eye injury not due to radiant warmer use in premature neonates. Am J Dis Child. 1993;147:565–9.
Piazena H. Ergebnisbericht zur Risikoanalyse gemäß DIN EN 62471 bei Anwendung eines Bestrahlungsgerätes zur lR-Hauttherapie des Typs hydrosun 750 mit BTE 595. Berlin: Persönl. Mittlg; 2017.
Rahn C, Marti H, Frohns A, et al. Water-filtered infrared A reduces chlamydial infectivity in vitro without causing ex vivo eye damage in pig and mouse models. J Photochem Photobiol B. 2016;165:340–50.
Kuratli J, Pesch T, Marti H, et al. Water filtered infrared A and visible light (wIRA/VIS) irradiation reduces Chlamydia trachomatis infectivity independent of targeted cytokine inhibition. Front Microbiol. 2018;9:2757.
Nelidova D, Morikawa RK, Cowan CS, et al. Restoring light sensitivity using tunable near-infrared sensors. Science. 2020;368(6495):1108–13.
Shinhmar H, Grewal M, Sivaprasad S, et al. Optically improved mitochondrial function redeems aged human visual decline. J Gerontol A Biol Sci Med Sci. 2020;75:e49–52.
Söderberg PG. Optical radiation and the eyes with special emphasis on children. Prog Biophys Mol Biol. 2011;107:389–92.
Acknowledgments
The majority of the results presented in this chapter were obtained by Meike Schröder (Dr. med. Thesis, Göttingen 2000), Christina Aumann (Dr. med. Thesis, Göttingen 2001), Verena Löwe (Dr. med. Thesis, Würzburg 2009), and Ulrike Benninghoff, Dr. med. (Würzburg), within the context of their doctoral or postdoctoral work, respectively. Many thanks to all the undergraduate and graduate collaborators and to the nursing staff of the involved neonatal wards and intensive care units for their enthusiasm and efforts. The expert technical assistance of Ms. B. Hallmann, Göttingen, and Ms. E. Maurer, Würzburg, in the physical investigations and part of the clinical observations is gratefully acknowledged. This project had been initiated and funded by a grant from the Dr. med. h.c. Erwin Braun Stiftung, Basel, Switzerland.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Open Access This chapter is licensed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license and indicate if changes were made.
The images or other third party material in this chapter are included in the chapter's Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the chapter's Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder.
Copyright information
© 2022 The Author(s)
About this chapter
Cite this chapter
Singer, D. (2022). Mode of Action, Efficacy, and Safety of Radiant Warmers in Neonatology. In: Vaupel, P. (eds) Water-filtered Infrared A (wIRA) Irradiation. Springer, Cham. https://doi.org/10.1007/978-3-030-92880-3_13
Download citation
DOI: https://doi.org/10.1007/978-3-030-92880-3_13
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-92879-7
Online ISBN: 978-3-030-92880-3
eBook Packages: MedicineMedicine (R0)