Abstract
The potential benefits of influenza vaccination programmes targeted at children have gained increasing attention in recent years.
We conducted a literature search of economic evaluations of influenza vaccination in those aged ≤18 years. The search revealed 20 relevant articles, which were reviewed. The studies differed widely in terms of the costs and benefits that were included. The conclusions were generally favourable for vaccination, but often applied a wider perspective (i.e. including productivity losses) than the reference case for economic evaluations used in many countries. Several evaluations estimated outcomes from a single-year epidemiological study, which may limit their validity given the year-to-year variation in influenza transmissibility, virulence, vaccine match and prior immunity. Only one study used a dynamic transmission model able to fully incorporate the indirect herd protection to the wider community.
The use of dynamic models offers great scope to capture the population-wide implications of seasonal vaccination efforts, particularly those targeted at children.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Key points for decision makers
-
The majority of the studies found that childhood influenza vaccination was cost effective
-
The studies differed widely in terms of the costs and benefits that were included and the methodologies used
-
Many studies included productivity costs, which may not be relevant in all settings
The potential benefits of influenza vaccination programmes targeted at children have gained increasing attention in recent years. In the US, recommendations for influenza vaccination have expanded over the last decade to include those aged 6–23 months (2004), those aged 6–59 months (2006), and to all children aged 6 months to 18 years (2009).[1] However, despite these recommendations, vaccine uptake in US children remains relatively low.[2]
In most other developed countries, childhood influenza vaccination has not been expanded beyond targeted programmes for children at risk of influenza complications. In Europe, among 29 countries surveyed, only six (Austria, Estonia, Finland, Latvia, Slovakia and Slovenia) recommended vaccinating children without other risk indication.[3] In the UK, children under 5 years old were identified as a key target group for pandemic vaccination in 2009, with ongoing debate about whether this should be extended in future years.[4]
Children have the highest risk of influenza infection[5] and they play a key role in the transmission of influenza due to their high contact intensity at home and in schools or playgroups,[6] as well as their increased rates of viral shedding.[1] Children with pre-existing conditions (and otherwise healthy children[7,8]) also have relatively high rates of severe influenza complications, including hospitalization[9,10] and death.[11]
The societal economic impact of childhood influenza is dominated by parental work loss, both to care for a sick child and as a result of secondary infections acquired from the child.[12] There is growing evidence that childhood influenza vaccination can prevent influenza within the household and the community.[13–15] The recent controversy around the effectiveness of influenza vaccination in the elderly[16,17] has highlighted the role that childhood vaccination could play in protecting the wider community.
There are two main types of influenza vaccines currently available: the trivalent inactivated influenza vaccine (TIV), which is injected intradermally, and the live attenuated influenza vaccine (LAIV), which is given as a nasal spray. Both TIV and LAIV contain three influenza virus strains, which are reconsidered and recommended by the WHO on an annual basis.[18]
Several comparative trials suggest the superiority of LAIV over TIV for the prevention of influenza in children.[19–22] However, LAIV has been associated with increased (although relatively low) rates of adverse events and is not currently recommended for children under 2 years of age or those with risk conditions.[23] LAIV is also more expensive than TIV. In most regions, including the US and Europe, TIV is licensed to be used in individuals aged older than 6 months. Licensure of LAIV has been approved in the US for non-pregnant individuals aged 2–49 years.[1] The European Medicines Agency has approved LAIV for those aged 2–18 years.[24]
The aim of this review was to appraise the published economic evaluations of childhood influenza vaccination to help characterize the numerous sources of complexity in estimating the epidemiological and economic impact of vaccination. By doing this, we hope to provide researchers and policy makers with a better understanding of the alternative methodological approaches applied, as well as offer guidance for future evaluations.
1. Search Strategy
We conducted a literature search for English-language economic evaluations of influenza vaccination in individuals aged ≤18 years. We excluded studies of vaccination options exclusively targeted at specific risk groups and those targeted at pandemic influenza prevention. A previous primarily descriptive literature review[12] was used to identify 15 relevant publications published before 2006.[25–38] We excluded one study from the previous review because it did not relate the cost data collected to health benefits.[39] New publications up to October 2010 were identified through Scopus literature searches using the search terms (as keyword, title or abstract) ‘influenza’ AND ‘vaccine’ (or ‘vaccin’, ‘vaccination’, ‘immunization’, ‘immunisation’) AND ‘economic’ (or ‘cost-effectiveness’, ‘cost-benefit’, ‘cost-utility’, ‘cost effectiveness’, ‘cost benefit’, ‘cost utility’). The search identified six new publications that met our criteria and were not included in the previous review.[40–45] Thus we retained a total of 20 economic evaluations for review.
2. Economic Evaluations of Childhood Influenza Vaccination
2.1 Efficacy and Endpoints
Most studies used efficacy estimates against one of two outcomes: clinically diagnosed influenza-like illness (ILI) and/or laboratory-confirmed influenza infection. However, several studies (e.g.[32,35,42,45]) applied efficacy estimates against influenza-related healthcare resource use such as hospital admissions. One study also considered efficacy against otitis media.[27]
Table I shows vaccine efficacy figures used in the studies. For comparison, a recent Cochrane review reported vaccine efficacy in healthy children below 16 years old of 59% (95% CI 41, 71) against confirmed influenza and 36% (95% CI 24, 46) against ILI for inactivated vaccines.[46] Equivalent estimates for live vaccines were 82% (95% CI 71, 89) against confirmed influenza and 33% (95% CI 28, 38) against ILI (although there were no studies in children under 2 years old). On the whole, the efficacy values used in economic evaluations appear to be in line with the results of the Cochrane review.[46]
Several economic evaluations used estimates of vaccine efficacy and disease incidence based on a single clinical trial[27,30,35,40,43,44] or observational study.[42,45] While this is arguably a pragmatic and defensible option for some medical interventions, for influenza vaccination it is problematic since the transmissibility, virulence, vaccine match and prior immunity vary from year-to-year.[47] For instance, Salleras et al.[45] did not include the possibility of hospitalization or mortality due to influenza as these endpoints were not observed in the trial alongside which the evaluation was conducted. In such cases, a lack of observed severe disease may be due to trial sample size and/or milder circulating strains; however, it is unlikely to be generalizable to population-wide programmes run over multiple influenza seasons.
Likewise, in some years influenza vaccines can be poorly matched to the predominant influenza strain, possibly due to a shift in antigenic composition. Such effects not only reduce vaccine effectiveness but can also increase the incidence and severity of influenza that year, since the general population has less pre-existing natural immunity. A Cochrane review of influenza vaccination in adults found that inactivated parenteral vaccines were less efficacious when the content did not match WHO recommendations and the circulating strains.[18] One review suggested that, in the decade 1987–1997, a good match between vaccine and the predominant strain was made in 50% of seasons.[48]
The use of non-specific endpoints (such as ILI) can be problematic.[47] Clinical case definitions can differ from study to study, and while standardized ILI definitions are useful, their specificity and positive predictive value may still vary with the circulating pathogens. One study estimated the positive predictive value of ILI as an indicator of influenza as 0.36 in children aged ≤14 years.[49] The use of ILI as an outcome measure in young children may be particularly problematic, as they are less likely to show typical clinical features and the burden of respiratory syncytial virus (RSV) may be substantial.[50] Marchetti et al.[41] applied trial estimates of ILI efficacy from an international meta-analysis to country-specific ILI disease rates. Any difference in the positive predictive value of ILI between these sources introduces bias; for example, if the country-specific ILI disease rates include a lower proportion of true influenza cases than the efficacy trial, this may lead to overestimating the impact of vaccination on these cases.
The use of non-specific endpoints also has implications for estimating average resource use (and other model outcomes). Such estimates may be diluted by the examination of ILI cases, which are often less severe than influenza cases.[51] For example, laboratory-confirmed influenza outpatient costs have been found to be significantly higher than ILI outpatient costs.[52] If these lower ILI-related outcome estimates are applied to influenza prevented cases, this may underestimate the benefits of vaccination. Conversely, the benefits of influenza prevention may be overestimated when using estimates from laboratory-confirmed influenza, if there is a bias to test more severe cases.
Adverse events associated with influenza vaccination were included in some, but not all, studies (table II). Where included, they were generally not found to be influential in determining cost effectiveness. Inclusions of such events are likely to be more important when assessing LAIV than when assessing TIV.
Summary of factors (cost or benefit) included in each of the base-case economic evaluations of influenza vaccination in individuals aged ≤18 years. Dark grey indicates the choice made about inclusion of the factor would likely be favourable to the cost effectiveness of a vaccine programme and light grey indicates it would likely be unfavourable. The final column indicates whether the study found vaccination to be cost saving
2.2 Indirect Protection
Influenza vaccination not only protects the vaccine recipients, but may also indirectly protect their social contacts and the wider population. This effect is often represented using dynamic models,[53] which aim to mimic the underlying time-varying dynamics of transmission by relating the risk of infection to the proportion of infected people in the population. The risk of infection (or force of infection when it relates to susceptible individuals only) decreases as a result of vaccination. This contrasts with static models, which apply a fixed (or static) risk of infection that does not change as a result of vaccination in the model. Only one of the reviewed studies (Weycker et al.[34]) used a dynamic model. It was based on an earlier agent-based microsimulation model, which tracked the transmission of influenza among individuals in a hypothetical population as they moved between communities, households, schools and workplaces.[54] The remaining studies used static models in which the risk of infection is independent of the proportion of the population that is infectious.[53]
Several of these studies incorporated a proxy indirect effect via a reduction in influenza or ILI among household contacts of vaccinated children, based on clinical trials or observational studies.[26,27,30,35,38,40,41,44] However, the impact of influenza vaccination goes beyond immediate household members; for example, contacts of vaccinated children in schools and playgroups are also protected, and adult household contacts are less likely to transmit influenza to contacts at work. This population-wide effect of influenza vaccination can be larger than that predicted by a clinical trial; on the other hand, if a sufficient proportion of the population is already protected, then increasing vaccine coverage produces diminishing returns.[54–56] For instance, vaccinating two children in the same family is not likely to provide twice the level of indirect protection as vaccinating a single child. Estimating indirect effects using dynamic models is usually preferable to doing so based on results from clinical trials, which are usually designed to estimate the short-term effects of interventions on an individual level.[57] Observational post-licensure studies can be more informative in this respect, but the circulating strains, household structure and contact patterns can be country specific, making inferences to other settings problematic.
Several other dynamic models of seasonal influenza vaccination in children have been published,[54–56] although most of these have not been linked to economic analyses. One of the challenges for dynamic models in this context is that their results are highly sensitive to the estimated social contacts that enable transmission of infections. Ideally, these models require age-specific data on effective contacts between susceptible and infectious hosts in various social situations. These contact estimates should also be adjusted for part of the infectious period to account for the fact that the behaviour and effective contacts of infected individuals change when they show symptoms of disease. Due to important advances in the collection of social contact data to parameterize infectious disease transmission models over the last 5 years, such data are beginning to emerge for an increasing number of countries.[6,58] The use of such data has been shown to provide better fits to empirical observations than was previously possible when researchers were forced to use more simplified and uncertain contact patterns in such models.[59,60]
For influenza, ignoring indirect effects altogether would underestimate the potential benefits of vaccination. Therefore, if an analysis indicates that an option for influenza vaccination is cost effective compared with non-vaccination, it would only reinforce that finding when indirect herd effects are added. However, one of the key aims of conducting a cost-effectiveness analysis of childhood influenza vaccination is to find out for which age groups influenza vaccination is most cost effective. This type of analysis should be conducted in an incremental manner comparing an option against the next best feasible alternative (e.g. no vaccination vs vaccinating 6–23 month olds vs vaccinating 6–35 month olds, etc.). In such an approach, the influence of indirect effects (including those beyond the household) on the choice of the optimal age groups to vaccinate is likely to be large. If influenza vaccines can (partially) interrupt transmission, then the potential degree of herd protection that childhood vaccination could offer to adults may be large. Therefore, exploring the impact of accounting for the infectious nature of influenza (by modelling the transmission dynamics) is a necessary requirement to investigate uncertainty in model outcomes as a result of the choice of a particular model structure (structural uncertainty).[61,62] While the parameter uncertainty in empirical social contact patterns can be included in sensitivity analysis, it would be impossible to account for the unknown structural uncertainty if this dynamic model option is not explored at all.
One key aspect of influenza epidemiology and vaccine impact that is difficult to capture in simple models is immunity. Both past infections and vaccination can induce immunity to a new infection that can last longer than a single influenza season, but this will eventually wane. Furthermore, individuals who are naturally infected with influenza may have a reduced risk of future infection, although this effect will diminish due to gradual mutational changes in the antigenic type of the dominant influenza strains each season.[63] This effect is more likely to occur in an unvaccinated individual, which implies that the benefit of increasing vaccination uptake will diminish with the increasing age of a cohort. One model assumed that infected individuals had a chance of acquiring protective immunity lasting 10 years,[29] but none of the other models reviewed took this into account. Appropriately incorporating the role of immunity will have an important effect on the long-term impact of vaccination and hence its cost effectiveness.
2.3 Costs and Benefits Evaluated
The studies differed widely in terms of the costs and benefits that were included (table II). All but two[31,32] of the studies were conducted from a societal perspective, considering benefits regardless of to whom they were accrued. Of these, all but two[25,29] considered the value of lost productivity due to caregivers missing work to care for sick children. Some studies also considered the value of lost productivity due to household contacts (e.g. caregivers) becoming sick,[26,27,30,34,35,38,40,41,44] to the children themselves in the value of lost school attendance,[29,44,45] and the value of lost lifetime productivity due to premature death.[33,34,42]
The valuation of time losses can be approached in several ways. Most studies used the costs of lost productivity (based on earnings) to value lost time due to morbidity and mortality. An exception was Salleras et al.,[45] who used willingness-to-pay estimates to value the avoidance of work and school absenteeism. Willingness-to-pay studies are conceptually more comprehensive valuations of the benefits of health gains to the individual and are, therefore, considered superior in the welfarist framework of economic evaluation.[64,65] However, they have been criticized for lacking methodological rigour and consistency in practice.[64,65] It is of note that none of the studies that valued time losses due to the combination of influenza-related morbidity and mortality did this on the basis of a willingness-to-pay study.
The two studies that took a third-party payer or provider perspective[31,32] were among the few to conclude that vaccinating low-risk children was not cost saving. Several other studies conducted sensitivity analyses, which additionally adopted a payer or provider perspective. Of these, three concluded that vaccination was no longer cost saving from this perspective,[30,38,42] and only one suggested that vaccination was still cost saving.[37] This suggests that the more favourable conclusions drawn from studies conducted using a societal perspective need to be interpreted appropriately by healthcare authorities in countries such as the UK[66] and Canada,[67] given that their guidelines for health technology assessment prescribe a payer or provider perspective.[68]
The majority of studies presented the net value or benefit/cost ratio of an intervention in monetary terms, i.e. the cost of the vaccination programme compared with the direct and indirect societal costs avoided through the intervention.[26–30,32,33,35,37,38,42,44,45] However, several such studies can be regarded as incomplete cost-benefit analyses because they only valued benefits in terms of avoided morbidity (i.e. the value of healthcare costs and productivity saved),[26–28,30,32,37,44,45] and not in terms of avoided mortality.[69]
Several studies took an extra-welfarist approach by measuring benefits in terms of non-monetized utilities such as QALYs.[25,36,40,41,43] Estimating quality of life in small children can be problematic, because none of the standard quality-of-life instruments were designed to be administered in children under the age of 5 years. These studies surveyed caregivers to act as proxies for the ill child.[70] Most of these studies were relatively recent (all but one[25] were published after 2006), possibly reflecting the increasing preference for this approach by healthcare authorities. However, the benefits captured were not consistent between studies. Some studies included benefits in both the denominator (i.e. utilities, such as QALYs) and the numerator (e.g. productivity gains) of the cost-utility ratio.[41,43] This practice has been questioned by some economists who believe that this can result in double counting.[68,71] Apart from being challenged on the above theoretical grounds, many (country-specific) guidelines for health technology assessment also explicitly state only direct medical costs should be included on the costs side.[72]
Several evaluations, particularly those targeted specifically at healthy children, did not include serious influenza complications (table II). Some argued for the exclusion of mortality on the basis that childhood deaths due to influenza are rare and/or difficult to observe in a single trial.[26,32,37,45] However, studies suggest that healthy children, while at a lower risk, contribute to influenza-related hospitalizations[7] and deaths.[8] The failure to include deaths may be problematic, since the benefit of a single avoided child death is substantial in most economic evaluation frameworks. However, the omission may be less important in studies that found a favourable result despite not valuing all the benefits. Only one study used a population dynamic model to account for the indirect protection to the elderly,[34] who have by far the highest risk of influenza-related death.[11,73] This study based death rates on modelled rates of ‘excess’ disease[11] and estimated that the majority of deaths prevented by childhood vaccination would be in those aged over 65 years.[34] The future inclusion of modelled ‘excess’ disease rates demands further discussion around the accuracy and interpretation of such estimates.[47,73]
In the studies reviewed, various methodological and modelling decisions seemed to be associated with vaccine programmes being found to be cost saving (table II). Studies that included productivity losses (due to illness and caregiving) appear more likely to be cost saving; however, in some cases reductions in time losses were offset by those incurred by caregivers to obtain vaccination for their child. The inclusion of indirect protection to other (non-targeted) age groups also appears to be associated with a programme being found cost saving. The inclusion of influenza complications did not appear to be strongly associated with cost effectiveness but is likely to be more influential in models that incorporate indirect protection to the elderly.
2.4 Administration
Several US studies have compared the cost effectiveness of a vaccine administered on an individual level (e.g. in a primary healthcare visit) with one administered on a group level (e.g. in a school-based campaign).[26,30] Another US study compared a programme delivering vaccines during working hours with one offering more flexible hours of delivery.[27] In all cases, a programme that does not require caregivers to miss work in order to bring their children for vaccination was substantially more cost effective. However, none of these studies considered the possible additional expense of bringing vaccines to a school-based setting or making them available outside office hours in the absence of existing infrastructure to do this. The caregiver time costs of vaccinating a child was often a substantial component in the total cost of vaccination in the studies in which it was included.[26,27,30,35–38,41,43,45] For instance, Prosser et al.[36] estimated caregiver vaccination time costs to account for 41–66% of total vaccination costs. This aspect might be less important in (non-US) settings where childhood vaccination already occurs routinely outside office hours (e.g. through communal services in some European countries).
Influenza vaccines are typically given in a single dose per season, but children aged less than 9 years who have not had a previous influenza vaccination are recommended to receive a second dose at least 4 weeks after the initial dose in the same influenza season.[1,74] Several models acknowledge that some children may require two doses by assuming a proportion of each vaccinated cohort receives two doses, while the remainder only receive a single dose.[27,30,32,33] This would be sufficient when evaluating an existing childhood immunization programme, but does not account for the need to vaccinate the full cohort of children reaching the age of vaccination in the first year of a new vaccination programme. The first year is particularly important in an economic model since costs and benefits in future years are reduced by discounting. A few models have captured this effect by following a cohort over several seasons[41] or by presenting separate results for the first and subsequent year of a vaccination programme.[38] However, none of the models captured the persistence of vaccine protection beyond a single season.[75,76]
2.5 Variability and Uncertainty
Although all studies conducted some form of sensitivity analysis, several studies only conducted one-way sensitivity analysis,[25–27,29,35,38,40,42,42,44,45,45] which is generally considered inadequate to explore parameter uncertainty.[77] Furthermore, many of the factors most influential to cost effectiveness were methodological choices (table II), rather than those related to parameter estimation. In several of the studies, these choices were not discussed in detail.
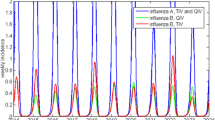
In addition to uncertainty around appropriate parameter values, influenza epidemics have seasonal variability in transmissibility, virulence, vaccine match and prior immunity.[47] This variation needs to be considered when estimating parameter values, particularly those that are based on a single (or small number of) influenza season(s). For example, a long-term prospective study in children under 5 years of age found annual laboratory-confirmed symptomatic influenza rates varied from 1% to 19% over a 25-year period.[78]
The evaluation of indirect herd protection adds an additional complexity to seasonal variability. For example, high coverage vaccination programmes may, in some seasons, be able to largely mitigate an influenza epidemic and, in others, only lessen the impact.[55] Accurately estimating the likely indirect impact of a programme (over several seasons) cannot be achieved by using the average parameter values, as variability in many variables will not have a linear impact on model results.[79]
3. Recommendations
During the latest (2009) influenza pandemic, dynamic models were widely used to inform prevention and control efforts.[80–82] These pandemic evaluations focused on trying to understand the ways in which alternative interventions, including vaccination, would impact the transmission of influenza in the community. This approach is different to that taken in most of the seasonal influenza evaluations we have reviewed, which focused on the protection of those directly targeted by vaccination (and, in some cases, their households). The use of dynamic models offers great scope to help inform seasonal vaccination efforts, particularly those targeted at children. However, care must be taken to ensure they are appropriately structured and parameterized, and that they capture the inherent variability involved in influenza control.
Future models should ideally consider the analysis of smaller age-based (and if possible risk-based) groupings. The amalgamation of groups with heterogeneous disease risks (and outcome values) is likely to be the most problematic. For example, the risk of severe influenza complications is significantly higher in those aged under 2 years than in older children, and the evidence for the efficacy of TIV in this group remains weak.[46] As discussed in section 2.2, the use of multiple age groupings will also allow the appropriate incremental analysis of alternative options for vaccination against the next best alternative. It would be useful for future evaluations to present the incremental effects with and without different benefits (e.g. caregiver productivity losses, indirect herd protection) in scenario analyses. This will allow decision makers to better understand the impact of these different factors, and give their own weighting to the importance they wish to attach to these factors. Due to the year-to-year variability in influenza, models should be informed by studies (or meta-analyses) of multiple seasons. Where non-specific endpoints, such as ILI, must be used, they should be applied with caution.[47]
This review has highlighted the role of modelling assumptions and methodological decisions in economic evaluation of influenza vaccination. Analysts need to be explicit about their assumptions and justify these, acknowledging the shortcomings of these choices. Policy makers need to ensure that they rely on evidence from studies that are consistent with their guidelines for health technology assessment. Although more realistic models (such as those incorporating dynamic effects and stratified population groups) impose trade-offs in terms of model complexity and the data needed to parameterize them, they should be used in situations where herd effects and heterogeneities are important. This seems to be the case for evaluations of universal childhood influenza vaccination.
4. Conclusions
Universal childhood influenza vaccination is not currently recommended in most countries. Although we identified 20 economic evaluations on childhood influenza vaccination, most of these were conducted for the US and adopted a wider perspective (i.e. including productivity losses) than the reference case for economic evaluations used by many governments. Therefore, their favourable results may not be transferable to all settings. Furthermore, the primary public health basis for childhood influenza vaccination – vaccinating healthy children in order to protect children at higher risk and the elderly – may be difficult to use as a basis for convincing parents about the importance of childhood vaccination. The recent empirical evidence of herd protection[14] may prove to be a turning point in stimulating governments’ interests in childhood influenza vaccination. Ideally future policy decisions should be informed by independent and thorough economic evaluations using appropriately parameterized dynamic models.
References
Fiore AE, Shay DK, Broder K, et al. Prevention and control of seasonal influenza with vaccines: recommendations of the Advisory Committee on Immunization Practices (ACIP), 2009. MMWR Recomm Rep 2009; 58 (RR-8): 1–52
Centers for Disease Control and Prevention. Seasonal influenza vaccination coverage among children aged 6 months-18 years: eight immunization information system sentinel sites, United States, 2009–10 influenza season. MMWR Morb Mortal Wkly Rep 2010; 59(39): 1266–9
Mereckiene J, Cotter S, Nicoll A, et al. National seasonal influenza vaccination survey in Europe, 2008. Euro Surveill 2008; 13(43): 19017
UK Department of Health. JCVI statement on seasonal influenza vaccination of 30 December 2010 [online]. Available from URL: http://www.dh.gov.uk/prod_consum_dh/groups/dh_digitalassets/@dh/@ab/documents/digitalasset/dh_123209.pdf [Accessed 2012 Jun 13]
Monto AS, Koopman JS, Longini Jr IM. Tecumseh study of illness: XIII. Influenza infection and disease, 1976–1981. Am J Epidemiol 1985; 121(6): 811–22
Mossong J, Hens N, Jit M, et al. Social contacts and mixing patterns relevant to the spread of infectious diseases. PLoS Med 2008; 5(3): e74
Loughlin J, Poulios N, Napalkov P, et al. A study of influenza and influenza-related complications among children in a large US health insurance plan database. Pharmacoeconomics 2003; 21(4): 273–83
Bhat N, Wright JG, Broder KR, et al. Influenza-associated deaths among children in the United States, 2003–2004. N Engl J Med 2005; 353(24): 2559–67
Thompson WW, Shay DK, Weintraub E, et al. Influenza-associated hospitalizations in the United States. JAMA 2004; 292(11): 1333–40
Newall AT, Scuffham PA. Influenza-related disease: the cost to the Australian healthcare system. Vaccine 2008; 26(52): 6818–23
Thompson WW, Weintraub E, Dhankhar P, et al. Estimates of US influenza-associated deaths made using four different methods. Influenza Other Respi Viruses 2009; 3(1): 37–49
Savidan E, Chevat C, Marsh G. Economic evidence of influenza vaccination in children. Health Policy 2008; 86(2–3): 142–52
Glezen WP. Herd protection against influenza. J Clin Virol 2006; 37(4): 237–43
Loeb M, Russell ML, Moss L, et al. Effect of influenza vaccination of children on infection rates in Hutterite communities: a randomized trial. JAMA 2010; 303(10): 943–50
Reichert TA, Sugaya N, Fedson DS, et al. The Japanese experience with vaccinating schoolchildren against influenza. N Engl J Med 2001; 344(12): 889–96
Kelly H, Newall AT. Mortality benefits of influenza vaccination in elderly people. Lancet Infect Dis 2008; 8(8): 462–3
Simonsen L, Taylor RJ, Viboud C, et al. Mortality benefits of influenza vaccination in elderly people: an ongoing controversy. Lancet Infect Dis 2007; 7(10): 658–66
Jefferson T, Di Pietrantonj C, Rivetti A, et al. Vaccines for preventing influenza in healthy adults. Cochrane Database Syst Rev 2010; 7: CD001269
Belshe RB, Edwards KM, Vesikari T, et al. Live attenuated versus inactivated influenza vaccine in infants and young children. N Engl J Med 2007; 356(7): 685–96
Ambrose CS, Levin MJ, Belshe RB. The relative efficacy of trivalent live attenuated and inactivated influenza vaccines in children and adults. Influenza Other Respi Viruses 2011; 5(2): 67–75
Ashkenazi S, Vertruyen A, Aristegui J, et al. Superior relative efficacy of live attenuated influenza vaccine compared with inactivated influenza vaccine in young children with recurrent respiratory tract infections. Pediatr Infect Dis J 2006; 25(10): 870–9
Fleming DM, Crovari P, Wahn U, et al. Comparison of the efficacy and safety of live attenuated cold-adapted influenza vaccine, trivalent, with trivalent inactivated influenza virus vaccine in children and adolescents with asthma. Pediatr Infect Dis J 2006; 25(10): 860–9
Esposito S, Principi N. The rational use of influenza vaccines in healthy children and children with underlying conditions. Curr Opin Infect Dis 2009; 22(3): 244–9
European Medicines Agency. Fluenz influenza vaccine (live attenuated, nasal) [online]. Available from URL: http://www.ema.europa.eu/docs/en_GB/document_library/EPAR_-_Summary_for_the_public/human/001101/WC500103712.pdf [Accessed 2012 Jun 13]
Riddiough MA, Sisk JE, Bell JC. Influenza vaccination: cost-effectiveness and public policy. JAMA 1983; 249(23): 3189–95
White T, Lavoie S, Nettleman MD. Potential cost savings attributable to influenza vaccination of school-aged children. Pediatrics 1999; 103(6): e73
Cohen GM, Nettleman MD. Economic impact of influenza vaccination in preschool children. Pediatrics 2000; 106(5): 973–6
Dayan GH, Nguyen VH, Debbag R, et al. Cost-effectiveness of influenza vaccination in high-risk children in Argentina. Vaccine 2001; 19(30): 4204–13
Fitzner KA, Shortridge KF, McGhee SM, et al. Cost-effectiveness study on influenza prevention in Hong Kong. Health Policy 2001; 56(3): 215–34
Luce BR, Zangwill KM, Palmer CS, et al. Cost-effectiveness analysis of an intranasal influenza vaccine for the prevention of influenza in healthy children. Pediatrics 2001; 108(2): E24
Turner D, Wailoo A, Nicholson K, et al. Systematic review and economic decision modelling for the prevention and treatment of influenza A and B. Health Technol Assess 2003; 7(35): 1–170
Hall JL, Katz BZ. Cost of influenza hospitalization at a tertiary care children’s hospital and its impact on the cost-benefit analysis of the recommendation for universal influenza immunization in children age 6 to 23 months. J Pediatr 2005; 147(6): 807–11
Meltzer MI, Neuzil KM, Griffin MR, et al. An economic analysis of annual influenza vaccination of children. Vaccine 2005; 23(8): 1004–14
Weycker D, Edelsberg J, Halloran ME, et al. Populationwide benefits of routine vaccination of children against influenza. Vaccine 2005; 23(10): 1284–93
Esposito S, Marchisio P, Bosis S, et al. Clinical and economic impact of influenza vaccination on healthy children aged 2–5 years. Vaccine 2006; 24(5): 629–35
Prosser LA, Bridges CB, Uyeki TM, et al. Health benefits, risks, and cost-effectiveness of influenza vaccination of children. Emerg Infect Dis 2006; 12(10): 1548–58
Salo H, Kilpi T, Sintonen H, et al. Cost-effectiveness of influenza vaccination of healthy children. Vaccine 2006; 24(23): 4934–41
Skowronski DM, Woolcott JC, Tweed SA, et al. Potential cost-effectiveness of annual influenza immunization for infants and toddlers: experience from Canada. Vaccine 2006; 24(19): 4222–32
Pisu M, Meltzer MI, Hurwitz ES, et al. Household-based costs and benefits of vaccinating healthy children in daycare against influenza virus: results from a pilot study. Pharmacoeconomics 2005; 23(1): 55–67
Hibbert CL, Piedra PA, McLaurin KK, et al. Cost-effectiveness of live-attenuated influenza vaccine, trivalent in preventing influenza in young children attending daycare centres. Vaccine 2007; 25(47): 8010–20
Marchetti M, Kühnel UM, Colombo GL, et al. Cost-effectiveness of adjuvanted influenza vaccination of healthy children 6 to 60 months of age. Hum Vaccin 2007; 3(1): 14–22
Navas E, Salleras L, Domínguez A, et al. Cost-effectiveness analysis of inactivated virosomal subunit influenza vaccination in children aged 3–14 years from the provider and societal perspectives. Vaccine 2007; 25(16): 3233–9
Luce BR, Nichol KL, Belshe RB, et al. Cost-effectiveness of live attenuated influenza vaccine versus inactivated influenza vaccine among children aged 24–59 months in the United States. Vaccine 2008; 26(23): 2841–8
Schmier J, Li S, King Jr JC, et al. Benefits and costs of immunizing children against influenza at school: an economic analysis based on a large-cluster controlled clinical trial. Health Affairs 2008; 27(2): w96–104
Salleras L, Navas E, Domínguez A, et al. Economic benefits for the family of inactivated subunit virosomal influenza vaccination of healthy children aged 3–14 years during the annual health examination in private paediatric offices. Vaccine 2009; 27(25–26): 3454–8
Jefferson T, Rivetti A, Harnden A, et al. Vaccines for preventing influenza in healthy children. Cochrane Database Syst Rev 2008; 2: CD004879
Newall AT, Kelly H, Harsley S, et al. Cost effectiveness of influenza vaccination in older adults: a critical review of economic evaluations for the 50- to 64-year age group. Pharmacoeconomics 2009; 27(6): 439–50
Stephenson I, Nicholson KG. Influenza: vaccination and treatment. Eur Respir J 2001; 17(6): 1282–93
Navarro-Mari JM, Pérez-Ruiz M, Cantudo-Munoz P, et al. Influenza-like illness criteria were poorly related to laboratory-confirmed influenza in a sentinel surveillance study. J Clin Epidemiol 2005; 58(3): 275–9
Fujieda M, Maeda A, Kondo K, et al. Influenza vaccine effectiveness and confounding factors among young children. Vaccine 2008; 26(50): 6481–5
Keren R, Zaoutis TE, Saddlemire S, et al. Direct medical cost of influenza-related hospitalizations in children. Pediatrics 2006; 118(5): e1321–7
Lambert SB, Allen KM, Carter RC, et al. The cost of community-managed viral respiratory illnesses in a cohort of healthy preschool-aged children. Respir Res 2008; 9: 11
Kim SY, Goldie SJ. Cost-effectiveness analyses of vaccination programmes: a focused review of modelling approaches. Pharmacoeconomics 2008; 26(3): 191–215
Halloran ME, Longini IM, Cowart DM, et al. Community interventions and the epidemic prevention potential. Vaccine 2002; 20(27–28): 3254–62
Basta NE, Chao DL, Halloran ME, et al. Strategies for pandemic and seasonal influenza vaccination of schoolchildren in the United States. Am J Epidemiol 2009; 170(6): 679–86
Vynnycky E, Pitman R, Siddiqui R, et al. Estimating the impact of childhood influenza vaccination programmes in England and Wales. Vaccine 2008; 26(41): 5321–30
Clemens J, Shin S, Ali M. New approaches to the assessment of vaccine herd protection in clinical trials. Lancet Infect Dis 2011; 11(6): 482–7
Hens N, Goeyvaerts N, Aerts M, et al. Mining social mixing patterns for infectious disease models based on a two-day population survey in Belgium. BMC Infectious Diseases 2009; 9: 5
Goeyvaerts N, Hens N, Ogunjimi B, et al. Estimating infectious disease parameters from data on social contacts and serological status. J Royal Stat Soc C-App 2010; 59(2): 255–77
Ogunjimi B, Hens N, Goeyvaerts N, et al. Using empirical social contact data to model person to person infectious disease transmission: an illustration for varicella. Math Biosci 2009; 218(2): 80–7
Bilcke J, Beutels P, Brisson M, et al. Accounting for methodological, structural, and parameter uncertainty in decision-analytic models: a practical guide. Med Decis Making 2011; 31(4): 675–92
Jit M, Brisson M. Modelling the epidemiology of infectious diseases for decision analysis: a primer. Pharmacoeconomics 2011; 29(5): 371–86
Carrat F, Flahault A. Influenza vaccine: the challenge of antigenic drift. Vaccine 2007; 25(39–40): 6852–62
Smith RD, Sach TH. Contingent valuation: what needs to be done? Health Econ Policy Law 2010; 5(1): 91–111
Polsky D, Willke RJ, Scott K, et al. Theory versus practice: a review of ‘willingness-to-pay’ in health and health care. Health Econ 2001; 10(1): 39–52
National Institute for Health and Clinical Excellence. Guide to the methods of technology appraisal. London: NICE, 2008
Canadian Agency for Drugs and Technologies in Health. Guidelines for the economic evaluation of health technologies. Ottawa (ON): CADTH, 2006
Knies S, Severens JL, Ament AJHA, et al. The transferability of valuing lost productivity across jurisdictions: differences between national pharmacoeconomic guidelines. Value Health 2010; 13(5): 519–27
Drummond M, Sculpher MJ, Torrance GW, et al. Methods for the economic evaluation of health care programmes. 3rd rev. ed. Oxford: Oxford University Press, 2005
Griebsch I, Coast J, Brown J. Quality-adjusted life-years lack quality in pediatric care: a critical review of published cost-utility studies in child health. Pediatrics 2005; 115(5): e600–14
Brouwer WBF, Koopmanschap MA, Rutten FFH. Productivity costs measurement through quality of life? A response to the recommendation of the Washington Panel. Health Econ 1997; 6(3): 253–9
Tarn TY, Smith MD. Pharmacoeconomic guidelines around the world. ISPOR Connections 2004; 10(4): 5
Newall AT, Viboud C, Wood JG. Influenza-attributable mortality in Australians aged more than 50 years: a comparison of different modelling approaches. Epidemiol Infect 2010; 138(6): 836–42
Influenza vaccines. Wkly Epidemiol Rec 2005; 80(33): 279–87
Hoskins TW, Davies JR, Allchin A. Controlled trial of inactivated influenza vaccine containing the A/Hong Kong strain during an outbreak of influenza due to the A/England/42/72 strain. Lancet 1973; 2(7821): 116–20
Briscoe JH. The protective effect of influenza vaccine in a mixed influenza A and B epidemic in a boys’ boarding school. J R Coll Gen Pract 1977; 27(166): 28–31
Claxton K, Sculpher M, McCabe C, et al. Probabilistic sensitivity analysis for NICE technology assessment: not an optional extra. Health Econ 2005; 14(4): 339–47
Neuzil KM, Zhu Y, Griffin MR, et al. Burden of interpandemic influenza in children younger than 5 years: a 25-year prospective study. J Infect Dis 2002; 185(2): 147–52
Newall AT, Wood JG, Oudin N, et al. Cost-effectiveness of pharmaceutical-based pandemic influenza mitigation strategies. Emerg Infect Dis 2010; 16(2): 224–30
Baguelin M, Hoek AJV, Jit M, et al. Vaccination against pandemic influenza A/H1N1v in England: a real-time economic evaluation. Vaccine 2010; 28(12): 2370–84
Gojovic MZ, Sander B, Fisman D, et al. Modelling mitigation strategies for pandemic (H1N1) 2009. CMAJ 2009; 181(10): 673–80
Lee BY, Brown ST, Korch GW, et al. A computer simulation of vaccine prioritization, allocation, and rationing during the 2009 H1N1 influenza pandemic. Vaccine 2010; 28(31): 4875–9
Acknowledgements
ATN holds a National Health and Medical Research Council (NHMRC) Training Fellowship (no. 630724; Australian-based Public Health Fellowship). PB is supported by ‘SIMID’ (Simulation Models of Infectious Disease Transmission and Control Processes), a project funded by the Flemish Government Agency for Innovation by Science and Technology (IWT).
ATN has in the past received research funding for other previous projects from a manufacturer of the influenza vaccine, GlaxoSmithKline Pty Ltd. MJ and PB have no conflicts to declare.
ATN led the project and conducted the literature review. PB initiated the idea for the review. ATN and MJ assembled the tables in consultation with PB. All authors contributed to the study design, the analysis and interpretation of the literature, and the drafting of the manuscript. ATN acts as the guarantor for the content of this paper.
This paper is part of a theme issue co-edited by Lisa Prosser, University of Michigan, USA, and no external funding was used to support the publication of this theme issue.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Newall, A.T., Jit, M. & Beutels, P. Economic Evaluations of Childhood Influenza Vaccination. PharmacoEconomics 30, 647–660 (2012). https://doi.org/10.2165/11599130-000000000-00000
Published:
Issue Date:
DOI: https://doi.org/10.2165/11599130-000000000-00000