Abstract
The annual incidence of skin and soft tissue infections (SSTIs) has nearly tripled in the US since the early 1990s. Many purulent SSTIs in the community setting are caused by methicillin-resistant Staphylococcus aureus (MRSA). Incision and drainage (I&D) are indicated for most purulent MRSA infections; however, the use of adjunctive antibacterials is controversial.
The objective of this study was to systematically evaluate studies that have investigated whether or not antibacterials provide added benefit to I&D alone for purulent MRSA SSTIs.
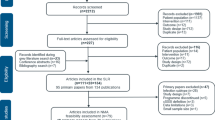
We included articles from MEDLINE and The Cochrane Library that fulfilled the following criteria: (i) original research; (ii) English language; (iii) compared I&D alone versus I&D plus antibacterials for purulent MRSA SSTIs; and (iv) compared patient outcomes. We also reviewed the references of these articles to identify other relevant studies. Studies that solely examined paediatric patients were excluded. To facilitate cross-study comparison, we systematically evaluated the following study characteristics: (i) study design; (ii) patient population; (iii) comparator groups; (iv) sample size; (v) outcome measures; (vi) outcome definitions; (vii) duration of follow-up; and (viii) measurement and adjustment of potential confounding variables.
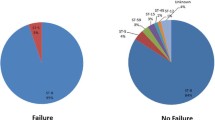
Eleven studies, spanning more than 30 years, met inclusion criteria. Two of these were conducted prior to the emergence of MRSA in the community; another evaluated cephalexin versus placebo for MRSA. None of these found added benefit of adjunctive antibacterials. Four studies compared health outcomes between patients who received ‘wactive’ or ‘appropriate’ therapy and those who received ‘inactive’ or ‘inappropriate’ therapy after I&D for purulent MRSA SSTIs. Two of these studies found ‘active’ or ‘appropriate’ therapy to be beneficial, while two others did not. Four studies compared health outcomes between patients who received anti-MRSA antibacterials plus I&D with those who received alternative antibacterials plus I&D for purulent MRSA SSTIs. Three of these reported improved outcomes with anti-MRSA antibacterials, while another reported mixed findings.
Presently, the bulk of the available evidence suggests anti-MRSA antibacterials provide added benefit to I&D alone for purulent MRSA SSTIs; however, the current evidence is limited to small, case-control, observational studies.



Similar content being viewed by others
References
Hersh AL, Chambers HF, Maselli JH, et al. National trends in ambulatory visits and antibiotic prescribing for skin and soft-tissue infections. Arch Intern Med 2008; 168: 1585–91
Moran GJ, Krishnadasan A, Gorwitz RJ, et al. Methicillin-resistant S. aureus infections among patients in the emergency department. N Engl J Med 2006; 355: 666–74
Tillotson GS, Draghi DC, Sahm DF, et al. Susceptibility of Staphylococcus aureus isolated from skin and wound infections in the United States 2005–07: laboratory-based surveillance study. J Antimicrob Chemother 2008; 62: 109–15
Stevens DL, Bisno AL, Chambers HF, et al. Practice guidelines for the diagnosis and management of skin and soft-tissue infections. Clin Infect Dis 2005; 41: 1373–406
Liu C, Bayer A, Cosgrove SE, et al. Clinical practice guidelines by the infectious diseases society of America for the treatment of methicillin-resistant Staphylococcus aureus infections in adults and children. Clin Infect Dis 2011; 52: E18–55
Taira BR, Singer AJ, Thode Jr HC, et al. National epidemiology of cutaneous abscesses: 1996 to 2005. Am J Emerg Med 2009; 27: 289–92
Rajendran PM, Young D, Maurer T, et al. Randomized, double-blind, placebo-controlled trial of cephalexin for treatment of uncomplicated skin abscesses in a population at risk for community-acquired methicillin-resistant Staphylococcus aureus infection. Antimicrob Agents Chemother 2007; 51: 4044–8
Szumowski JD, Cohen DE, Kanaya F, et al. Treatment and outcomes of infections by methicillin-resistant Staphylococcus aureus at an ambulatory clinic. Antimicrob Agents Chemother 2007; 51: 423–8
Paydar KZ, Hansen SL, Charlebois ED, et al. Inappropriate antibiotic use in soft tissue infections. Arch Surg 2006; 141: 850–4; discussion 5-6
Frei CR, Miller ML, Lewis 2nd JS, et al. Trimethoprimsulfamethoxazole or clindamycin for community-associated MRSA (CA-MRSA) skin infections. J Am Board Fam Med 2010; 23: 714–9
Schmitz GR, Bruner D, Pitotti R, et al. Randomized controlled trial of trimethoprim-sulfamethoxazole for uncomplicated skin abscesses in patients at risk for community-associated methicillin-resistant Staphylococcus aureus infection. Ann Emerg Med 2010; 56: 283–7
King MD, Humphrey BJ, Wang YF, et al. Emergence of community-acquired methicillin-resistant Staphylococcus aureus USA300 clone as the predominant cause of skin and soft-tissue infections. Ann Intern Med 2006; 144: 309–17
Frazee BW, Lynn J, Charlebois ED, et al. High prevalence of methicillin-resistant Staphylococcus aureus in emergency department skin and soft tissue infections. Ann Emerg Med 2005; 45: 311–20
Parchman ML, Munoz A. Risk factors for methicillinresistant Staphylococcal aureus skin and soft tissue infections presenting in primary care: a South Texas Ambulatory Research Network (STARNet) study. J Am Board Fam Med 2009; 22: 375–9
Tattevin P, Diep BA, Jula M, et al. Methicillin-resistant Staphylococcus aureus USA300 in long-term care facility. Emerg Infect Dis 2009; 15: 953–5
David MZ, Gilkman P, Crawford SE, et al. What is community-associated methicillin-resistant Staphylococcus aureus? J Infect Dis 2008; 197: 1235–43
Pallin DJ, Egan DJ, Pelletier AJ, et al. Increased US emergency department visits for skin and soft tissue infections, and changes in antibiotic choices, during the emergence of community-associated methicillin-resistant Staphylococcus aureus. Ann Emerg Med 2008; 51: 291–8
Edelsberg J, Taneja C, Zervos M, et al. Trends in US hospital admissions for skin and soft tissue infections. Emerg Infect Dis 2009; 15: 1516–8
Frei CR, Makos BR, Daniels KR, et al. Emergence of community-acquired methicillin-resistant Staphylococcus aureus skin and soft tissue infections as a common cause of hospitalization in United States children. J Pediatr Surg 2009; 45: 1967–74
Klein E, Smith DL, Laxminarayan R. Community-associated methicillin-resistant Staphylococcus aureus in outpatients, United States, 1999–2006. Emerg Infect Dis 2009; 15: 1925–30
Fridkin SK, Hageman JC, Morrison M, et al. Methicillin-resistant Staphylococcus aureus disease in three communities. N Engl J Med 2005; 352: 1436–44
Gorwitz RJ, Jernigan DB, Powers JH, et al. Strategies for clinical management of MRSA in the community: Summary of an experts’ meeting convened by the Centers for Disease Control and Prevention 2006 [online]. Available from URL: http://www.cdc.gov/ncidod/dhqp/ar_mrsa_ca.html [Accessed 2011 May 05]
Ellis M. The use of penicillin and sulphonamides in the treatment of suppuration. Lancet 1951; 1: 774–5
Miller LG, Quan C, Shay A, et al. A prospective investigation of outcomes after hospital discharge for endemic, community-acquired methicillin-resistant and -susceptible Staphylococcus aureus skin infection. Clin Infect Dis 2007; 44: 483–92
Khawcharoenporn T, Tice A. Empiric outpatient therapy with trimethoprim-sulfamethoxazole, cephalexin, or clindamycin for cellulitis. Am J Med 2010; 123: 942–50
Styers D, Sheehan DJ, Hogan P, et al. Laboratory-based surveillance of current antimicrobial resistance patterns and trends among Staphylococcus aureus: 2005 status in the United States. Ann Clin Microbiol Antimicrob 2006; 5: 2
Gupta K, Macintyre A, Vanasse G, et al. Trends in prescribing beta-lactam antibiotics for treatment of community-associated methicillin-resistant Staphylococcus aureus infections. J Clin Microbiol 2007; 45: 3930–4
Macfie J, Harvey J. The treatment of acute superficial abscesses: a prospective clinical trial. Br J Surg 1977; 64: 264–6
Llera JL, Levy RC. Treatment of cutaneous abscess: a double-blind clinical study. Ann Emerg Med 1985; 14: 15–9
Lee MC, Rios AM, Aten MF, et al. Management and outcome of children with skin and soft tissue abscesses caused by community-acquired methicillin-resistant Staphylococcus aureus. Pediatr Infect Dis J 2004; 23: 123–7
Duong M, Markwell S, Peter J, et al. Randomized, controlled trial of antibiotics in the management of community-acquired skin abscesses in the pediatric patient. Ann Emerg Med 2010; 55: 401–7
Ruhe JJ, Smith N, Bradsher RW, et al. Community-onset methicillin-resistant Staphylococcus aureus skin and soft-tissue infections: impact of antimicrobial therapy on outcome. Clin Infect Dis 2007; 44: 777–84
Ruhe JJ, Menon A. Tetracyclines as an oral treatment option for patients with community onset skin and soft tissue infections caused by methicillin-resistant Staphylococcus aureus. Antimicrob Agents Chemother 2007; 51: 3298–303
Frei CR, Miller ML, Forcade NA. Response: Re: Trimethprim-sulfamethoxazole or clindamycin for community-associated MRSA (CA-MRSA) skin infections. J Am Board Fam Med 2011; 24: 332–3
National Institute of Allergy and Infectious Disesases (NIAID). Uncomplicated skin and soft tissue infections caused by community-associated methicillin-resistant Staphylococcus aureus [ClinicalTrials.gov identifier NCT00730028]. US National Institutes of Health, ClinicalTrials.gov [online]. Available from URL: http://www.clinicaltrials.gov [Accessed 2012 Jan 9]
National Institute of Allergy and Infectious Disesases (NIAID). Strategies using off-patent antibiotics for methicillin resistant S. aureus ‘STOP MRSA’ [ClinicalTrials.gov identifier NCT00729937]. US National Institutes of Health, ClinicalTrials.gov [online]. Available from URL: http://www.clinicaltrials.gov [Accessed 2012 Jan 9]
Gaspari RJ, Resop D, Mendoza M, et al. A randomized controlled trial of incision and drainage versus ultrasonographically guided needle aspiration for skin abscesses and the effect of methicillin-resistant Staphylococcus aureus. Ann Emerg Med 2001; 57: 483–91
Acknowledgements
The authors would like to thank Kyllie Ryan-Hummel, Research Assistant at The University of Texas at Austin, for formatting this manuscript for submission to the journal. No funding was provided for the conduct of this review or the preparation of this paper. CRF is supported by the US NIH in the form of a NIH/KL2 career development award (RR 025766). In addition, CRF has received research grants and/or served as a scientific consultant/advisor for AstraZeneca, Forest, Ortho McNeil Janssen and Pfizer.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Forcade, N.A., Wiederhold, N.P., Ryan, L. et al. Antibacterials as Adjuncts to Incision and Drainage for Adults with Purulent Methicillin-Resistant Staphylococcus aureus (MRSA) Skin Infections. Drugs 72, 339–351 (2012). https://doi.org/10.2165/11599510-000000000-00000
Published:
Issue Date:
DOI: https://doi.org/10.2165/11599510-000000000-00000