Abstract
Background: The transpetrosal approach is a complex skull base procedure with a high risk of complications, particularly caused by injury of the venous system. It is in part related to variability of blood outflow pathways and their distinctive patterns in each individual patient.
Objective: To evaluate outcomes and complications after skull base surgery with use of the petrosal approach modifications, which selection was based on the detailed preoperative assessment of venous drainage patterns.
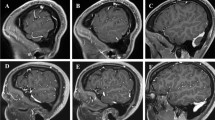
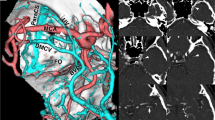
Methods: Overall, 74 patients, who underwent surgery via the transpetrosal approach at our institution between 2000 and 2017, were included in this study. In all cases, the venous drainage pattern was assessed preoperatively and categorized according to the predominant blood outflow pathway into four types as previously suggested by Hacker: (1) sphenoparietal sinus (SpPrt), (2) sphenobasal vein (SpB), (3) sphenopetrosal sinus (SpPS), and (4) cortical. The blood outflow through the bridging petrosal vein and the vein of Labbé was also taken into consideration. In patients with SpPrt- and a cortical-type venous drainage, the transpetrosal approach was used in a standard way. In patients with SpB-type venous drainage, limited extradural anterior petrosectomy was combined with intradural anterior petrosectomy after dural opening, superior petrosal sinus transection, tentorial cutting, Meckel’s cave opening, and trigeminal nerve mobilization. In patients with SpPS-type venous drainage, after standard petrosectomy, dural opening, and tentorial cutting, SpPS ligation was done followed by 2-week interval before staged definitive tumor resection.
Results: Gross total, near-total, and subtotal resection of the lesion (meningioma, 48 cases; retrochiasmatic craniopharyngioma, 11 cases; brain stem cavernoma, 7 cases; other tumors, 8 cases) was achieved in 30 (40.5%), 24 (32.4%), and 20 (27.0%) patients, respectively. Postoperative complications that were possibly related to venous compromise were noted in 18 patients (24.3%), but neither one was major. Of these 18 patients, 9 were symptomatic, but all symptoms—aphasia (4 cases), seizures (2 cases), and confusion (3 cases)—fully resolved after conservative treatment. Overall, 13 patients, including 4 symptomatic, had signal changes on T2-weighted brain MRI, which were permanent only in 3 cases (all asymptomatic).
Conclusion: Our suggested surgical strategy can be applied to any type of the venous drainage pattern. Preoperative evaluation and intraoperative preservation of the blood outflow pathways are crucial means for safe and effective application of the transpetrosal approach.
Access this chapter
Tax calculation will be finalised at checkout
Purchases are for personal use only
Similar content being viewed by others
References
Hakuba A, Nishimura S, Inoue Y. Transpetrosal–transtentorial approach and its application in the therapy of retrochiasmatic craniopharyngiomas. Surg Neurol. 1985;24:405–15.
Kawase T, Toya S, Shiobara R, Mine T. Transpetrosal approach for aneurysms of the lower basilar artery. J Neurosurg. 1985;63:857–61.
Kawase T, Shiobara R, Toya S. Anterior transpetrosal–transtentorial approach for sphenopetroclival meningiomas: surgical method and results in 10 patients. Neurosurgery. 1991;28:869–76.
Al-Mefty O, Ayoubi S, Kadri PA. The petrosal approach for the total removal of giant retrochiasmatic craniopharyngiomas in children. J Neurosurg. 2007;106(2 Suppl):87–92.
Al-Mefty O, Fox JL, Smith RR. Petrosal approach for petroclival meningiomas. Neurosurgery. 1988;22:510–7.
Bertalanffy H, Benes L, Miyazawa T, Alberti O, Siegel AM, Sure U. Cerebral cavernomas in the adult. Review of the literature and analysis of 72 surgically treated patients. Neurosurg Rev. 2002;25:1–55.
Cho CW, Al-Mefty O. Combined petrosal approach to petroclival meningiomas. Neurosurgery. 2002;51:708–18.
Erkmen K, Pravdenkova S, Al-Mefty O. Surgical management of petroclival meningiomas: factors determining the choice of approach. Neurosurg Focus. 2005;19(2):E7.
François P, Ben Ismail M, Hamel O, Bataille B, Jan M, Velut S. Anterior transpetrosal and subtemporal transtentorial approaches for pontine cavernomas. Acta Neurochir (Wien). 2010;152:1321–9.
Gross BA, Dunn IF, Du R, Al-Mefty O. Petrosal approaches to brainstem cavernous malformations. Neurosurg Focus. 2012;33(2):E10.
Hauck EF, Barnett SL, White JA, Samson D. The presigmoid approach to anterolateral pontine cavernomas. J Neurosurg. 2010;113:701–8.
Ichinose T, Goto T, Morisako H, Takami T, Ohata K. Microroll retractor for surgical resection of brainstem cavernomas. World Neurosurg. 2010;73:520–2.
Ohue S, Fukushima T, Kumon Y, Ohnishi T, Friedman AH. Surgical management of brainstem cavernomas: selection of approaches and microsurgical techniques. Neurosurg Rev. 2010;33:315–24.
Oiwa Y, Nakai K, Masaki Y, Masuo O, Kuwata T, Moriwaki H, Itakura T. Presigmoid approach for cavernous angioma in the pons—technical note. Neurol Med Chir (Tokyo) 2002;42:91–98.
Saito N, Sasaki T, Chikui E, Yuyama R, Kirino T. Anterior transpetrosal approach for pontine cavernous angioma—case report. Neurol Med Chir (Tokyo). 2002;42:272–4.
Shimamoto Y, Kawase T, Sasaki H, Shiobara R, Yamada F. Anterior transpetrosal approach to the prepontine epidermoids. Skull Base Surg. 1999;9:75–80.
Inamasu J, Shiobara R, Kawase T, Kanzaki J. Haemorrhagic venous infarction following the posterior petrosal approach for acoustic neurinoma surgery: a report of two cases. Eur Arch Otorhinolaryngol. 2002;259:162–5.
Kaplan HA, Browder J. Importance of veins in partial cerebral lobectomy. J Neurosurg. 1974;41:360–6.
Krisht AF, Barrow DL, Al-Mefty O, Dawson R, Shengelala G, Bonner G. Venous anatomy of the vein of Labbé complex. In: Hakuba A, editor. Surgery of the intracranial venous system. New York: Springer; 1996. p. 36–42.
Leonetti JP, Reichman OH, Silberman SJ, Gruener G. Venous infarction following translabyrinthine access to the cerebellopontine angle. Am J Otol. 1994;15:723–7.
Hacker H. Normal supratentorial veins and dural sinus. In: Newton TH, Potts DG, editors. Radiology of the skull and brain. Saint Louis: Mosby; 1974. p. 1851–77.
Garcia-Ibanez E, Garcia-Ibanez JL. Middle fossa vestibular neurectomy: a report of 373 cases. Otolaryngol Head Neck Surg. 1980;88:486–90.
Ohata K, Baba M. Anterior transpetrosal–transtentorial approach. In: Hakuba A, editor. Surgical anatomy of the skull base. Tokyo: Miwa Shoten; 1996. p. 77–107.
Immadoel Haq IB, Susilo IR, Goto T, Ohata K. Dural incision in the petrosal approach with preservation of the superior petrosal vein. J Neurosurg. 2016;124:1074–8.
Savardekar AR, Goto T, Nagata T, Ishibashi K, Terakawa Y, Morisako H, Ohata K. Staged ‘intentional’ bridging vein ligation: a safe strategy in gaining wide access to skull base tumors. Acta Neurochir (Wien). 2014;156:671–9.
Al-Mefty O, Krisht A. The dangerous veins. In: Hakuba A, editor. Surgery of the intracranial venous system. New York: Springer; 1996. p. 338–45.
Guppy KH, Origitano TC, Reichman OH, Segal S. Venous drainage of the inferolateral temporal lobe in relationship to transtemporal/transtentorial approaches to the cranial base. Neurosurgery. 1997;41:615–20.
Sakata K, Al-Mefty O, Yamamoto I. Venous consideration in petrosal approach: microsurgical anatomy of the temporal bridging vein. Neurosurgery. 2000;47:153–61.
Al-Mefty O, Ayoubi S, Kadri PA. The petrosal approach for the resection of retrochiasmatic craniopharyngiomas. Neurosurgery. 2008;62(5 Suppl 2 Operative):ONS331–6.
Koerbel A, Gharabaghi A, Safavi-Abbasi S, Samii A, Ebner FH, Samii M, Tatagiba M. Venous complications following petrosal vein sectioning in surgery of petrous apex meningiomas. Eur J Surg Oncol. 2009;35:773–9.
Koerbel A, Wolf SA, Kiss A. Peduncular hallucinosis after sacrifice of veins of the petrosal venous complex for trigeminal neuralgia. Acta Neurochir (Wien). 2007;149:831–3.
Masuoka J, Matsushima T, Hikita T, Inoue E. Cerebellar swelling after sacrifice of the superior petrosal vein during microvascular decompression for trigeminal neuralgia. J Clin Neurosci. 2009;16:1342–4.
Strauss C, Naraghi R, Bischoff B, Huk WJ, Romstöck J. Contralateral hearing loss as an effect of venous congestion at the ipsilateral inferior colliculus after microvascular decompression: report of a case. J Neurol Neurosurg Psychiatry. 2000;69:679–82.
Strauss C, Neu M, Bischoff B, Romstöck J. Clinical and neurophysiological observations after superior petrosal vein obstruction during surgery of the cerebellopontine angle: case report. Neurosurgery. 2001;48:1157–61.
Hafez A, Nader R, Al-Mefty O. Preservation of the superior petrosal sinus during the petrosal approach. J Neurosurg. 2011;114:1294–8.
Gupta SK, Salunke P. Intradural anterior petrosectomy for petroclival meningiomas: a new surgical technique and results in 5 patients: technical note. J Neurosurg. 2012;117:1007–12.
Ichimura S, Yoshida K, Kagami H, Inaba M, Orii M, Kitamura Y, Saga I, Toda M. Epidural anterior petrosectomy with subdural visualization of sphenobasal vein via the anterior transpetrosal approach—technical case report. Neurosurg Rev. 2012;35:609–14.
Shibao S, Toda M, Orii M, Fujiwara H, Yoshida K. Various patterns of the middle cerebral vein and preservation of venous drainage during the anterior transpetrosal approach. J Neurosurg. 2016;124:432–9.
Nakase H, Shin Y, Nakagawa I, Kimura R, Sakaki T. Clinical features of postoperative cerebral venous infarction. Acta Neurochir (Wien). 2005;147:621–6.
Ohata K, Haque M, Morino M, Nagai K, Nishio A, Nishijima Y, Hakuba A. Occlusion of the sigmoid sinus after surgery via the presigmoidal–transpetrosal approach. J Neurosurg. 1998;89:575–84.
Conflict of Interest Statement
The authors have no conflict of interest concerning the reported materials or methods.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2023 Springer Nature Switzerland AG
About this paper
Cite this paper
Nimmannitya, P. et al. (2023). Surgical Strategy in Modification of the Transpetrosal Approach to Avoid Postoperative Venous Complications: A Report of 74 Consecutive Cases. In: Turel, K.E., Chernov, M.F., Sarkar, H. (eds) Complications in Neurosurgery. Acta Neurochirurgica Supplement, vol 130. Springer, Cham. https://doi.org/10.1007/978-3-030-12887-6_4
Download citation
DOI: https://doi.org/10.1007/978-3-030-12887-6_4
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-12886-9
Online ISBN: 978-3-030-12887-6
eBook Packages: MedicineMedicine (R0)