Abstract
In most quality improvement (QI) experiences, QI teams work in a single facility or community. This case describes the experience of a multifacility QI team in the Republic of Georgia that sought to improve the diagnosis and treatment of respiratory tract infections, the most frequent reason for seeking medical care among children. The QI team for Samtredia District drew members from the ambulatory clinic and Pediatrics Department of the district hospital as well as individual doctors’ practices that were all part of the same private medical service delivery network, Geo Hospitals. Geo Hospitals management also participated in QI team meetings to help address gaps in availability of essential inputs such as diagnostic tests and evidence-based medications. The case study details the design and implementation of the improvement effort and provides details about the capacity building and coaching support provided to the team that helped lead to improved health outcomes.
You have full access to this open access chapter, Download chapter PDF
Similar content being viewed by others
Keywords
- Coaching
- Compliance with clinical standards
- Cost savings
- Evidence-based treatment
- Georgia
- Rational use of antibiotics
- Respiratory tract infections
Background
Respiratory tract infections (RTIs) are the most frequent reasons for seeking medical care at the ambulatory as well as at the hospital level in the Republic of Georgia. In 2012, RTIs accounted for 36% of pediatric hospital admissions and 45% of ambulatory visits for children (NCDC&PH 2013).
According to the World Health Organization (WHO), RTIs, particularly pneumonia, remain one of the leading causes of under-five child mortality globally. Diagnosing and curing RTIs do not require advanced technologies. Yet, despite effective interventions to treat these infections, provision of appropriate care remains very low, particularly for appropriate medication prescription practices, including antibiotics (WHO and UNICEF 2013).
In Georgia , RTIs are the most common clinical condition for which children seek medical care. In 2012, approximately 46% of all outpatient pediatric (patients ages 0–15 years) clinical encounters were diagnosed with RTIs; pneumonia accounted for 7% of all pediatric hospitalizations. Due to the high burden of RTIs among children in the country, addressing the quality of diagnosis and treatment of RTIs became a priority focus area in Georgia. While many health-care quality improvement (QI) interventions have been successfully implemented in resource-limited settings, the evidence of their effect on improving RTI care and particularly rational prescription practices remains scarce. In addition, there is limited information about how these QI interventions have been planned, tested, implemented, and sustained in low- and middle-income countries, including Georgia.
To support the Government of Georgia’s strategic direction on improving the quality of medical services for priority clinical conditions, including RTIs in children, in February 2012, a United States Agency for International Development (USAID)-funded technical assistance project with decades of expertise in QI began to address challenges related to quality, consistency, and continuity of pediatric respiratory infections in the country.
To improve the quality of RTI diagnostic and treatment practices, the project, in close consultation with the Ministry of Labour, Health and Social Affairs (MoLHSA), selected the Imereti Region and a sample of its 82 facilities and 212 village doctor practices to implement improvement activities. The focus of the QI activities was to improve the quality of care of the highest disease burdens in the country, including cardiovascular disease, chronic obstructive pulmonary disease, and diagnosis and management of RTIs and asthma. Sites were chosen based on the political feasibility and representation of all levels of the health service delivery system to address continuity and timeliness of care. In addition, the project supported the formation of several QI teams in the region (i.e., teams of health workers from those facilities and doctor practices) who worked to improve health provider performance related to these clinical conditions. This was done by reviewing current client data, conducting problem analyses, developing and testing ideas to change their current processes, and measuring data to determine if their changes were leading to improvement.
Designing the Improvement Effort
Background on Georgia’s Health System
In recent years, Georgia’s health system has transitioned from a highly centralized Soviet Semashko model toward privatization of health service delivery infrastructure and liberalization of regulations. Consequently, health services are now predominantly provided by the private sector, including medical care corporations, stand-alone outpatient clinics, hospitals, and village solo practitioners.
Inherited from the Soviet system, the number of physicians in Georgia is the highest in the European region (4.8 per 1000 population in 2012), yet the utilization of outpatient and inpatient services is the lowest (NCDC&PH 2013). While coverage and reimbursement of health services by the Government of Georgia have changed several times in recent years, the state does not generally cover outpatient medications, the cost of which is the largest share of total health expenditures. Despite the Government’s coverage of selected outpatient and hospital services, implemented through various state health programs, out-of-pocket payments contributed to 70% of total health expenditures in 2012 (Chanturidze et al. 2009). The lack of affordability of medications and of access to quality medical care for high-burden clinical conditions thus posed significant challenges to patients and society in Georgia.
Site Selection and Formation of the QI Team
During the design stage of the project, medical facilities in the Imereti Region were undergoing changes in ownership and operations. Most of the facilities were owned by two of the largest private medical service delivery networks in the country (My Family Clinics and Geo Hospitals) and were financed on a per capita reimbursement system. Given this structure, the project deliberately selected medical facilities in these two networks to implement improvement activities. It was expected that when their central management saw the benefits of quality improvement in project-supported sites owned by these corporations, they would scale up successful QI practices to other facilities in their networks.
The QI team in Samtredia District included representatives from all levels of care under the management of Geo Hospitals, which was managing the State Program on Village Doctors and was the implementer of the main publicly funded health programs in the district. The QI team comprised two pediatricians from a Geo Hospitals ambulatory clinic, one pediatrician from a 35-bed district hospital in the Geo Hospitals network, and seven doctors from village clinics that were functionally and programmatically linked to Geo Hospitals. Due to a shortage of nurses and their limited role in providing clinical care in Georgia, nurses were not included in the improvement team. The composition of the QI team was deliberate in order to: (1) strengthen referral and counter-referral linkages between the different levels of care at the district level; and (2) fit into the objectives of Geo Hospitals to improve communication and care coordination between village doctors and their newly established ambulatory clinic and hospital within the district. Involvement in QI activities as part of the multifacility improvement team was a welcome opportunity for village doctors since they had limited information on recent changes in implementation of the State Program on Village Doctors and the organization of health service delivery within the district. In addition, strengthening the quality of the medical care for the most frequent reasons for children’s ambulatory visits, particularly in the villages, responded to the needs of Geo Hospitals to reduce medical care costs by managing the risk of overutilization of their primary care and specialty outpatient services.
Choosing Improvement Priorities
At the start of the QI intervention in June 2012, unpublished data from the National Center for Disease Control and Public Health (NCDC&PH) and the WHO suggested that in contrast to many other developing countries where lack of access to the health-care services is a core problem in the delivery of high-quality RTI care, in Georgia the main issue was the overutilization of diagnostic tests, specialist services, and medications, particularly antibiotics. The latter led to unjustified out-of-pocket expenses and adverse health and economic outcomes for families and society.
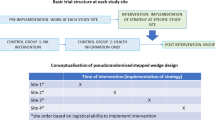
Before the improvement work began in Samtredia, a baseline assessment was carried out by the project implementing organization from April to August 2012 to identify critical quality gaps in the diagnosis and management of RTIs and other priority clinical areas. The assessment was part of a larger unpublished study conducted by the project in 9 hospitals, 10 ambulatory clinics, and 26 village primary care practices to assess the cost-effectiveness of QI interventions. The study included intervention and control facilities and gathered information on existing gaps in care processes and supporting system functions from review of patients’ medical charts, an observation checklist to assess key inputs/inventory, and interviews with care providers, managers, and patients/parents. Results from the medical record review revealed irrational and non-evidence-based use of medications during ambulatory management of RTIs and hospital management of pneumonia in children. At the ambulatory care level, a child with an acute RTI received, on average, 3.4 (95% confidence interval, 3.17–3.65) medications, with 2.6 (95% confidence interval, 2.37–2.75) of them irrelevant to his or her clinical condition and without any medical justification (i.e., non-evidence-based). Similarly, at the hospital level, a child received, on average, 7.5 (95% confidence interval, 7.14–7.87) medications, with 5.46 (95% confidence interval, 5.13–5.80) of them irrelevant to his or her clinical condition and not compliant with up-to-date scientific evidence. As shown in Fig. 2.1, non-evidence-based medications (including cough medications, probiotics, vitamins, antihistamines, and intravenous steroids) were prescribed to almost all children presenting with RTIs. Some non-evidence-based medications (e.g., vitamins) are associated with mild patient safety risk while others (e.g., intravenous steroids) are associated with high risk of adverse events and call for immediate action.
Use of non-evidence-based (Non-EB) medications in children diagnosed with pneumonia or RTIs at discharge and at last ambulatory visits (October 2010 to March 2012). Percent of medical charts with specific groups of non-evidence-based medications. (Source: Ambulatory (n = 212) and hospital (n = 274) medical charts)
The baseline assessment helped the Samtredia QI team, as well as the other project-supported QI teams delivering care for pediatric patients, to develop and refine their improvement aims.
Carrying Out the Improvement Intervention
The quality improvement intervention started with the project team and facility managers visiting each intervention facility and identifying members for the QI teams in the Imereti Region, including the Samtredia QI team presented in this case. After identifying all QI teams in the region, in March 2012 the project organized a 2-day learning session for all the QI teams in Imereti Region, with the participation of local, regional, and national key stakeholders. The purpose of the learning session was to introduce QI concepts and methods as well as ways to plan, implement, monitor, and refine changes in their health-care processes. The emphasis on health systems rather than individuals was new and unexpected for the members of the QI teams as they were used to top-down supervision that seeks to find bad performers and individuals to blame. In addition to QI methodologies, learning session participants received up-to-date information on evidence-based best practices for the management of RTIs in ambulatory and hospital settings. Participants were assisted in developing improvement aims, objectives, changes, and measurement criteria by working through a clinical case study. The sections below outline how the QI teams worked to choose their improvement priorities, how they set their aims and measures for improvement, and the changes they tested to improve the quality of diagnosis and management of RTIs.
Problem Analysis
The project provided clinical support for the Samtredia QI team’s RTI diagnosis and management improvement work through an external technical expert in RTI – the head of the Georgian Respiratory Association, who was also a professor of the Tbilisi State Medical University Pediatric Department and Clinical Director of the largest children’s referral hospital in Tbilisi.
The project supported the team with biweekly coaching visits from the technical expert, which included technical assistance on problem solving and clinical capacity building. The creation of one multifacility improvement team in Samtredia allowed the project team to achieve cost savings by avoiding separate coaching visits to each facility and instead providing coaching in one location to the multifacility improvement team. This allowed the project to increase the frequency of the coaching, which in turn proved to be a precondition for successful and sustainable improvement.
During the QI team meetings (lasting on average 2–4 hours), village doctors and pediatricians from the ambulatory clinic and the Samtredia District hospital selected medical charts to identify gaps in diagnosis and management of RTIs at individual doctors’ practices, as well as coordination of care at different levels. In addition to randomly selecting medical charts with standard RTI diagnoses, members of the QI team also brought for discussion, rare cases of RTIs among children from their clinical practice. They discussed possible interventions/changes in their local health-care processes to close the gaps and improve care. The coaching visits were usually conducted on the weekends (due to unavailability of other free time). The value of the visits was so high for individual provider teams that none of the providers objected to sacrificing their personal time to work on improvement activities without any remuneration for participation from the project or health facilities (e.g., overtime, per diem, or travel costs). Geo Hospitals management was also invited and regularly participated in QI team meetings. Their involvement was instrumental to address gaps in availability of essential key inputs (e.g., diagnostic tests, equipment, and other medical commodities) at medical facilities.
The first coaching visit in June 2012 included a brief overview of QI methodology as well as a clinical lecture on best practices in pediatric pneumonia management. As part of the coaching visit, the project’s technical expert presented a typical medical chart of a child in Georgia diagnosed with pneumonia, for whom 11 medications were prescribed. After careful analysis of each prescribed medication, the team agreed that only one medication was necessary. After presenting this typical case, the expert presented the results of the baseline assessment of RTI management that clearly showed the scope of the problem of overprescribing medications. This was followed by a discussion on the impact of such excessive use of medications on antibiotic resistance, patient safety, and costs associated with medical treatment. Team members realized that excessive use of antibiotics and other medications to treat pediatric RTIs was part of their routine practice. They wanted to change this practice but felt unsure and ill equipped to do so.
To help team members use systems thinking, the project helped QI teams use improvement tools such as a problem tree, fishbone (cause-and-effect) diagram, and driver diagrams, to help delineate the root causes of the problem related to irrational use of medications and systematize them according to the six WHO health system building blocks (WHO 2012). Despite being inexperienced and having very limited exposure to QI concepts and methodologies, the providers enthusiastically started identifying the root causes of the irrational prescription practices. Specifically, they identified these four root causes:
-
Poor knowledge of evidence-based guidelines and inadequate skills to manage acute pediatric respiratory tract infections
-
Inadequate ability to locate and evaluate current scientific evidence and apply it to their clinical practice
-
Limited availability of evidence-based medications in the hospitals, in a recommended dosage and form (e.g., amoxicillin)
-
Parental misconceptions and beliefs (e.g., their demand for multiple medications, antibiotic prescriptions, parenteral medications, and specialist consultations and additional tests)
Development of Aims and Measures of Improvement
At the first coaching visit, the Imereti teams also discussed and reached initial agreement regarding the overall aim of the improvement intervention as well as improvement objectives, changes to test out, and proposed indicators to assess their progress. The QI teams identified their improvement aim as “decrease morbidity and mortality among children two months to five years of age due to acute upper (rhinitis, sinusitis, pharyngitis) and lower (bronchitis, pneumonia) respiratory infections through improved case management.” Since case management of RTIs was identified as a universal challenge among all QI teams supported by the project, all QI teams (including the Samtredia QI team) identified the same overarching goal of improvement interventions, while changes tested to reach the improvement objectives were not always the same. To accurately measure the progress toward this aim, specific improvement objectives and indicators to assess care at all stages (assessment and diagnosis, treatment, parent counseling, and follow-up) were also discussed (Chitashvili and Cherkezishvili 2014).
For example, to evaluate the progress in the quality of clinical assessment and diagnosis, the teams tracked the following two indicators:
-
Percent of medical charts of children that had documentation of vital signs, weight, and height
-
Percent of medical charts of children with RTI with justified diagnosis (defined as at least one relevant symptom of the disease with duration and objective clinical finding documented in the chart)
The rationale for choosing these indicators was an identified gap found during the baseline assessment of documenting clinical symptoms and their duration in medical charts. For example, to diagnose bronchitis, the provider should at least find out whether that patient has a cough as the main symptom, record its duration, and record relevant lung sounds on both sides. However, even this elementary standard was met in only 5% of medical charts with diagnosis of bronchitis. The same problem was observed across all RTI diagnoses. Poor assessment and documentation of the diagnosis of symptoms and their duration make it impossible to assess the quality of diagnosis/differential diagnosis of RTIs and consequently, clinical decisions around disease management.
Along with improvement aims and indicators, during the first few coaching visits, the QI team also agreed on the sources for data collection, frequency, and sampling for routine monitoring, keeping in mind the need to balance resource (human and financial resources, time) availability and statistical rigor. Specifically, progress in improved RTI practices was routinely assessed through random sampling of medical charts with relevant diagnosis from the facility registries. The project’s regional coordinator visited each facility monthly to help health-care providers to select the charts and perform routine monthly monitoring. This monthly monitoring support continued throughout project implementation. In addition, the regional coordinator conducted spot checks of routine monitoring results for at least 25% of selected medical charts at each facility (requiring on average 3–4 hours of work per each facility). Routine monitoring results were entered into Excel by the regional coordinator, and the data from different QI teams were aggregated by the project team.
Testing and Implementing Changes
The changes tested by the team and progress on the indicators were analyzed by using Excel-based annotated time series charts, discussed during the learning sessions, which were held quarterly (eight sessions in all). Progress on indicators during these sessions was shown through poster displays of time series charts showing two or three of the best performing indicators as well as those with the least improvement. The team analyzed the factors and changes that contributed to the improvement and the remaining challenges to address to improve the gaps in quality of care.
The changes introduced were mostly associated with improving the knowledge, skills, and practices of care providers and knowledge and attitudes of patients related to overutilization of medications to treat pediatric RTIs. Patients’ attitudes were addressed by counseling parents and families about rational medication use. Based on knowledge and practice gaps, providers identified specific clinical topics for which they needed clinical trainings and information on up-to-date, evidence-based best practices. Table 2.1 details examples of the changes the Samtredia QI team tested to improve RTI diagnosis and management. The full set of changes tested and the evidence-based clinical interventions implemented is available (Chitashvili and Cherkezishvili 2014).
Support for Improvement
To build individual, institutional, and systems capacity (Focal Area #2 of USAID Georgia’s Global Health Initiative plan), the project supported continuous strengthening of human resources for health by providing integrated, competency-based clinical and QI trainings for medical care providers and coaching visits to facility-based QI teams participating in the improvement work in Imereti (Chitashvili 2015).
The most frequent format for improving problem solving during the coaching visits, which were usually conducted every 2 weeks, was peer review of medical charts. To conduct these reviews, under the supervision of the external advisor, the QI team members were assigned different roles, which were rotated. For example, while one team member’s role was to summarize and critically evaluate the medical chart of his/her peer, other team members discussed the case, identified gaps and best practices in the charts according to agreed indicators, and documented the medical chart review results in the routine monitoring Excel database. Project coaches identified the cases from medical charts that had the most gaps or the best compliance with clinical practice guidelines and used these as a basis for discussion with the QI team. Discussions, usually facilitated by the QI coach, centered on comparing the current care with evidence-based best practices, identifying gaps and their root causes, and discussing changes needed to improve the care. Peer review of medical charts with RTI diagnosis and case discussions were a routine part of each coaching visit.
Initially, at the hospital level, the project planned to improve hospital management of pneumonia (which occurs in about 20% of all RTI cases). However, due to rapid improvement in ambulatory management of respiratory tract infections and hospital management of pneumonia, in September 2012, the project team and QI teams decided to expand the scope of the QI intervention to the whole spectrum of respiratory tract infections at both ambulatory care and hospital levels.
To improve the clinical knowledge and practices of care providers, during the coaching visits, the QI teams received clinical and improvement capacity building through interactive lectures and presentations on evidence-based management of selected clinical conditions by the project’s external advisor. These clinical training sessions were integral parts of the coaching visits and usually were conducted in the clinic rather than in a classroom setting. The gaps in provider knowledge and practices were regularly assessed by knowledge assessment questionnaires and directly observed during clinical visits of children with RTIs. Patients for directly observed consultations were selected based on the RTI diagnosis (to ensure full range of RTI diagnosis) and patient/parent consent. Observation was conducted by QI team members, the external advisor, and other clinical consultants of the project. During such observations, after obtaining informed consent from the children’s parents, patients were invited to group consultations. During the directly observed consultations, randomly selected QI team members demonstrated their skills and knowledge by consulting with children with different RTI diagnoses. Other team members took notes and, together with the external advisor and the project team, discussed the quality of care provided after the consultations.
Another example of the on-the-job training methods used by the project was the use of local specialists to build capacity of family physicians to address the felt needs of providers. For example, during one of the team meetings, village doctors expressed their discomfort about performing otoscopy and in general based their diagnoses solely on clinical symptoms or referred patients to specialists. This created significant barriers for children in villages to access care in a timely fashion and avoid pain. All village doctors had otoscopes (distributed in 2006–2007 as part of the Primary Health Care Professionals Retraining Program funded by the European Union), but without any experience and practice, they lacked confidence and did not use this important diagnostic tool in their everyday practice. After identification of the problem, the QI team organized on-the-job trainings and a workshop on “Otoscopy in pediatric respiratory tract infections.” The workshop was conducted by the otorhinolaryngologist from Samtredia Geo Hospitals (where the QI team conducted regular meetings), together with the project team. It consisted of lectures and practical training sessions on indications, execution, and interpretation of an otoscopic exam. For these purposes, the project and QI team members invited patients from all project-supported sites and conducted free testing and consultation sessions with patients during the seminar. Typically, medical trainings in Georgia were more theory-based and less applied (i.e., theoretical lectures for large audiences, usually off-site, and without the possibility to practice newly acquired skills). The new format enabled family doctors from villages and district ambulatory clinics to immediately apply skills and knowledge received during the training under the direct supervision of highly qualified experts. Because information on the number and proportion of otitis diagnosed at the primary care level was not readily available within each and across different medical facilities, the QI team was not able to document the improvement in diagnosis of otitis at the primary care level.
To address the poor knowledge of medical care providers, the project’s main approach was not only to provide updates on evidence-based clinical practice but also to equip the team with the skills to search and assess clinical recommendations in terms of strength of evidence and its applicability to their clinical practice using the PICOT (Patient, Intervention, Comparison, Outcome, Types of Study) model . From passive “recipients” of updated evidence-based best practices from the project, members of the Samtredia QI team turned into active “consumers” of EB literature – skills they could use to identify best care practices/clinical content of improvement interventions in any clinical focus area. Specifically, the project:
-
Invited QI team members to participate in Translating Research into Practice (TRIP) on-the-job trainings, conducted by the project, in collaboration with the New York University nursing school
-
Conducted regular case study discussions and review of evidence-based medical literature during QI team meetings
-
Encouraged care providers to search for and review medical literature and have them present the literature during the regional learning sessions and medical conferences organized by the project at the local, regional, and national levels
-
Encouraged QI teams to organize workshops for other care providers and share the evidence updates on management of particular RTIs, comorbidities, and rare and interesting cases
In an environment of constantly updated evidence-based clinical recommendations based on new research findings, the project believed that such an approach built providers’ capacity to sustain improved compliance with best care practices in any clinical area of their interest even after the end of the project-supported improvement interventions. Similarly, the providers participating on the QI team could use the improvement capacity they acquired during the RTI work and apply it to any priority clinical area.
The clinical content for the above-mentioned clinical trainings was developed through close collaboration with local professional associations, such as the Georgia Family Medicine Association, Georgian Respiratory Association, Georgian Hypertension Society, Georgian Cardiology Association, Georgian Association of Pediatricians, and Georgian Association of Allergology and Clinical Immunology.
To increase utilization of continuous learning opportunities by the greatest number of physicians in Georgia, the project also supported communication and information exchanges between medical care facility managers, providers, and organizations/individuals and invited local physicians to participate in regional learning sessions and other project events (Chitashvili 2015).
Results
After 20 months of QI interventions, the Samtredia QI team dramatically improved RTI diagnosis and management practices. For example, the indicator “percent of medical charts of children with RTI with justified diagnosis” increased from 47% to 100% (Fig. 2.2).
Improvements in proper diagnosis were also accompanied by better management and treatment of RTIs, including rational antibiotic therapy. Based on the national guidelines and their original source from the British Thoracic Society, the indicator monitored by the team requires that: (1) an antibiotic is indicated, and (2) the first-choice antibiotic is selected for the patient’s age and symptoms (first-choice medication and right form, dose, and frequency). As shown in Fig. 2.3, the use of first-line antibiotics increased from 7% to 100% at project-supported sites from April 2012 to February 2014. (Note that hospital data are shown only from September 2012, when the project decided to broaden the clinical scope from pneumonia to all RTIs treated at the hospital level.)
Similarly, according to the baseline assessment, the use of other non-evidence-based (non-EB) medications (such as vitamins, short-acting methylxanthines, the so-called metabolics, expectorants, and cough depressants) was the routine practice in the region. During the project interventions, the number of non-EB medications per patient decreased from 1.12 to 0.03 at ambulatories and from 7.0 to 0.0 at the hospital in Samtredia District.
In sum, average compliance with all process indicators monitored increased by 57% from April 2012 to February 2014 (Fig. 2.4).
The cost-effectiveness analysis conducted by the project for the entire Georgia QI intervention showed that these QI interventions were effective not only in terms of improvement in evidence-based clinical practice but also from the viewpoint of rationalization of hospital pediatric pneumonia and ambulatory RTI management costs. Results showed that after 30 months of implementation of quality improvement interventions (with the assumption that the achieved level will be sustained for at least a year), the incremental cost saving per patient in the case of hospital management of pediatric pneumonia was 21.1 USD, and in the case of ambulatory management of pediatric RTI, it was 4.5 USD. Assessment of incremental cost savings using decision-tree analysis for each selected indicator showed that the intervention was more cost saving than the business-as-usual alternative. This means that as a result of the quality improvement interventions, the quality of care assessed with the selected indicators improved, simultaneously while eliminating the costs of non-EB practice. Specifically, while the project-related cost of the intervention for hospital management of pneumonia was 15,870 USD and for ambulatory management of RTIs was 23,807Footnote 1 USD, after the intervention (due to the decrease in prescribing of non-EB medications and diagnostic tests), 19,708 USD and 135,318 USD, respectively, were saved. The cost savings exceeded intervention-related expenses by 15,215 USD (9.8 USD per patient) for hospital and 102,032 USD (6.6 USD per patient) for ambulatory management of RTI. In other words, the intervention saved 9.8 USD and 6.6 USD per patient, for hospital and ambulatory management of RTI, respectively, and increased the likelihood of receiving better quality of care for pediatric RTIs in the intervention facilities (Chitashvili 2015).
Spreading the Knowledge
Along with the documented improvements, medical providers themselves also expressed a willingness to spread the modern evidence-based best practices outside of the project. With project support, they conducted two medical conferences for doctors not supported by the QI intervention. At the conferences, featured on regional TV channels, they presented their clinical cases along with critical analyses and justification of changed/improved practices. The fact that they gradually changed the themes for the conferences from the “Management of the Most Prevalent Pediatric Respiratory Diseases” (conducted in February 2012) to “Rare and Interesting cases of Pediatric Respiratory Clinical Conditions” (conducted in January 2013) illustrates also the evolution of their knowledge and confidence managing these cases.
Reflection
Thinking back, all decisions made at the beginning of the project regarding design and composition of the improvement team were successful; the design of the team allowed efficient use of project resources and took into account the intrinsic motivations not only of health-care providers but also of patients and the private corporations that owned the facilities. The choice of the project expert/coach also greatly influenced the success of the improvement effort. The expert himself attributed the success to the methodology of quality improvement: “The format the project introduced was different from the traditional trainings we were used to in the country. Intensiveness of the interventions close to clinical practice, routine monitoring of the results achieved, and enthusiasm of our colleagues in the region enabled us to exceed expectations and reach spectacular results. At the beginning of the project, we could not imagine that our doctors would manage difficult clinical cases in resource-constrained settings and have their decisions be compatible with the current best evidence. It was a pleasure to witness the transformation of the QI team from reactive listeners to proactive planners. Quite soon they started to plan the agenda for next meetings, identify the most visible gaps in their knowledge and skills, ask for trainings, bring their cases, and suggest new activities for the group. I am really happy to be part of this project and hope that this experience as well as personal contacts will continue after the end of the project.”
In contrast with other projects implemented in Georgia, this project built not only clinical but also improvement capacity of care providers and managers. Now they are equipped with the knowledge and skills to identify and manage gaps in other processes of care, as well as identify the evidence-based content of care by searching for and critically reviewing the existing scientific evidence. As one of the Samtredia QI team members, a family physician, mentioned, these are the skills she and her colleagues value the most as an outcome of the project and use in day-to-day clinical practice, regardless of the clinical area: “We were taught about the importance of guidelines during our family medicine training. For example, we received copies of 40 guidelines and training on some of them. But it is really difficult to return from [such] lectures and transform your practice in one day, without support and feedback. One needs guidance and assurance that complications came from the natural history of diseases and not from your mistakes, or because the guideline recommendation was wrong. Without this kind assistance, rarely anybody have the courage to go against widespread practice, doctors’ and parents’ beliefs […] From today’s perspective, I see that I had flaws even in understanding guidelines, for example the levels of evidence, the strength of the recommendation. When you have the deep knowledge and intensive support, it is not difficult to persuade anybody: patient, parent, colleague, employer […] And what is more important is you have the internal assurance of doing the right thing and protecting patients from unnecessary medications and risks associated with their use.”
Finally, a huge success of the project was incorporating rigorous research into the intervention design to complement the regular QI team monitoring data. The cost-effectiveness study, yet to be published, generated evidence on effectiveness and cost impact of the QI intervention which is instrumental to make evidence-based decisions at different levels of the health service delivery system in Georgia and many similar settings. Similarly, routine monitoring of the progress and regular coaching helped clinical providers to see the progress of their efforts, better understand remaining gaps, and refine changes to continuously improve the content and process of care.
The major regret for us is that due to ongoing major health sector reform and changes in governance within the health system in Georgia, scale-up of the improvement interventions was not systematically undertaken by the state and monitoring indicators were not integrated into the routine reporting systems to promote measurement and accountability.
In the future, we feel that to scale up successful QI best practices, we could also consider limiting assistance to the demonstration QI teams for 18 months and use the project resources to spread the QI interventions to other facilities using our QI champions as coaches to their peers.
Snapshot of a Changed Practice
A 6-month-old male patient was brought for an ambulatory visit in Samtredia Geo Hospitals due to nasal discharge and fever. The doctor explained to the mother that the boy had a viral respiratory tract infection, a common condition that needed no treatment other than an antipyretic (if the fever was more than 38.5 °C), comfort, and fluids. Then the doctor explained to the patient’s mother the abnormal signs for this condition and what she could do if dangerous signs occurred. The doctor explained that the drugs commonly used in previous years were not necessary. The mother later said, “At first, I was afraid to just watch my ill child suffering and not give him anything. But, after seeing the same result as with 5–6 medications for older kids, I felt assured and happy. Now I know what is dangerous and when the treatment is just comfort and warmth of the mother. I feel confident that with the close monitoring of our pediatrician, my kids will be healthy, and we will not miss anything dangerous.”
Notes
- 1.
1 USD = 1.7 GEL.
References
Chanturidze T, Ugulava T, Duran A, Ensor T, Richardson E (2009) Georgia: health system review. Health Syst Transit 11(8):1–116. Available at: http://www.euro.who.int/__data/assets/pdf_file/0003/85530/E93714.pdf
Chitashvili T (2015) Scaling up, sustaining and institutionalizing better health care in Georgia: results and strategic recommendations from USAID support for improving quality of priority clinical conditions during 2012–2015. Technical report. Published by the USAID ASSIST Project. University Research Co., LLC (URC), Bethesda. Available at: https://pdf.usaid.gov/pdf_docs/PA00W72V.pdf
Chitashvili T, Cherkezishvili E (2014) Tested changes and applied evidence-based clinical interventions to improve care of respiratory infections among children in Georgia’s Imereti region. Published by the USAID Health Care Improvement Project. University Research Co., LLC (URC), Bethesda. Available at: https://pdf.usaid.gov/pdf_docs/PA00W72T.pdf
National Center for Disease Control and Public Health (NCDC&PH) (2013) Ministry of Labour, Health and Social Affairs of Georgia. Statistical Yearbook, 2012. Tbilisi. Available at: http://ncdc.ge/AttachedFiles/2012_ebdab6ba-1aef-45af-bb77-d087e98ebeed.pdf
World Health Organization (2012) Monitoring the building blocks of health systems: a handbook of indicators and their measurement strategies. Available at: http://www.who.int/healthinfo/systems/monitoring/en/
World Health Organization and UNICEF (2013) Ending preventable child deaths from pneumonia and diarrhoea by 2025: the integrated global action plan for pneumonia and diarrhoea (GAPPD). Available at: http://apps.who.int/iris/bitstream/10665/79200/1/9789241505239_eng.pdf
Acknowledgments
The authors express special gratitude to Project Quality Advisor consultant Ivane Chkhaidze, regional coordinator Ketevan Jugheli, and the Samtredia QI team members – Tamar Loladze, Bela Bregvadze, Khatuna Kobakhidze, Ekaterine Dvalishvili, Marina Dondua, Irma Amaglobeli, Mzia Sakvarelidze, Olga Vashakidze, Nana Loria, and Tvalmaisa Amaglobeli – for their hard work, professionalism, and devotion to the improvement of health care in Georgia. The authors also express gratitude to the central management of Geo Hospitals – George Kvinikadze, Ia Sephiashvili, and Sergo Magradze – and to managers of the Samtredia branch of Geo Hospitals, Irakli Lagidze and Luara Kakhiani, for their exceptional support and contribution to team success. Finally, we appreciate the Ministry of Health, Labour and Social Affairs of Georgia, the National Center for Disease Control and Public Health, and USAID for supporting and financing the project and University Research Co., LLC (URC) for implementing the project.
The work described in this case was funded by the USAID Office of Health Systems through the USAID Applying Science to Strengthen and Improve Systems Project, implemented by URC under Cooperative Agreement Number AID-OAA-A-12-00101.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Open Access This chapter is licensed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence and indicate if changes were made.
The images or other third party material in this chapter are included in the chapter's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the chapter's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder.
Copyright information
© 2020 University Research Co., LLC
About this chapter
Cite this chapter
Chitashvili, T., Cherkezishvili, E. (2020). Improving Quality of Care for Respiratory Tract Infections in Children: The Role of Capacity Building and Coaching in Supporting One Multifacility Improvement Team in Samtredia District, Georgia. In: Marquez, L. (eds) Improving Health Care in Low- and Middle-Income Countries. Springer, Cham. https://doi.org/10.1007/978-3-030-43112-9_2
Download citation
DOI: https://doi.org/10.1007/978-3-030-43112-9_2
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-43111-2
Online ISBN: 978-3-030-43112-9
eBook Packages: MedicineMedicine (R0)