Abstract
The aim of this study was to assess the characteristics and short-term outcome of elderly patients admitted to the ICU of ‘Sotiria’ Regional Chest Diseases Hospital of Athens. We examined retrospectively the records of 344 patients aged ≥70 years old admitted to the ICU of a tertiary hospital during a five-year period, from 2009-2013. We reported demographic and clinical data, length of ICU stay, need for mechanical ventilation and ICU mortality. Among 1730 admitted to the ICU during this period, the elderly comprised 344 (19.8%). The main causes of ICU admission were Chronic Obstructive Pulmonary Disease (COPD) exacerbation (n=169), postoperative respiratory failure (n=78), acute respiratory failure of various etiologies (n=76) and cardiogenic pulmonary edema (n=25). Overall mortality rate of elderly patients was 41.5%. According to age groups, 200 patients were 70-74 years old with a mortality rate of 47%, 42 patients were 80-84 years old presenting a mortality rate of 28.5%, while 14 patients aged over 85 years old, presented a mortality of 42.8%. The mean length of ICU stay (LOS) for the elderly patients was 11.2 days, while the corresponding LOS value for younger patients was 8.1 days. Elderly patients present highest mortality than younger population. However, mortality does not correlate exclusively with advancing age over 70 years, but mostly with the underlying disease. Therefore, age should not be the sole determinant of ICU admission.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
I. Introduction
The significant improvement of the living standards in the developed countries in the past decades, in conjunction with the scientific achievements in the fields of technology and pharmacology, has led to a notable increase in the human life span. As a result, an increased number of elderly patients require hospitalization to be treated in Intensive Care Units (ICUs) [1-3]. From a medical point of view, this group of patients is usually characterized by a higher mortality, associated with significant co-morbidities [4-7]. Therefore, elderly patients are at increased risk of being denied expensive health care resources and admission to the intensive care unit. The futility or not of ICU admission for the elderly patients remain a matter of controversy [8, 9].
The aim of this study was to report the epidemiological evidence and extrapolate possible results concerning the usefulness of ICU admission for elderly patients.
II. Study material and methods
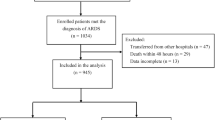
We examined retrospectively the records of all patients admitted to the ICU of ‘Sotiria’ Regional Chest Diseases Hospital of Athens in the five-year period (2009-2013). From a total of 1730 patients admitted, we studied 344 patients aged ≥70 years old. We recorded the following data: sex, age, Acute Physiology and Apache II Chronic Health Evaluation score, reason of admission, need for ventilator support, length of ICU stay and mortality. We compare these data with the corresponding data of the younger population (<70 years old) admitted to the ICU during the same period. Statistical analysis was performed using the unpaired, two tailed Student test (p,0,05 was considered significant).
III. Results
344 elderly patients (≥70 years old) were admitted during a five-year period to our ICU, when total admissions were 1730. The number of patients admitted per year (aged ≥70 years and <70) and the percentage of elderly patients among the total number of patients during the five-year period of the study are shown in table 1.
The distribution of elderly patients per year of admission and sex is presented in table 2. An equal distribution per year is noted, but there is a clear predominance of men (men/women 1.75:1). Among the elderly patients, 219 were men (63.7%) and 125 women (36.3%).
The total number and the percentage of patients in both age groups that required ventilator support during the five-year period of the study are shown in table 3. Table 3 also presents the number of deaths during the ICU hospitalization and the mortality rate both in the elderly and the younger population.
In table 4 the elderly patients are classified according to age groups.
The reasons for ICU admission of elderly patients and the corresponding Apache II score and mortality rate are shown in table 5.
The length of ICU stay of elderly patients is shown in table 6. It should be noted that from the total number of 1730 patients studied, 1423 among them (82.2%) required ventilatory support. Among 1386 patients aged <70 years, 1145 (82.6%) required ventilatory support. The overall mortality rate of the younger patients was 23.1%. Among the elderly patients, 278 (80.8%) needed ventilatory support, while mortality rate reached 41.5%.
IV. Discussion
It is frequently argued that ICU admission of elderly patients is unjustifiable due to their reduced life expectancy and the presumed higher intensive care unit and hospital mortality [9,10]. However, several studies have shown a favorable long-term outcome in previously functional elderly patients after ICU stay, although others have noted a positive correlation between advancing age and mortality [4,6,11-15,16,17,18]. According to international standards, ICU admission should be based on criteria such as the reversibility of the cause that led to the acute deterioration of the patient’s health, the life expectancy, and the former health status of the patient, without taking into account the age of the patient, except on rare occasions [19]. Nevertheless, age is often used as an important factor, while making triage decisions, especially during times of decreased critical care-bed availability.
The data presented in table 1 suggest that elderly patients comprise a relatively low percentage (19.8) compared to the total number of patients admitted in the ICU. There was also no difference recorded in the admission rate of elderly patients during the five-year period. This observation contradicts other studies, which suggest that ICUs tend more often to hospitalize critically ill elderly patients with poor prognosis [3]. According to table 2, there is a clear predominance of male patients (63.7%), and thus, it is assumed that elderly male patients present a more severe morbidity compared to female patients of the same age. It should also be noted that 83.7% of the elderly patients in our study, were between 70 and 79 years old (table 4). In our study population, acute exacerbation of chronic obstructive pulmonary disease (COPD exacerbation) represents the leading cause of ICU admission among elderly patients (49.1%), followed by postoperative respiratory failure (22.7%) and acute respiratory failure of various etiologies (22.1%), while cardiogenic pulmonary edema (7.3%) occupies the last position as shown in table 5.
Our study indicates that both groups of patients (elderly and non-elderly) required ventilatory support in an almost equal proportion (80.8% and 82.6% respectively), as shown in table 3. The average length of stay of elderly patients in the ICU (11.2 days) did not differ significantly from the respective length of stay of younger patients (8.1 days). In our study, there was no difference in the costs for the management and treatment of elderly patients, in comparison with the younger patients, as there was no treatment restriction. Costs were calculated according to the bottom-up method. Specifically, both individual patients’ costs (i.e. mechanical ventilation, clinical support consumables, respiratory physiotherapy, mean length of stay) and not related costs of patients (i.e. ICU staff remunerations) had been taken into account [20,21]. Recent studies have shown that older age is associated with reduced hospital costs. The relationship between age and costs was independent of hospital mortality, resuscitation status and discharge location. Less aggressive treatment and fewer treatment resources are possible reasons for the lower costs [22]. The statistically significant higher mortality rate of elderly patients (41.5%), compared with the overall mortality of critically ill patients admitted to the ICU (32.6%) and the mortality of the patients under 70 years old (23.1%), seems to correlate not only with age, but also with the severity of the underlying disease and the preexisting health problems. According to recent data from the literature, increased risk for developing sepsis and delirium among elderly critically ill patients are associated with the adverse outcomes in the age groups [23, 24].
Several studies have observed the short and long-term outcomes of elderly patients treated in the ICU. Short-term survival seems to correlate with the severity of illness upon admission, while long-term survival is mainly associated with the previous functional status and co-morbidities [12,25-27]. Most studies conclude that age alone is not a major determining prognostic factor and should not prevent treatment to be offered [3,12,25,28]. The above evidence, in conjunction with the mortality rate observed per disease category, suggests that the cause of ICU admission may be used as a prognostic index of the outcome. As we can observe from the study results, mortality rate doesn’t seem to correlate with advancing age above 70 years old. Age should not therefore represent an absolute criterion for ICU admission, an observation that complies with recent bibliographic data [3,25]. Another interesting result derived from this study is the gradual decrease in the mortality rate of the elderly patients admitted to the ICU during the last five years, possibly due to the better management of the patients and the higher qualification levels of the ICU staff. The decision to supply intensive health care to an elderly patient should be based on several factors, which are not solely correlated with age.
V. Conclusion
In conclusion, we suggest that medical diagnosis and the severity of the underlying disease leading to ICU admission in patients aged above 70 years represent the most important prognostic factors for their outcome. The higher qualifications of the ICU staff and the improved management of patients have led to the decrease of mortality which does not seem to be exclusively associated with advancing age above 70 years, but also with the severity of the underlying disease. Consequently age should not be considered as an inhibitory factor for the admission of elderly patients in the ICU, as survival rates may be sufficiently high when the length of stay remains within reasonable time limits.
References
Yu W, Ash AS, Levinsky NG, Moskowitz MA: Intensive care unit use and mortality in the elderly. J Gen Intern Med 2000;15:97–102.
Ip SP, Leung YF, Ip CY, Mak WP: Outcomes of critically ill elderly patients: Is high-dependency care for geriatric patients worthwhile? Crit Care Med 1999; 27:2351–7.
Nagappan R, Parkin G: Geriatric Critical Care. Crit Care Clin 2003;19:253–70.
Kass JE, Castriotta RJ, Malakoff F: Intensive care unit outcome in the very elderly. Crit Care Med 1992; 20: 1666–71.
Grace RF, Gosley M, Smith P: Mortality and outcomes of elderly patients admitted to the intensive care unit at Cairns Base Hospital, Australia. Crit Care Recusc 2007;9:334–7.
Reinikainen M, Uusaro A, Niskanen M, Ruokonen E: Intensive care of the elderly in Finland. Acta Anaisthesiol Scand 2007;51:519–21.
Blot S, Koulenti, D, Dimopoulos G, Martin, C, Komnos A, Krueger W, Spina G, Armaganidis A, Rello J, EU-VAP Study Investigators: Prevalence, Risk Factors, and Mortality for Ventilator-Associated Pneumonia in Middle-Aged, Old, and Very Old Critically Ill Patients. Crit. Care Med. 2014; 42(3): 601–609.
Sinuff T, Kahnamui K, Cook DJ, Levy MM: Values Ethics and Rationing in Critical care task Force. Rationing critical care beds: a systematic review. Crit Care Med 2004;32:1588–97.
Boyumendil A, Somme D, Garrouste-Orgeas M, Guidet B: Should elderly patients be admitted to the intensive care unit? Intensive Care Med 2007; 33:1252–62.
Marik PE: Should age limit admission to the intensive care unit? Am J Hosp Palliat Care 2007; 24:63–6.
De Rooij SE, Govers A, Korevaar JC, Abu-Hanna A, Levi M, de Jonge E: short-term and long-term mortality in very elderly patients admitted to an intensive care unit. Intensive Care Med 2006;32:965–7.
Torres OH, Francia E, Longobardi V, Gich I, Benito S, Ruiz: Short and long-term outcomes of older patients in intermediate care units. Int Care Med 2006;32:1052–9.
Kaarlola A, Tallgren M, Pettila V: Long-term survival, quality of life and quality-adjusted life-years among critically ill elderly patients. Crit Care Med 2006; 34(8):2120–6.
Adelman RD, Berger JT, Macina LO: Critical care for the geriatric patient. Clin Geriatr Med 1994;10:19–30.
Chelluri L, Grenvik A, Silverman M: Intensive care for critically ill elderly: mortality, costs and quality of life. Review of the literature. Arch Intern Med 1995;155:1013–22.
De Rooij SE, Govers AC, Korevaar JC, Giesbers AW, Levi M, de Jonge E: Cognitive, functional, and quality-of-life outcomes of patients aged 80 and older who survived at least 1 year after planned or unplanned surgery or medical intensive care treatment. J Am Griatr Soc 2008, 56 (5): 816–822.
Sprung CL, Artigas A, Kesecioglu J, Pezzi A, Wiis J, Pirracchio R, Baras M, Edbrooke DL, Pesenti A, Bakker J, Hargreaves C, Gurman G, Cohen SL, Lippert A, Payen D, Corbella D, Iapichino G: The Eldicus prospective, observational study of triage decision making in European intensive care units. Part II: intensive care benefit for the elderly. Crit Care Med 2012;40:132–138.
Nathanson BH, Higgins TL, Brennan MJ, Kramer AA, Stark M, Teres D: Do elderly patients fare well in the ICU? Chest 2011; 139:825–831.
Task Force for the American College of Critical Care Medicine, Society of Critical Care Medicine. Guidelines for ICU Admission, Discharge and Triage. Crit Care Med 1999; 27(3): 633–8.
Grigorakos L, Dimopoulos G, Nikolopoulos I, Katsanos Ch, Mavropanou D, Konstandinou K: The cost of hospitalization of patients with Chronic Obstructive Pulmonary Disease (COPD) in the Intensive Care Unit (ICU ) . Announcement at the 20th Annual Panhellenic Medical Conference, Athens, 17-21 May 1994. Volume of Abstracts, 1994: 112.
Grigorakos L, Stasinopoulou E, Markou N, Nikiteas N: Manpower and cost of Intensive Care Units (ICU ). In: Grigorakos L. Intensive Care Unit. Respiratory failure and mechanical ventilation. Before - During - After. Athens, myedition.gr, 2014, pp. 340–349.
Chelluri L, Mendelsohn AB, Bele SH, Rotondi AJ, Angus DC, Donahoe MP, Sirio CA, Schultz R, Pinsky MR: Hospital costs in patients receiving prolonged mechanical ventilation: Does age have an impact? Crit Care Med 2003; 31:1746–51.
Pisani MA: Considerations in caring for the critically ill older patient. J Intensive Care Med 2009;24:83–95.
Ahmed NN, Pearce SE: Acute care for the elderly: a literature review. Popul Health Manag 2010; 13(4): 219–225.
Marik PE: Management of the critically ill geriatric patient. Crit Care Med 2006; 34:S176–82.
Pesau B, Falger s, Berger E, Weimann J, Schuster E, Leithner C, Frass M: Influence of the age on outcome of mechanically ventilated patients in an intensive care unit. Crit Care Med 1992;20:489–92.
Meinders A, Van der Hoeven JC, Meinders AE: The outcome of prolonged mechanical ventilation in elderly patients: Are the efforts worthwhile? Age Aging 1996; 25:353–6.
Lerolle N, Trinquart L, Bornstain C, Tadié JM, Imbert A, Diehl JL, Fagon JY, Guérot E: Increased intensity of treatment and decreased mortality in elderly patients in an intensive care unit over a decade. Crit Care Med. 2010; 38(1):59–64.
Author information
Authors and Affiliations
Additional information
Authors’ Profile
Dr. Leonidas Grigorakos is an Associate Professor of Medicine (ICU) at National and Kapodistrian University of Athens (Faculty of Nursing), and Director of the Intensive Care Unit at Trauma Hospital of Athens, KAT, Kifissia, Athens, Greece.
Dr. Ioannis Nikolopoulos is a Pulmonary Specialist at the Center of Respiratory-Insufficiency - ICU Dept. at ‘Sotiria’ Regional Chest Diseases Hospital of Athens, Greece.
Dr. Katerina Sakagianni is an Anesthesiologist/Intensivist Consultant at Trauma Hospital of Athens, KAT, Kifissia, Athens, Greece.
Dr. Nikolaos Markou is a Pulmonary Specialist/Intensivist at Trauma Hospital of Athens, KAT, Kifissia, Athens, Greece.
Dimitrios Nikolaou is a Physiotherapist at Trauma Hospital of Athens, KAT, Kifissia, Athens, Greece and a Master Candidate at “Metabolic Diseases of Bones” Master Programme of the National and Kapodistrian University of Athens, Greece.
Dr. Ioannis Kechagioglou is an Anesthesiologist at Trauma Hospital of Athens, KAT, Kifissia, Athens, Greece.
Dr. Dimitris Veldekis is a Pulmonary Specialist at ‘Sotiria’ Regional Chest Diseases Hospital of Athens, Greece.
This article is distributed under the terms of the Creative Commons Attribution License which permits any use, distribution, and reproduction in any medium, provided the original author(s) and the source are credited.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made.
The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder.
To view a copy of this licence, visit https://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Grigorakos, L., Nikolopoulos, I., Sakagianni, K. et al. Intensive Care Management of The Critically Ill Elderly Population: The Case of ‘Sotiria’ Regional Chest Diseases Hospital of Athens, Greece. GSTF J Nurs Health Care 2, 13 (2015). https://doi.org/10.7603/s40743-015-0013-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.7603/s40743-015-0013-7