Abstract
Deficits in neural reward processing have been implicated in the etiology of depression and have been observed in high-risk individuals. However, depression is a heterogeneous disorder, and not all depressed individuals exhibit blunted neural reward response, suggesting the need to examine more specific depression phenotypes. Early-onset depression, a well-defined phenotype, has been associated with greater intergenerational transmission of depression and appears more closely linked to neural reward processing deficits. The present study examined whether a maternal history of early-onset depression was associated with neural reward response among mothers and their daughters. Mothers with and without a history of depression, as well as their biological, adolescent daughters (N = 109 dyads), completed a monetary reward guessing task while electroencephalogram was collected. Analyses focused on the Reward Positivity (RewP), an event-related potential following reward receipt. Adjusting for current depressive symptoms, maternal early-onset depression was associated with a blunted RewP in the mothers and a numerically smaller RewP in their never-depressed, adolescent daughters. Maternal adult-onset depression was not statistically associated with a blunted RewP in mothers or daughters. Thus, a blunted RewP appears to be a trait-like vulnerability marker for depression that emerges before depression onset and relates to more specific depression phenotypes (e.g., early-onset depression). These findings have implications for early identification of individuals at risk of depression and for developing more targeted interventions.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
A maternal history of major depressive disorder (MDD) is strongly associated with increased risk for depression in offspring (Beardselee et al., 1998; Burke, 2003; Gotlib et al., 2020; Klein et al., 2005), with children of depressed parents at approximately three times greater risk for developing depression than children of nondepressed parents (Lieb et al., 2002; Weissman et al., 2006, 2021). Depression occurs in women at approximately twice the rate of that in men (Bromet et al., 2011), a gap that emerges during adolescence (Breslau et al., 2017; Thapar et al., 2012). Depression also appears more heritable among women (Kendler et al., 2001), and daughters of depressed mothers are at particularly heightened risk of depression during adolescence (Sheeber et al., 2002; Thapar et al., 2012). However, depression is both etiologically and clinically heterogeneous (Buch & Liston, 2021; Cai et al., 2020; Fried, 2017; Lynch et al., 2020), and not all daughters of depressed mothers will develop depression themselves, complicating investigations into mechanisms of intergenerational transmission (Goodman & Gotlib, 1999).
Deficits in reward processing appear central to depression symptomology and may be one candidate by which intergenerational depression transmission occurs (Kujawa & Burkhouse, 2017; Luking et al., 2016). Both neural and behavioral measures of aberrations in reward processing have been linked to current depression (Admon & Pizzagalli, 2015; Eshel & Roiser, 2010; Halahakoon et al., 2020; Keren et al., 2018; Pizzagalli, 2014). However, there is also evidence that neural markers of reward processing can signal vulnerability for depression, in that these reward-related deficits often appear before the occurrence of depressive symptoms (Freeman et al., 2022a; Gotlib et al., 2010; Kujawa et al., 2014; Luking et al., 2016) and can prospectively predict depression symptoms and onset (Bress et al., 2013; Hanson et al., 2015; Michelini et al., 2021; Morgan et al., 2013; Nelson et al., 2016). A modest body of evidence further suggests that neural reward response is familial (Silverman et al., 2014; Weinberg et al., 2015), indicating that these measures may help to understand intergenerational depression transmission.
One useful measure of neural reward response is the Reward Positivity (RewP), an event-related potential (ERP) elicited 250 to 350 ms following reward receipt at frontocentral electrode sites (Proudfit, 2015). The RewP is thought to reflect activity in brain regions associated with reward processing (Carlson et al., 2011; Foti et al., 2011b), including the striatum and medial prefrontal cortex, and has been associated with individual differences in self-reported and behavioral measures of reward sensitivity (Bress & Hajcak, 2013). Additionally, the RewP has been proposed as a potential biomarker of depression (Proudfit, 2015; Weinberg et al., 2022). The association between the RewP and depression also appears to be state-independent; that is, a blunted RewP has been observed in currently euthymic individuals with remitted depression, suggesting it may be a trait-like marker of risk (Bowyer et al., 2019; Freeman et al., 2022a; Weinberg & Shankman, 2017). Further, a blunted RewP can prospectively predict increases in depressive symptoms (Freeman et al., 2022b), depression onset (Bress et al., 2013; Nelson et al., 2016), and first episode of recurrent/chronic depression (Michelini et al., 2021). Combined, these data suggest that the RewP may be a useful marker of depression risk.
The RewP might be particularly valuable for investigations of intergenerational transmission, given previous evidence that the magnitude of neural reward response is heritable (Li et al., 2019). Consistent with this, there is evidence from adult siblings that the RewP is familial (Weinberg et al., 2015). Additionally, a parental history of depression—particularly a maternal history—has been associated with a decreased RewP in children (Kujawa et al., 2014) and adolescents (Foti et al., 2011a; Freeman et al., 2022a), and is associated with alterations to the normative developmental trajectory of neural reward response (Ethridge et al., 2021). Taken together, a blunted RewP may be transmitted across generations, reflect underlying biological vulnerability to depression before symptom onset, and signal prospective depression risk. However, not all depressed individuals exhibit blunted reward sensitivity (Foti et al., 2014; Pelizza & Ferrari, 2009; Shankman et al., 2007), nor do all youth with a family history of depression (Suor et al., 2021).
Variations in neural reward response among those with depression may occur, in part, because depression is a heterogeneous disorder, both in terms of its presentation and etiology, suggesting the need to examine reward sensitivity in specific depression phenotypes (Shankman et al., 2007; Weinberg et al., 2016; Weinberg & Shankman, 2017). Early-onset depression appears more strongly associated with intergenerational transmission of depression and appears to be an especially heritable form of the disorder (Bland et al., 1986; Ferentinos et al., 2015; Klein et al., 2005; Levinson et al., 2003; Lyons et al., 1998; Weissman et al., 1993, 1984a, 1984b). Moreover, a parental history of early-onset, recurrent depression has been associated with greater depressive symptoms in adolescents (Jaffee et al., 2021) as well as reduced positive emotionality in children (Durbin et al., 2005). Previous neurophysiological studies have shown that adults with early-onset depression show reward-processing deficits (Shankman et al., 2007) and blunted neural responses to appetitive visual content (Weinberg et al., 2016). However, it is unclear how early-onset maternal depression relates to neural reward response in offspring. In particular, to understand whether reward processing deficits are transmitted across generations and not merely a manifestation of current depression symptoms associated with a parental depression history, it is necessary to examine these processes in high-risk children before the onset of clinically significant symptoms (Foti et al., 2011a; Freeman et al., 2022a; Gotlib et al., 2010; Kujawa et al., 2014; Luking et al., 2016; Olino et al., 2015; Sharp et al., 2014).
To this end, the present study examined the association between maternal depression history, depression age of onset, and neural reward response (i.e., RewP) in a sample of mothers with and without a history of depression and their never-depressed daughters. We hypothesized that, replicating previous research (Foti et al., 2014; Foti et al., 2011a; Freeman et al., 2022a; Kujawa et al., 2014; Liu et al., 2014; Weinberg & Shankman, 2017), women with a history of depression would exhibit a blunted neural reward response relative to women with no depression history. Further, we hypothesized that, among their never-depressed, biological daughters, girls with a maternal history of depression would exhibit a blunted neural reward response relative to girls without a maternal depression history. Finally, extending previous research (Shankman et al., 2007; Weinberg et al., 2016), we further predicted that early-onset maternal depression would be most strongly associated with a blunted RewP among mothers and daughters.
Method
Participants
Mothers and their biological daughters were recruited from the greater Montreal area to participate in a research study on neural processing of reward and threat. To determine study eligibility, mothers completed a phone screening using the Mini-International Neuropsychiatric Interview (MINI; Sheehan et al., 1998). Mother-daughter dyads were excluded if the mother endorsed mania or psychosis, as these symptoms appear to be unique from internalizing pathology (Watson, 2005) and show distinct associations with neural reward response (Nusslock & Alloy, 2017; Whitton et al., 2015). All participants were required to be fluent in English and not have experienced a head trauma resulting in loss of consciousness for 10 minutes or longer in the previous five years. Based on this screening criteria, 109 mother-daughter dyads (N = 218) were invited to the lab session. Fifty-five of the dyads were recruited based on a likely maternal history of depression or persistent depressive disorder (history of depression group), and 54 dyads were recruited based on the mother having no likely history of a major depressive episode (never-depressed group). Mothers were excluded from analyses if they did not complete the Doors task (n = 9), had unusable EEG data (i.e., too few trials retained for electrodes of interest; n = 1), had a past subthreshold manic episode (n = 1), or had a lifetime history of subthreshold depression with no lifetime major depressive episode (n = 3). For age of onset analyses, eight additional mothers were excluded for missing self-report data (n = 3), missing depression age of onset data (n = 4), or missing both (n = 1). Daughters were excluded from analyses if they did not complete the Doors task (n = 4), had a history of substance or alcohol use disorder (n = 5), had a maternal history of a subthreshold manic episode (n = 1), and/or had a maternal history of subthreshold depression with no maternal lifetime major depressive episode (n = 3). As a blunted RewP has been associated with a history of depression (Belden et al., 2016) and depressive symptoms (Bress et al., 2012) in youth, we sought to disentangle neural markers of depression risk from neural makers that may result as a consequence of experiencing a major depressive episode. Thus, daughters with a personal lifetime history of major depressive episode were also excluded (nMaternal Depression History = 13; nNever-Depressed Mother = 14). For age of onset analyses, seven additional daughters were excluded due to missing self-report data (n = 3), missing maternal depression age of onset data (n = 3), or missing both (n = 1). Thus, depression analyses focused on a subset of 95 mothers and 75 daughters, and depression age of onset analyses focused on a subset of 87 mothers and 68 daughters. Mothers were between the ages of 32 and 59 (M = 45.83, SD = 6.40), and daughters were between the ages of 10 and 19 (M = 13.73, SD = 2.53). Sample characteristics are summarized by group in Table 1.
Procedure
Participants completed informed consent or for those younger than 18 years old, mother consent and daughter assent. Mother-daughter dyads then completed a battery of questionnaires online. During the lab visit, participants completed diagnostic and life stress interviews and various computer tasks while EEG was acquired. Initial analyses from this sample and task, examining the effects of maternal history of depression on developmental trajectories of neural reward response, have been previously published (Ethridge et al., 2021). The results from other tasks in this sample are reported elsewhere (e.g., Freeman et al., 2022a). A list of measures completed by participants, the task code, syntax, and deidentified data for the analyses reported here can be found at: https://osf.io/zks9e/?view_only=f92d8c5c5eb342018e1b041e62281d2b.
Each participant was compensated $25 per hour for their time, for a total of $200 to $225 per dyad, plus earnings from the computer tasks. All procedures were approved by the McGill University research ethics board.
Measures
Diagnostic interviews
Mothers were administered the Structured Clinical Interview for DSM-5 Disorders, Clinician Version (SCID-V; First et al., 2016) to assess lifetime history of mental disorders (mood, anxiety, alcohol and substance use, trauma and stressor-related, obsessive-compulsive, and psychotic disorders). Depression age of onset data were collected during the SCID. Early-onset depression was defined as the first depressive episode occurring before 20 years old, as previous work finds that depression onset before age 20 is associated with greater familial and intergenerational transmission of the disorder (Tozzi et al., 2008; Weissman et al., 1988, 1984b). Adult-onset depression was defined as the first depressive episode occurring at 20 years or older. During the SCID, participants who struggled to recall their age of first depressive episode were provided with a timeline which interviewers used to anchor participants against memorable life events (e.g., grade in school, marriage, birth of a child). For daughters, lifetime history of mental disorders (mood, anxiety, alcohol and substance use, trauma and stressor-related, obsessive-compulsive, and psychotic disorders) were assessed using the Mini-International Neuropsychiatric Interview for children and adolescents (MINI-Kid; Sheehan et al., 2010). Interviews were conducted by PhD-level graduate students and bachelors-level research coordinators, and training and supervision of interviews was provided by a clinical psychology faculty member (AW) at monthly review meetings. Interviews were recorded, and a subset of SCIDs (n = 20) and MINI-Kids (n = 20) were recoded. Interrater reliability for depressive disorders was adequate to excellent for both the SCID (lifetime major depressive disorder K = 0.88; persistent depressive disorder K = 0.70) and MINI-Kids (lifetime major depressive disorder K = 0.70; persistent depressive disorder K = 0.64; Landis & Koch, 1977).
Inventory of depression and anxiety symptoms
Mothers completed the Inventory for Depression and Anxiety Symptoms (IDAS; Watson et al., 2007, 2008), a 99-item measure assessing depression and anxiety symptoms. Previous research has shown strong psychometric properties for the IDAS (Watson et al., 2007, 2008). Analyses focused on the summed 20-item General Depression subscale, which provides a measure of unipolar depression symptoms over the past two weeks and showed excellent internal consistency in the present sample (α = .92).Footnote 1
Mood and feelings questionnaire
Daughters completed the Mood and Feelings Questionnaire (MFQ; Angold et al., 1995) to assess depressive symptoms. In the present study, daughters completed 32 items assessing depression symptoms over the past two weeks; responses were summed to create a composite score. Previous research has shown strong psychometric properties for the MFQ (Kent et al., 1997; Wood et al., 1995). The MFQ showed excellent internal consistency in the present sample (α = .93).Footnote 2
Pubertal developmental scale
Daughters completed the Pubertal Development Scale (PDS; Petersen et al., 1988) to assess indicators of pubertal development (e.g., breast development, onset of menarche). Participants were given the option to indicate “prefer not to answer” on any item, and thus, we created individually averaged scores for each participant (Ethridge et al., 2021). In the present sample, participants completed 4.79 items on average (SD = 0.77).Footnote 3
Task
Mothers and daughters completed the doors task, which has been shown to elicit reward-related neural responses (Proudfit, 2015). Participants viewed two doors and selected which door they believed contained a prize behind it by using the left or right mouse buttons. Following their selection, participants viewed a fixation cross for 1,000 ms, followed by a green arrow pointing up or a red arrow pointing down, if they had guessed correctly or incorrectly, respectively, for 2,000 ms. Participants then saw another fixation cross for 1,500 ms, followed by a screen stating, “Click for next round.” Participants were informed that they would win $0.50 for each correct guess (gain) and lose $0.25 for each incorrect guess (loss). Feedback was randomly shown, with half of the 40 trials resulting in gain and the other half resulting in loss feedback. Mothers were compensated with $3.00, and daughters were compensated with $4.00 after the task. Mothers and daughters were compensated with these amounts so that their earnings were decoupled from their actual responses per a request from an ethics board that participants not engage in gambling-like behaviors. Mothers and daughters earned different amounts to increase believability of this minor deception. The task was administered on a Core i7 computer using Presentation software (Version 18.1, Neurobehavioral Systems, Inc., Berkeley, CA).
Psychophysiological recording and data reduction
EEG was acquired using a 32-electrode BrainVision actiCHamp system (Brain Products, Munich, Germany) with the standard 10/20 layout and a ground electrode at FPz. Data were sampled at 1,000 Hz. Vertical eye movement was monitored using electrodes placed 1 cm above and below one eye, and horizontal eye movement was recorded using electrodes placed 1 cm from the outer canthi of the eyes.
Data were processed offline using BrainVision Analyzer software (Version 2.1, Brain Products, Munich, Germany). Offline band-pass filters (0.01-30Hz, 24 dB/oct) were applied. Data were referenced to an average of TP9 and TP10, and ocular artifacts were corrected by using a variation of the Gratton method (Gratton et al., 1983). Intervals for individual channels were rejected using a semiautomatic procedure applying these criteria: (a) voltage step >50 μV, (b) a change of 175 μV within 400 ms, or (c) activity <0.5 μV within 100 ms. Data were then visually inspected, and remaining artifacts were manually rejected from individual channels. Electrode channels with fewer than five useable trials were interpolated from three to four surrounding electrodes. Gain and loss trials were then averaged separately, and baseline correction was conducted by using the 200 ms period before feedback onset.
The RewP was scored between 250 and 350 ms using data from an average of electrode-sites Fz, Cz, FC1, and FC2 (FCavg). For mothers and daughters, 0.19% and 0.98% of data at the FCavg were rejected during artifact rejection, respectively. Trial counts for the FCavg per condition for mothers and daughters are presented in Table 2. Activity in this time window and at these sites following gain and loss feedback demonstrated good to excellent internal consistency, measured by using the split-half correlation of odd and even numbered trials averaged separately for each feedback condition and corrected using the Spearman-Brown prophecy formula (mothers: rgain = .91, rloss = .87; daughters: rgain = .91, rloss = .80).
Data-analytic plan
Analyses were conducted in SPSS statistics version 27 (IBM Corp., Armonk, NY). We first conducted two paired-sample t-tests to determine whether neural response differed between gain and loss conditions among mothers and daughters. We report Pearson’s correlations among ERP measures and self-reported depressive symptoms across mothers and daughters for descriptive purposes (Table 3).
Two separate linear regressions were conducted to determine if a maternal history of depression was associated with neural response to gain among mothers and daughters. In each regression, the neural response to gain was the dependent variable, and the independent variables were mothers’ depression history (0 = No, 1 = Yes) and neural response to loss for mothers or daughters. Next, separate hierarchical linear regressions for mothers and daughters were conducted to determine whether maternal depression age of onset was associated with neural response to gain. In step 1 for each analysis (one for mothers and one for daughters), early-onset maternal depression (0 = No, 1 = Yes) and adult-onset maternal depression (0 = No, 1 = Yes) were included as predictors, alongside neural response to loss. In step 2, current depressive symptoms for mothers or daughters were added to the model to adjust for potential differences in state-level symptoms between the early- and adult-onset depression groups. Neural response to loss was included in each regression to control for variance in neural response present in both task conditions. Additional analyses examining the role of other mental disorders in the primary analyses as well as adjusting for daughters’ pubertal development are included in the supplemental materials (Tables S1-S3).
Results
Descriptive analyses
Compared with never-depressed mothers, mothers with a history of depression reported elevated depressive symptoms (Table 1). Mothers with a history of depression did not differ from never-depressed mothers on age or ethnicity; however, never-depressed mothers had a higher household income level than mothers with a history of depression (Table 1). Daughters with a maternal history of depression did not differ from daughters of never-depressed mothers on age, ethnicity, depressive symptoms, or pubertal development (Table 1).
Neural response to gain and loss
Separate paired-sample t-tests were conducted to test for neural differences in activity in response to gain and loss conditions. As expected, in the time-window of the RewP, mothers showed a significantly greater neural response to gain (MMother = 11.46, SDMother = 6.46) than loss (MMother = 9.41, SDMother = 5.58) feedback, t(94) = 5.75, p < .001. Similarly, daughters also showed greater neural response to gain (MDaughter = 12.29, SDDaughter = 8.57) than loss (MDaughter = 7.70, SDDaughter = 7.24) feedback, t(74) = 6.72, p < .001.
Depression history and neural response to gain
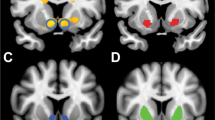
Tables 4 and 5 present the full results of the regression analyses predicting neural responses to gain from maternal history of depression, for mothers and daughters, respectively. Among mothers, a history of depression was significantly associated with a blunted neural response to gain, B = -1.43, SE = 0.71, β = -.11, p = .047 after adjusting for mothers’ neural response to loss (Table 4; Fig. 1). In contrast, among daughters, a maternal history of depression did not significantly predict neural response to gain, B = -0.79, SE = 1.38, β = -.05, p = .568 when adjusting for daughters’ neural response to loss (Table 5; Fig. 2). As reported in the supplement, this pattern of results in the daughters was the same when adjusting for daughters’ pubertal development (Table S1).
ERP waveforms and topographical maps for mothers’ RewP. (A) ERP average waveforms following gain (red) and loss (blue) feedback, and the difference wave (gray) depicting gain minus loss at the FCavg for never-depressed mothers. (B) Topographical map depicting the gain minus loss neural response difference for never-depressed mothers at the FCavg. (C) ERP average waveforms following gain (red) and loss (blue) feedback, and the difference wave (gray) showing gain minus loss at the FCavg for mothers with a history of depression. (D) Topographical map depicting the gain minus loss neural response difference for mothers with a history of depression at the FCavg.(E) ERP average waveforms following gain (red) and loss (blue) feedback, and the difference wave (gray) representing gain minus loss at the FCavg for mothers with a history of early-onset depression. (F) Topographical map depicting the gain minus loss difference for mothers with a history of early-onset depression at the FCavg. (G) ERP average waveforms following gain (red) and loss (blue) feedback, and the difference wave (gray) showing gain minus loss at the FCavg for mothers with a history of adult-onset depression. (H) Topographical map depicting the gain minus loss difference for mothers with a history of adult-onset depression at the FCavg
ERP waveforms and topographical maps for daughters’ RewP. (A) ERP average waveforms following gain (red) and loss (blue) feedback, and the difference wave (gray) representing gain minus loss at the FCavg for daughters of never-depressed mothers. (B) Topographical map depicting the gain minus loss difference for daughters of never-depressed mothers at the FCavg. (C) ERP average waveforms following gain (red) and loss (blue) feedback, and the difference wave (gray) showing gain minus loss at the FCavg for daughters of mothers with a history of depression. (D) Topographical map depicting the gain minus loss difference for daughters of mothers with a history of depression at the FCavg. (E) ERP average waveforms following gain (red) and loss (blue) feedback, and the difference wave (gray) representing gain minus loss at the FCavg for daughters with a maternal history of early-onset depression. (F) Topographical map depicting the gain minus loss difference for daughters with a maternal history of early-onset depression at the FCavg. (G) ERP average waveforms following gain (red) and loss (blue) feedback, and the difference wave (gray) showing gain minus loss at the FCavg for daughters with a maternal history of adult-onset depression. (H) Topographical map depicting the gain minus loss difference for daughters with a maternal history of adult-onset depression at the FCavg
Depression age of onset and neural response to gain
Tables 4 and 5 present the full results of the regression analyses predicting neural response to gain from maternal depression age of onset for mothers and daughters, respectively. In the mothers, early-onset depression was associated with blunted neural response to gain, after adjusting for neural response to loss and mothers’ current depressive symptoms, B = -3.50, SE = 1.10, β = -.21, p = .002 (Table 4; Fig. 1). In contrast, adult-onset depression was not significantly associated with mothers’ neural response to gain, B = -1.31, SE = 0.94, β = -.08, p = .166. As reported in the supplement, this pattern of results in the mothers was the same when adjusting for mothers’ other mental disorders (Table S2).
A similar pattern of results was seen among their never-depressed, biological daughters. Adjusting for daughters’ neural response to loss and current depressive symptoms, the association between early-onset maternal depression and neural response to gain was in the same direction and of a similar magnitude as that observed in the mothers, although the effect was non-significant, B = -3.78, SE = 1.93, β = -.16, p = .055 (Table 5; Fig. 2). Adult-onset maternal depression was not significantly associated with daughters’ neural response to gain, B = -0.89, SE = 1.54, β = -.05, p = .566. As reported in the supplement, this pattern of results in the daughters was the same when adjusting for daughters’ pubertal development or daughters’ other mental disorders (Table S1; Table S3).
Discussion
This study examined whether a history of early-onset depression is associated with neural reward response among mothers and their never-depressed, biological daughters. Early-onset depression was associated with a significantly blunted RewP among mothers and a numerically blunted RewP among their never-depressed daughters. These findings suggest that a blunted RewP may represent a state-independent vulnerability marker that emerges before depression onset, relates to more specific depressive phenotypes, and may be helpful to guide future prevention efforts.
Prior work suggests that a history of depression is associated with blunted neural reward response (Proudfit, 2015; Weinberg et al., 2022), and that this association is a stable, trait-like marker of depression risk (Bowyer et al., 2019; Freeman et al., 2022a; Weinberg & Shankman, 2017) that may be transmitted across generations (Ethridge et al., 2021; Freeman et al., 2022). Consistent with these findings and our hypotheses, mothers with a history of depression exhibited a blunted RewP relative to never-depressed mothers. In contrast to our hypotheses and prior research (Freeman et al., 2022a; Kujawa et al., 2014; Kujawa & Burkhouse, 2017), daughters with a maternal history of depression did not exhibit a blunted RewP relative to daughters of never-depressed mothers. As depression is phenotypically and etiologically heterogeneous, well-defined subgroups may provide greater insight into the intergenerational transmissibility of deficits in neural reward response. Indeed, we observed that early-onset depression was characterized by a blunted RewP among mothers. In the daughters, we observed a numerically similar, though nonsignificant, effect even when adjusting for daughters’ current depression symptoms. Importantly, these results do not appear to be attributable to differences in the current severity of depression symptoms, which did not significantly improve the model fit. Supplementary depression age of onset analyses among the mothers and daughters additionally suggested that these findings remained consistent with the reported results when adjusting for the association between other mental disorders and the RewP. Although our sample size was modest and future research should seek to replicate these effects in a larger sample, these findings suggest that blunted neural reward response is a potential trait-like risk factor for intergenerational transmission of depression, especially among those with early-onset depression.
The RewP is thought to reflect neural reward responsivity (Carlson et al., 2011; Foti et al., 2011b) and has been associated with reward-related behavior (Bress & Hajcak, 2013). Thus, mothers and daughters with a blunted RewP may be less responsive to rewards and may pursue rewarding experiences to a lesser extent than those with an intact RewP. As we tested our hypothesis in a sample of never-depressed daughters, our findings support the notion that the RewP may be a viable risk marker that emerges before symptom onset and may help to identify more specific depression risk profiles. Prior work has shown that the severity of a maternal depressive episode is associated with greater blunting of the RewP in offspring (Kujawa et al., 2014), and, moreover, that individuals with early-onset depression are at greater risk for recurrent and chronic depression, suicidality, and more severe symptoms (Rush, 2007; Sung et al., 2013). Thus, one possible alternative explanation is that the relationship between early-onset maternal depression and daughters’ RewP is due to greater maternal depression severity and not age of onset itself. Future work should gather information regarding depression severity to empirically test this hypothesis. Further, given that the effect among daughters in the current sample is nonsignificant, replication in a larger sample is needed.
As prior work suggests that early-onset depression is more likely to follow a chronic course (Dunn & Goodyer, 2006; McLeod et al., 2016), it is also possible that daughters of mothers with early-onset depression experienced greater exposure to their mother’s depression and associated stressors, such as interpersonal stress (Hammen, 2006; Hammen et al., 2012), and that such exposure may have influenced their developmental trajectory of neural reward response. Consistent with this, prior research suggests that interpersonal stress is related to blunted neural reward response (Ethridge et al., 2018; Freeman et al., 2022a; Rappaport et al., 2019). In light of these findings, another possible explanation for the association between early-onset depression and blunted neural reward response in offspring is due, in part, to greater exposure to maternal depression and associated stressors.
While early-onset depression appears to be an especially familial and heritable form of the disorder (Bland et al., 1986; Ferentinos et al., 2015; Klein et al., 2005; Levinson et al., 2003; Lyons et al., 1998; Weissman et al., 1993, 1984a, 1984b), there are multiple pathways to depression, and blunted neural reward responsivity is only one risk factor for an equifinal disorder. Additionally, not all daughters with aberrant neural reward responsivity will develop depression, and there are likely other biological and environmental factors that influence their symptom trajectory. Given that the daughters in the present analyses have no personal history of depression, it is also possible that some of the daughters of mothers with early-onset depression experience certain protective factors (e.g., social support) that reduce their propensity to develop depression in the context of multiple risk factors. Further, as the daughters in the present analyses were between 10 and 19 years old, some may develop early-onset depression themselves over time. Future work should seek to identify intersecting pathways to depression as well as to evaluate factors that may increase resilience.
The present study provides insight into depression heterogeneity and the role of specific depression phenotypes on the intergenerational transmission of neurobiological risk factors for depression. However, several limitations should be considered. First, we examined our research questions among female mother-daughter dyads given previous work showing that depression is approximately twice as common in females than males beginning in adolescence (Thapar et al., 2012) and that intergenerational associations in activation of brain regions associated with reward processing is stronger in female mother-daughter dyads compared with parent-offspring dyads of different sexes (Yamagata et al., 2016). Consequently, we were unable to assess whether our findings were consistent for paternal transmission of blunted neural reward response to offspring or whether maternal transmission is consistent in male offspring. Second, the present study is cross-sectional. Thus, we were unable to determine whether blunted neural reward response in the daughters prospectively predicted depression onset. Future research should evaluate such questions using longitudinal methods. Finally, our sample size was modest, and future work should seek to replicate our effects in a larger sample.
Overall, our findings offer novel insight into depression heterogeneity and suggest that neural reward response may be associated with familial transmission of early-onset depression more specifically. These findings underscore that, while depression is heritable and heterogeneous, enhanced understanding of specific depression phenotypes and neurobiological markers that increase depression transmissibility has implications for early detection and could ultimately aid in developing evidence-based interventions.
Notes
Five mothers were excluded from Cronbach’s alpha calculation due to missing IDAS General Depression items or data.
Eight daughters were excluded from Cronbach’s alpha calculation due to missing MFQ items or data.
PDS data were missing from four daughters.
References
Admon, R., & Pizzagalli, D. A. (2015). Dysfunctional reward processing in depression. Current Opinion in Psychology, 4, 114–118. https://doi.org/10.1016/j.copsyc.2014.12.011
Angold, A., Costello, E. J., Messer, S. C., & Pickles, A. (1995). Development of a short questionnaire for use in epidemiological studies of depression in children and adolescents. International Journal of Methods in Psychiatric Research, 5(4), 237–249.
Beardselee, W. R., Versage, E. M., & Giadstone, T. R. G. (1998). Children of affectively ill parents: A review of the past 10 years. Journal of the American Academy of Child & Adolescent Psychiatry, 37(11), 1134–1141. https://doi.org/10.1097/00004583-199811000-00012
Belden, A. C., Irvin, K., Hajcak, G., Kappenman, E. S., Kelly, D., Karlow, S., Luby, J. L., & Barch, D. M. (2016). Neural correlates of reward processing in depressed and healthy preschool-age children. Journal of the American Academy of Child & Adolescent Psychiatry, 55(12), 1081–1089. https://doi.org/10.1016/j.jaac.2016.09.503
Bland, R. C., Newman, S. C., & Orn, H. (1986). Recurrent and nonrecurrent depression: A family study. Archives of General Psychiatry, 43(11), 1085–1089. https://doi.org/10.1001/archpsyc.1986.01800110071009
Bowyer, C. B., Joyner, K. J., Yancey, J. R., Venables, N. C., Hajcak, G., & Patrick, C. J. (2019). Toward a neurobehavioral trait conceptualization of depression proneness. Psychophysiology, 56(7), e13367. https://doi.org/10.1111/psyp.13367
Breslau, J., Gilman, S. E., Stein, B. D., Ruder, T., Gmelin, T., & Miller, E. (2017). Sex differences in recent first-onset depression in an epidemiological sample of adolescents. Translational Psychiatry, 7(5), e1139–e1139. https://doi.org/10.1038/tp.2017.105
Bress, J. N., & Hajcak, G. (2013). Self-report and behavioral measures of reward sensitivity predict the feedback negativity. Psychophysiology, 50(7), 610–616. https://doi.org/10.1111/psyp.12053
Bress, J. N., Smith, E., Foti, D., Klein, D. N., & Hajcak, G. (2012). Neural response to reward and depressive symptoms in late childhood to early adolescence. Biological Psychology, 89(1), 156–162. https://doi.org/10.1016/j.biopsycho.2011.10.004
Bress, J. N., Foti, D., Kotov, R., Klein, D. N., & Hajcak, G. (2013). Blunted neural response to rewards prospectively predicts depression in adolescent girls. Psychophysiology, 50(1), 74–81. https://doi.org/10.1111/j.1469-8986.2012.01485.x
Bromet, E., Andrade, L. H., Hwang, I., Sampson, N. A., Alonso, J., de Girolamo, G., de Graaf, R., Demyttenaere, K., Hu, C., Iwata, N., Karam, A. N., Kaur, J., Kostyuchenko, S., Lépine, J.-P., Levinson, D., Matschinger, H., Mora, M. E. M., Browne, M. O., Posada-Villa, J., … Kessler, R. C. (2011). Cross-national epidemiology of DSM-IV major depressive episode. BMC Medicine, 9(1), 90. https://doi.org/10.1186/1741-7015-9-90
Buch, A. M., & Liston, C. (2021). Dissecting diagnostic heterogeneity in depression by integrating neuroimaging and genetics. Neuropsychopharmacology, 46(1), Article 1. https://doi.org/10.1038/s41386-020-00789-3
Burke, L. (2003). The impact of maternal depression on familial relationships. International Review of Psychiatry, 15(3), 243–255. https://doi.org/10.1080/0954026031000136866
Cai, N., Choi, K. W., & Fried, E. I. (2020). Reviewing the genetics of heterogeneity in depression: Operationalizations, manifestations and etiologies. Human Molecular Genetics, 29(R1), R10–R18. https://doi.org/10.1093/hmg/ddaa115
Carlson, J. M., Foti, D., Mujica-Parodi, L. R., Harmon-Jones, E., & Hajcak, G. (2011). Ventral striatal and medial prefrontal BOLD activation is correlated with reward-related electrocortical activity: A combined ERP and fMRI study. NeuroImage, 57(4), 1608–1616. https://doi.org/10.1016/j.neuroimage.2011.05.037
Dunn, V., & Goodyer, I. M. (2006). Longitudinal investigation into childhood-and adolescence-onset depression: Psychiatric outcome in early adulthood. The British Journal of Psychiatry, 188(3), 216–222. https://doi.org/10.1192/bjp.188.3.216
Durbin, C. E., Klein, D. N., Hayden, E. P., Buckley, M. E., & Moerk, K. C. (2005). Temperamental emotionality in preschoolers and parental mood disorders. Journal of Abnormal Psychology, 114(1), 28–37. https://doi.org/10.1037/0021-843X.114.1.28
Eshel, N., & Roiser, J. P. (2010). Reward and punishment processing in depression. Biological Psychiatry, 68(2), 118–124. https://doi.org/10.1016/j.biopsych.2010.01.027
Ethridge, P., Sandre, A., Dirks, M. A., & Weinberg, A. (2018). Past-year relational victimization is associated with a blunted neural response to rewards in emerging adults. Social Cognitive and Affective Neuroscience, 13(12), 1259–1267. https://doi.org/10.1093/scan/nsy091
Ethridge, P., Freeman, C., Sandre, A., Banica, I., Dirks, M. A., & Weinberg, A. (2021). Intergenerational transmission of depression risk: Mothers’ neural response to reward and history of depression are associated with daughters’ neural response to reward across adolescence. Journal of Abnormal Psychology, No Pagination Specified-No Pagination Specified. https://doi.org/10.1037/abn0000662
Ferentinos, P., Koukounari, A., Power, R., Rivera, M., Uher, R., Craddock, N., Owen, M. J., Korszun, A., Jones, L., Jones, I., Gill, M., Rice, J. P., Ising, M., Maier, W., Mors, O., Rietschel, M., Preisig, M., Binder, E. B., Aitchison, K. J., … Lewis, C. M. (2015). Familiality and SNP heritability of age at onset and episodicity in major depressive disorder. Psychological Medicine, 45(10), 2215–2225. https://doi.org/10.1017/S0033291715000215
First, M. B., Williams, J. B. W., Karg, R. S., & Spitzer, R. L. (2016). User's guide for the SCID-5-CV Structured Clinical Interview for DSM-5® disorders: Clinical version. American Psychiatric Publishing, Inc.
Foti, D., Kotov, R., Klein, D. N., & Hajcak, G. (2011a). Abnormal neural sensitivity to monetary gains versus losses among adolescents at risk for depression. Journal of Abnormal Child Psychology, 39(7), 913–924. https://doi.org/10.1007/s10802-011-9503-9
Foti, D., Weinberg, A., Dien, J., & Hajcak, G. (2011b). Event-related potential activity in the basal ganglia differentiates rewards from nonrewards: Temporospatial principal components analysis and source localization of the feedback negativity. Human Brain Mapping, 32(12), 2207–2216.
Foti, D., Carlson, J. M., Sauder, C. L., & Proudfit, G. H. (2014). Reward dysfunction in major depression: Multimodal neuroimaging evidence for refining the melancholic phenotype. NeuroImage, 101, 50–58. https://doi.org/10.1016/j.neuroimage.2014.06.058
Freeman, C., Ethridge, P., Banica, I., Sandre, A., Dirks, M. A., Kujawa, A., & Weinberg, A. (2022a). Neural response to rewarding social feedback in never-depressed adolescent girls and their mothers with remitted depression: Associations with multiple risk indices. Journal of Psychopathology and Clinical Science, 131(2), 141–151. https://doi.org/10.1037/abn0000728
Freeman, C., Panier, L., Joelle, S., & Weinberg, A. (2022b). Neural response to social but not monetary reward predicts increases in depressive symptoms during the COVID-19 pandemic. Psychophysiology. https://doi.org/10.1111/psyp.14206
Fried, E. (2017). Moving forward: How depression heterogeneity hinders progress in treatment and research. Expert Review of Neurotherapeutics, 17(5), 423–425. https://doi.org/10.1080/14737175.2017.1307737
Goodman, S. H., & Gotlib, I. H. (1999). Risk for psychopathology in the children of depressed mothers: A developmental model for understanding mechanisms of transmission. Psychological Review, 106(3), 458–490. https://doi.org/10.1037/0033-295X.106.3.458
Gotlib, I. H., Hamilton, J. P., Cooney, R. E., Singh, M. K., Henry, M. L., & Joormann, J. (2010). Neural processing of reward and loss in girls at risk for major depression. Archives of General Psychiatry, 67(4), 380–387. https://doi.org/10.1001/archgenpsychiatry.2010.13
Gotlib, I. H., Goodman, S. H., & Humphreys, K. L. (2020). Studying the intergenerational transmission of risk for depression: Current status and future directions. Current Directions in Psychological Science, 29(2), 174–179. https://doi.org/10.1177/0963721420901590
Gratton, G., Coles, M. G. H., & Donchin, E. (1983). A new method for off-line removal of ocular artifact. Electroencephalography and Clinical Neurophysiology, 55(4), 468–484. https://doi.org/10.1016/0013-4694(83)90135-9
Halahakoon, D. C., Kieslich, K., O’Driscoll, C., Nair, A., Lewis, G., & Roiser, J. P. (2020). Reward-processing behavior in depressed participants relative to healthy volunteers: A systematic review and meta-analysis. JAMA Psychiatry, 77(12), 1286–1295. https://doi.org/10.1001/jamapsychiatry.2020.2139
Hammen, C. (2006). Stress generation in depression: Reflections on origins, research, and future directions. Journal of Clinical Psychology, 62(9), 1065–1082. https://doi.org/10.1002/jclp.20293
Hammen, C., Hazel, N. A., Brennan, P. A., & Najman, J. (2012). Intergenerational transmission and continuity of stress and depression: Depressed women and their offspring in 20 years of follow-up. Psychological Medicine, 42(5), 931–942. https://doi.org/10.1017/S0033291711001978
Hanson, J. L., Hariri, A. R., & Williamson, D. E. (2015). Blunted ventral striatum development in adolescence reflects emotional neglect and predicts depressive symptoms. Biological Psychiatry, 78(9), 598–605. https://doi.org/10.1016/j.biopsych.2015.05.010
Jaffee, S. R., Sligo, J. L., McAnally, H. M., Bolton, A. E., Baxter, J. M., & Hancox, R. J. (2021). Early-onset and recurrent depression in parents increases risk of intergenerational transmission to adolescent offspring. Journal of Child Psychology and Psychiatry, 62(8), 979–988. https://doi.org/10.1111/jcpp.13356
Kendler, K. S., Gardner, C. O., Neale, M. C., & Prescott, C. A. (2001). Genetic risk factors for major depression in men and women: Similar or different heritabilities and same or partly distinct genes? Psychological Medicine, 31(4), 605–616. https://doi.org/10.1017/S0033291701003907
Kent, L., Vostanis, P., & Feehan, C. (1997). Detection of major and minor depression in children and adolescents: Evaluation of the mood and feelings questionnaire. Journal of Child Psychology and Psychiatry, 38(5), 565–573. https://doi.org/10.1111/j.1469-7610.1997.tb01543.x
Keren, H., O’Callaghan, G., Vidal-Ribas, P., Buzzell, G. A., Brotman, M. A., Leibenluft, E., Pan, P. M., Meffert, L., Kaiser, A., Wolke, S., Pine, D. S., & Stringaris, A. (2018). Reward processing in depression: A conceptual and meta-analytic review across fMRI and EEG studies. American Journal of Psychiatry, 175(11), 1111–1120. https://doi.org/10.1176/appi.ajp.2018.17101124
Klein, D. N., Lewinsohn, P. M., Rohde, P., Seeley, J. R., & Olino, T. M. (2005). Psychopathology in the adolescent and young adult offspring of a community sample of mothers and fathers with major depression. Psychological Medicine, 35(3), 353–365. https://doi.org/10.1017/S0033291704003587
Kujawa, A., & Burkhouse, K. L. (2017). Vulnerability to depression in youth: Advances from affective neuroscience. Biological Psychiatry: Cognitive Neuroscience and Neuroimaging, 2(1), 28–37. https://doi.org/10.1016/j.bpsc.2016.09.006
Kujawa, A., Proudfit, G. H., & Klein, D. N. (2014). Neural reactivity to rewards and losses in offspring of mothers and fathers with histories of depressive and anxiety disorders. Journal of Abnormal Psychology, 123(2), 287–297. https://doi.org/10.1037/a0036285
Landis, J. R., & Koch, G. G. (1977). The measurement of observer agreement for categorical data. Biometrics, 33(1), 159–174. https://doi.org/10.2307/2529310
Levinson, D. F., Zubenko, G. S., Crowe, R. R., DePaulo, R. J., Scheftner, W. S., Weissman, M. M., Holmans, P., Zubenko, W. N., Boutelle, S., Murphy-Eberenz, K., MacKinnon, D., McInnis, M. G., Marta, D. H., Adams, P., Sassoon, S., Knowles, J. A., Thomas, J., & Chellis, J. (2003). Genetics of recurrent early-onset depression (GenRED): Design and preliminary clinical characteristics of a repository sample for genetic linkage studies. American Journal of Medical Genetics Part B: Neuropsychiatric Genetics, 119B(1), 118–130. https://doi.org/10.1002/ajmg.b.20009
Li, Z., Wang, Y., Yan, C., Cheung, E. F., Docherty, A. R., Sham, P. C., Gur, R. E., Gur, R. C., & Chan, R. C. (2019). Inheritance of neural substrates for motivation and pleasure. Psychological Science, 30(8), 1205–1217.
Lieb, R., Isensee, B., Höfler, M., Pfister, H., & Wittchen, H.-U. (2002). Parental major depression and the risk of depression and other mental disorders in offspring: A prospective-longitudinal community study. Archives of General Psychiatry, 59(4), 365–374. https://doi.org/10.1001/archpsyc.59.4.365
Liu, W., Wang, L., Shang, H., Shen, Y., Li, Z., Cheung, E. F. C., & Chan, R. C. K. (2014). The influence of anhedonia on feedback negativity in major depressive disorder. Neuropsychologia, 53, 213–220. https://doi.org/10.1016/j.neuropsychologia.2013.11.023
Luking, K. R., Pagliaccio, D., Luby, J. L., & Barch, D. M. (2016). Reward processing and risk for depression across development. Trends in Cognitive Sciences, 20(6), 456–468. https://doi.org/10.1016/j.tics.2016.04.002
Lynch, C. J., Gunning, F. M., & Liston, C. (2020). Causes and consequences of diagnostic heterogeneity in depression: Paths to discovering novel biological depression subtypes. Biological Psychiatry, 88(1), 83–94. https://doi.org/10.1016/j.biopsych.2020.01.012
Lyons, M. J., Eisen, S. A., Goldberg, J., True, W., Lin, N., Meyer, J. M., Toomey, R., Faraone, S. V., Merla-Ramos, M., & Tsuang, M. T. (1998). A registry-based twin study of depression in men. Archives of General Psychiatry, 55(5), 468–472. https://doi.org/10.1001/archpsyc.55.5.468
McLeod, G. F. H., Horwood, L. J., & Fergusson, D. M. (2016). Adolescent depression, adult mental health and psychosocial outcomes at 30 and 35 years. Psychological Medicine, 46(7), 1401–1412. https://doi.org/10.1017/S0033291715002950
Michelini, G., Perlman, G., Tian, Y., Mackin, D. M., Nelson, B. D., Klein, D. N., & Kotov, R. (2021). Multiple domains of risk factors for first onset of depression in adolescent girls. Journal of Affective Disorders, 283, 20–29. https://doi.org/10.1016/j.jad.2021.01.036
Morgan, J. K., Olino, T. M., McMakin, D. L., Ryan, N. D., & Forbes, E. E. (2013). Neural response to reward as a predictor of increases in depressive symptoms in adolescence. Neurobiology of Disease, 52, 66–74. https://doi.org/10.1016/j.nbd.2012.03.039
Nelson, B. D., Perlman, G., Klein, D. N., Kotov, R., & Hajcak, G. (2016). Blunted neural response to rewards as a prospective predictor of the development of depression in adolescent girls. American Journal of Psychiatry, 173(12), 1223–1230. https://doi.org/10.1176/appi.ajp.2016.15121524
Nusslock, R., & Alloy, L. B. (2017). Reward processing and mood-related symptoms: An RDoC and translational neuroscience perspective. Journal of Affective Disorders, 216, 3–16. https://doi.org/10.1016/j.jad.2017.02.001
Olino, T. M., Silk, J. S., Osterritter, C., & Forbes, E. E. (2015). Social reward in youth at risk for depression: A preliminary investigation of subjective and neural differences. Journal of Child and Adolescent Psychopharmacology, 25(9), 711–721. https://doi.org/10.1089/cap.2014.0165
Pelizza, L., & Ferrari, A. (2009). Anhedonia in schizophrenia and major depression: State or trait? Annals of General Psychiatry, 8(1), 22. https://doi.org/10.1186/1744-859X-8-22
Petersen, A. C., Crockett, L., Richards, M., & Boxer, A. (1988). A self-report measure of pubertal status: Reliability, validity, and initial norms. Journal of Youth and Adolescence, 17(2), 117–133.
Pizzagalli, D. A. (2014). Depression, stress, and anhedonia: Toward a synthesis and integrated model. Annual Review of Clinical Psychology, 10(1), 393–423. https://doi.org/10.1146/annurev-clinpsy-050212-185606
Proudfit, G. H. (2015). The reward positivity: From basic research on reward to a biomarker for depression. Psychophysiology, 52(4), 449–459. https://doi.org/10.1111/psyp.12370
Rappaport, B. I., Hennefield, L., Kujawa, A., Arfer, K. B., Kelly, D., Kappenman, E. S., Luby, J. L., & Barch, D. M. (2019). Peer victimization and dysfunctional reward processing: ERP and behavioral responses to social and monetary rewards. Frontiers in Behavioral Neuroscience, 13, 120. https://doi.org/10.3389/fnbeh.2019.00120
Rush, A. J. (2007). The varied clinical presentations of major depressive disorder. Journal of Clinical Psychiatry, 68(8), 4.
Shankman, S. A., Klein, D. N., Tenke, C. E., & Bruder, G. E. (2007). Reward sensitivity in depression: A biobehavioral study. Journal of Abnormal Psychology, 116(1), 95. https://doi.org/10.1037/0021-843X.116.1.95
Sharp, C., Kim, S., Herman, L., Pane, H., Reuter, T., & Strathearn, L. (2014). Major depression in mothers predicts reduced ventral striatum activation in adolescent female offspring with and without depression. Journal of Abnormal Psychology, 123(2), 298–309. https://doi.org/10.1037/a0036191
Sheeber, L., Davis, B., & Hops, H. (2002). Gender-specific vulnerability to depression in children of depressed mothers. In Children of depressed parents: Mechanisms of risk and implications for treatment (pp. 253–274). American Psychological Association. https://doi.org/10.1037/10449-010
Sheehan, D. V., Lecrubier, Y., Sheehan, K. H., Amorim, P., Janavs, J., Weiller, E., Hergueta, T., Baker, R., & Dunbar, G. C. (1998). The Mini-International Neuropsychiatric Interview (MINI): The development and validation of a structured diagnostic psychiatric interview for DSM-IV and ICD-10. Journal of Clinical Psychiatry, 59(20), 22–33.
Sheehan, D. V., Sheehan, K. H., Shytle, R. D., Janavs, J., Bannon, Y., Rogers, J. E., Milo, K. M., Stock, S. L., & Wilkinson, B. (2010). Reliability and validity of the Mini International Neuropsychiatric Interview for Children and Adolescents (MINI-KID). The Journal of Clinical Psychiatry, 71(3), 17393. https://doi.org/10.4088/JCP.09m05305whi
Silverman, M. H., Krueger, R. F., Iacono, W. G., Malone, S. M., Hunt, R. H., & Thomas, K. M. (2014). Quantifying familial influences on brain activation during the monetary incentive delay task: An adolescent monozygotic twin study. Biological Psychology, 103, 7–14.
Sung, S. C., Wisniewski, S. R., Balasubramani, G. K., Zisook, S., Kurian, B., Warden, D., Trivedi, M. H., & Rush, A. J. (2013). Does early-onset chronic or recurrent major depression impact outcomes with antidepressant medications? A CO-MED trial report. Psychological Medicine, 43(5), 945–960.
Suor, J. H., Granros, M., Calentino, A. E., Phan, K. L., & Burkhouse, K. L. (2021). The interplay of childhood maltreatment and maternal depression in relation to the reward positivity in youth. Development and Psychopathology, 1–11. https://doi.org/10.1017/S0954579421000857
Thapar, A., Collishaw, S., Pine, D. S., & Thapar, A. K. (2012). Depression in adolescence. The Lancet, 379(9820), 1056–1067. https://doi.org/10.1016/S0140-6736(11)60871-4
Tozzi, F., Prokopenko, I., Perry, J. D., Kennedy, J. L., McCarthy, A. D., Holsboer, F., Berrettini, W., Middleton, L. T., Chilcoat, H. D., & Muglia, P. (2008). Family history of depression is associated with younger age of onset in patients with recurrent depression. Psychological Medicine, 38(5), 641–649. https://doi.org/10.1017/S0033291707002681
Watson, D. (2005). Rethinking the mood and anxiety disorders: A quantitative hierarchical model for DSM-V. Journal of Abnormal Psychology, 114(4), 522. https://doi.org/10.1037/0021-843X.114.4.522
Watson, D., O’Hara, M. W., Simms, L. J., Kotov, R., Chmielewski, M., McDade-Montez, E. A., Gamez, W., & Stuart, S. (2007). Development and validation of the Inventory of Depression and Anxiety Symptoms (IDAS). Psychological Assessment, 19(3), 253.
Watson, D., O’Hara, M. W., Chmielewski, M., McDade-Montez, E. A., Koffel, E., Naragon, K., & Stuart, S. (2008). Further validation of the IDAS: Evidence of convergent, discriminant, criterion, and incremental validity. Psychological Assessment, 20(3), 248–259. https://doi.org/10.1037/a0012570
Weinberg, A., & Shankman, S. A. (2017). Blunted reward processing in remitted melancholic depression. Clinical Psychological Science, 5(1), 14–25. https://doi.org/10.1177/2167702616633158
Weinberg, A., Liu, H., Hajcak, G., & Shankman, S. A. (2015). Blunted neural response to rewards as a vulnerability factor for depression: Results from a family study. Journal of Abnormal Psychology, 124(4), 878–889. https://doi.org/10.1037/abn0000081
Weinberg, A., Perlman, G., Kotov, R., & Hajcak, G. (2016). Depression and reduced neural response to emotional images: Distinction from anxiety, and importance of symptom dimensions and age of onset. Journal of Abnormal Psychology, 125(1), 26–39. https://doi.org/10.1037/abn0000118
Weinberg, A., Kujawa, A., & Riesel, A. (2022). Understanding trajectories to anxiety and depression: Neural responses to errors and rewards as indices of susceptibility to stressful life events. Current Directions in Psychological Science, 31(2), 115–123. https://doi.org/10.1177/09637214211049228
Weissman, M. M., Prusoff, B. A., Gammon, G. D., Merikangas, K. R., Leckman, J. F., & Kidd, K. K. (1984a). Psychopathology in the children (Ages 6–18) of depressed and normal parents. Journal of the American Academy of Child Psychiatry, 23(1), 78–84. https://doi.org/10.1097/00004583-198401000-00011
Weissman, M. M., Wickramaratne, P., Merikangas, K. R., Leckman, J. F., Prusoff, B. A., Caruso, K. A., Kidd, K. K., & Gammon, G. D. (1984b). Onset of major depression in early adulthood: Increased familial loading and specificity. Archives of General Psychiatry, 41(12), 1136–1143. https://doi.org/10.1001/archpsyc.1984.01790230022003
Weissman, M. M., Warner, V., Wickramaratne, P., & Prusoff, B. A. (1988). Early-onset major depression in parents and their children. Journal of Affective Disorders, 15(3), 269–277. https://doi.org/10.1016/0165-0327(88)90024-9
Weissman, M. M., Wickramaratne, P., Adams, P. B., Lish, J. D., Horwath, E., Charney, D., Woods, S. W., Leeman, E., & Frosch, E. (1993). The relationship between panic disorder and major depression: A new family study. Archives of General Psychiatry, 50(10), 767–780. https://doi.org/10.1001/archpsyc.1993.01820220017003
Weissman, M. M., Wickramaratne, P., Nomura, Y., Warner, V., Pilowsky, D., & Verdeli, H. (2006). Offspring of depressed parents: 20 years later. American Journal of Psychiatry, 163(6), 1001–1008. https://doi.org/10.1176/ajp.2006.163.6.1001
Weissman, M. M., Talati, A., Gameroff, M. J., Pan, L., Skipper, J., Posner, J. E., & Wickramaratne, P. J. (2021). Enduring problems in the offspring of depressed parents followed up to 38 years. EClinicalMedicine, 38, 101000. https://doi.org/10.1016/j.eclinm.2021.101000
Whitton, A. E., Treadway, M. T., & Pizzagalli, D. A. (2015). Reward processing dysfunction in major depression, bipolar disorder and schizophrenia. Current Opinion in Psychiatry, 28(1), 7–12. https://doi.org/10.1097/YCO.0000000000000122
Wood, A., Kroll, L., Moore, A., & Harrington, R. (1995). Properties of the Mood and Feelings Questionnaire in adolescent psychiatric outpatients: A research note. Journal of Child Psychology and Psychiatry, 36(2), 327–334. https://doi.org/10.1111/j.1469-7610.1995.tb01828.x
Yamagata, B., Murayama, K., Black, J. M., Hancock, R., Mimura, M., Yang, T. T., Reiss, A. L., & Hoeft, F. (2016). Female-specific intergenerational transmission patterns of the human corticolimbic circuitry. Journal of Neuroscience, 36(4), 1254–1260. https://doi.org/10.1523/JNEUROSCI.4974-14.2016
Funding
This work was supported by funds associated with Dr. Weinberg’s Canada Research Chair
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
The authors report no biomedical financial interests or potential conflicts of interest.
Additional information
Open practices statement
The experiment and analyses reported in this manuscript were not pre-registered. A list of measures completed by participants, the task code, syntax, and deidentified data for the analyses reported here can be found at the following link: https://osf.io/zks9e/?view_only=f92d8c5c5eb342018e1b041e62281d2b.
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
ESM 1
(DOCX 27 kb)
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Allison, G.O., Freeman, C., Renault, H. et al. Risk factors for the intergenerational transmission of depression in women and girls: Understanding neural correlates of major depressive disorder and the role of early-onset maternal depression. Cogn Affect Behav Neurosci 23, 400–414 (2023). https://doi.org/10.3758/s13415-023-01063-x
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.3758/s13415-023-01063-x