Abstract
Background: In Japan, when pharmaceutical companies launch a new drug, they are obligated to conduct a post-marketing survey to evaluate the safety and efficacy of the drug in accordance with Good Post-Marketing Surveillance Practice under Article 14.4 (re-examination) of the Pharmaceutical Affairs Law at contracted medical institutions. We report the results of a drug use survey, which we conducted as a post-marketing survey.
Objective: This prospective post-marketing drug use survey was conducted to assess the safety and efficacy of the β-adrenergic receptor antagonist (β-blocker) Artist® Tablets (carvedilol) in patients with hypertension in Japan.
Patients: Patients were carvedilol-naive and had essential hypertension or renal parenchymal hypertension.
Methods: This was a prospective survey conducted over 3 years from October 1993 to September 1996. The standard observation period for the patients was defined as 12 weeks of treatment with carvedilol.
Results: We collected data on 4961 patients at 561 medical institutions who had not been previously treated with carvedilol; 4574 patients were included in the safety analysis and 4422 in the efficacy analysis. The incidence of adverse drug reactions (the proportion of patients with adverse drug reactions) was 4.31% (197 of 4574 patients), which is less than that shown in the pre-approval clinical trial of carvedilol (6.85%[68 of 993]). The most common adverse drug reactions were bradycardia, dizziness, hypotension, headache, and feeling light-headed.
After 12 weeks’ treatment with carvedilol, systolic/diastolic blood pressure (SBP/DBP) was reduced from 168.2 ± 18.6/95.7 ± 11.3mmHg at baseline to 144.3 ± 17.3/83.4 ± 10.8mmHg. Patients were classified according to which antihypertensive drug they had been using when carvedilol treatment was initiated. Coadministered agents were calcium channel blockers (CCBs), angiotensinconverting enzyme inhibitors (ACEIs), diuretics, and a-adrenergic receptor antagonists (α-blockers). At 12 weeks, the change in SBP/DBP in the monotherapy group was −22.7/−12.2mmHg and that of each combination therapy subgroup, CCB, ACEI, diuretic, and b-blocker, was −26.1/−12.7mmHg, −25.4/−11.9mmHg, −26.3/−13.0mmHg, and −24.4/−11.5mmHg, respectively. The achievement rates for target BP (<140/90mmHg) were 29.5% in the monotherapy group, 34.8% in the CCB group, 31.3% in the ACEI group, 31.8% in the diuretic group, and 32.4% in the β-blocker group. There was no significant difference in the achievement of target BP among the four combination therapy subgroups (p = 0.475). These results indicate that carvedilol exerts reasonable BP reduction regardless of whether it is used as monotherapy or in combination therapy, and that the effect is not influenced by the coadministered drug. Moreover, carvedilol was also effective in reducing BP levels in elderly patients (≥65 years) and in patients with diabetes mellitus or renal diseases.
Conclusions: The results of this study reflect the results of clinical trials up to the time of approval and it was confirmed that carvedilol is a highly useful drug in the treatment of hypertension.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
For the management of hypertension, risk stratification should be based on the presence or absence of risk factors other than blood pressure (BP), such as hypertensive organ damage or cardiovascular disease. If needed, an antihypertensive drug may be initiated to achieve BP goal. If hypertension is complicated with risk factors, such as diabetes mellitus, target organ damage, or renal dysfunction, aggressive management of hypertension is important to attain target BP goals as defined in the Japanese Society of Hypertension Guidelines for the Management of Hypertension (JSH 2004).[1] However, it is difficult to achieve target BP goals with a single antihypertensive drug and often combined administration of two or more drugs is required.
Currently available antihypertensive drugs in Japan include calcium channel blockers (CCBs), angiotensin-converting enzyme inhibitors (ACEIs), angiotensin II receptor blockers (ARBs), diuretics, β-adrenergic receptor antagonists (β-blockers), and α-adrenergic receptor antagonists (α-blockers). Most antihypertensive drugs have been demonstrated to have not only an antihypertensive effect, but also cerebrovascular/cardiovascular protective effects. Based on results of large-scale clinical studies, several guidelines[1–4] recommend that depending on their pharmacologic properties, some classes of antihypertensive drugs should be aggressively used and some should be contraindicated in patients with compelling indications such as established cardiovascular disease, diabetes, chronic kidney disease, or recurrent stroke. Regarding combined administration of two or more drugs, in order to select the best antihypertensive drugs for each patient, guidelines[1–4] recommend suitable combinations based on best evidence. These combinations are expected to provide additive or synergistic effects; however, the recommendations differ between the various guidelines.
β-Blockers are aggressively indicated for the treatment of hypertension associated with angina pectoris, myocardial infarction, tachycardia, and/or heart failure, and are recommended for the prevention of recurrence of myocardial infarction or occurrence of ischemic heart disease, and to improve prognosis in patients with heart failure. For cardioprotection and strict control of BP in patients with these risks, the use of β-blockers is of great significance. However, the blockade of β-receptors can induce adverse effects such as increased peripheral vascular resistance, decreased local circulation, excessive impairment of cardiac function, coronary vasospasm, and bronchoconstriction. However, most β-blockers are less likely to be used than antihypertensive drugs that are associated with a lower incidence of adverse drug reactions (ADRs), such as CCBs, ACEIs, and ARBs, because of concern of adverse effects on glucose/lipid metabolism.
Carvedilol, with an improved ADR profile, was synthesized by Boehringer-Mannheim (currently, Hoffmann-La Roche, Basel, Switzerland), and clinically developed and launched in Japan by Daiichi Pharmaceutical Co., Ltd. (currently, Daiichi Sankyo Co., Ltd., Tokyo, Japan) as a cardiac nonselective β-blocking agent with peripheral vasodilatation (mainly based on α1-blocking action).[5] Clinical studies have demonstrated that carvedilol has a long-lasting antihypertensive effect that allows once-daily administration without adversely affecting glucose/lipid metabolism, and has favorable efficacy when used alone or in combination with other drugs.[6–14] Carvedilol is the only β-blocker indicated for the treatment of chronic heart failure in Japan. Based on accumulated evidence in the treatment of chronic heart failure,[15–19] carvedilol has received a certain level of positive evaluation in Japan and other countries.[20,21] However, there have been no reports on the antihypertensive efficacy or safety of carvedilol when being used in many hypertensive patients in daily clinical practice in Japan. In particular, no large-scale study had been conducted to investigate whether β-blockers could aggravate glucose metabolism, or not, in Japanese patients with diabetes. In addition, it is known that elderly individuals generally respond less well to β-blockers because of their lower renin activity.
This prospective survey, conducted between October 1993 and September 1996, sought to assess the use of carvedilol in patients with hypertension in Japan. This report will also address the efficacy and safety of carvedilol alone and in combination with other drugs, in elderly patients and in high-risk patients with diabetes or renal disease, conditions that are more likely to be found in elderly individuals.
Patients and Methods
Patients
This survey was conducted in accordance with Good Post-Marketing Surveillance Practice[22] under Article 14.4 (re-examination) of the Pharmaceutical Affairs Law at contracted medical institutions. Patients were carvedilol-naive and had essential hypertension or renal parenchymal hypertension. After a contract was concluded at the medical institution, patients with these diseases who had not been previously treated with carvedilol and who received carvedilol during the observation period were investigated consecutively.
Dosage and Administration
Carvedilol was administered at the discretion of physicians participating in the survey, and was prescribed according to the dosage and administration in the package insert; the usual adult dosage for oral use is carvedilol 10-20 mg once daily. The dosage could be adjusted according to each patient’s age and symptoms. Neither prior treatment nor combination drugs were restricted. The standard observation period was 12 weeks, during which time patients were treated with carvedilol. If patients dropped out or withdrew from the survey, they were followed-up until that time.
Assessments
Patient Demographics
Data collected included patient initials, medical record number, date of birth, sex (pregnancy status for women), in- or outpatient status, diagnosis (target disease), severity (the WHO classification), duration of disease, presence/absence of complications, previous medical history, history of allergy, family history of hypertension, previous use of antihypertensive medications before the initiation of carvedilol, and concomitant use of other antihypertensive medications.
Carvedilol Dosage and Administration
The duration of carvedilol treatment and daily dose were recorded.
Clinical Observations
Data on systolic blood pressure (SBP)/diastolic blood pressure (DBP) and pulse rate were collected.
Laboratory Analyses
The laboratory analyses included hematology, blood chemistry, and urinalysis.
Adverse Drug Reactions
The name, severity, progress, medication taken for an ADR, outcome, drug-event relationship, and suspected concomitant medication were recorded for all ADRs.
Diseases that Developed During the Course of Carvedilol Treatment
The name and progression of diseases that developed during the course of carvedilol treatment were recorded.
Data Handling and Collection/Analytical Procedures
The safety population comprised patients who completed a case report form. Excluded were those who (i) received carvedilol during periods other than the survey period; (ii) started the drug before a contract was concluded; (iii) provided two case report forms; (iv) did not revisit the medical institutions after the initial visit; and (v) were not evaluated for ADRs.
The efficacy population comprised patients from the safety population and excluded patients (i) with unknown target disease or who used carvedilol for the treatment of a condition other than the target disease; and (ii) who were not evaluated or could not be evaluated for efficacy.
Assessment of efficacy was performed by each physician. The antihypertensive effect of carvedilol was assessed according to the following four criteria: ‘decreased’, ‘tended to be decreased’, ‘unchanged’, and ‘increased’.
The demographic data of the patients and the incidence of ADRs (the proportion of the patients with ADRs) in the safety population were analyzed using Fisher’s direct probability method. Changes from baseline in SBP/DBP and pulse rate were analyzed at week 12 using paired t-test and at weeks 2, 4, 6, 8, 10, and 12 according to Dunnett’s multiple comparison test. In the physicians’ assessment of efficacy, a 95% confidence interval was calculated for decrease in BP. All statistical tests were performed using a two-sided 5% significance level. The figures are presented as mean ± standard deviation (SD).
The observed ADRs were classified using preferred terms by each System Organ Class according to the 1996 version of the Japanese Adverse Drug Reaction Terminology.
Results
Patient Number and Disposition
Case report forms were collected from 4961 patients at 561 medical institutions throughout Japan. Among the total 4961 patients, 81 received carvedilol during periods other than the survey period, 162 had started the drug before a contract was concluded, 56 provided two case report forms, 85 did not revisit the medical institute after the initial visit, and three were not evaluated for ADRs; these 387 patients were excluded from the safety analyses. The remaining 4574 patients were included in the safety population. Among the safety population, five had unknown target disease or used carvedilol for a condition other than the target disease (renovascular hypertension), and 147 were not evaluated or could not be evaluated for efficacy; these 152 patients were excluded from the efficacy analyses. The remaining 4422 patients were included in the efficacy population. Patient disposition is shown in figure 1.
Patient Demographics
The demographic characteristics of patients comprising the safety population are presented in table I. The safety population had nearly equal numbers of males and females. Elderly patients aged ≥65 years accounted for 38.4% (1757 patients), including 579 advanced elderly patients aged ≥75 years (12.7%). The majority of the safety population were patients with essential hypertension (97.7%; n = 4468), and those with renal parenchymal hypertension accounted for 2.2% (101 patients). The severity of hypertension was graded as follows: 2713 patients (59.3%) had WHO grade I, 1037 (22.7%) grade II, and 586 (12.8%) grade III. Heart failure was found as a co-existing condition of hypertension in the largest number of the safety population (853 patients [18.7%]), followed by hepatic disease (536 patients [11.7%]), diabetes (500 patients [10.9%]), and renal disease (289 patients [6.3%]). During the survey, 2039 patients (44.6%) initiated carvedilol treatment at a dose of 10 mg/day and 2509 patients (54.9%) with 20 mg/day. During the carvedilol treatment period, a total of 2293 patients (50.1%) concomitantly used other antihypertensive medications; CCBs were the most commonly used by 1698 patients (37.1%).
Safety
Adverse Drug Reactions
Table II provides a list of patient-reported ADRs. Among the 4574 patients who comprised the safety population, the overall incidence of ADRs was 4.31% (197 of 4574), which was lower than the reported 6.85% (68 of 993 patients with essential hypertension or renal parenchymal hypertension) for the approval of carvedilol. The most common ADR (preferred terms) was bradycardia (24 events, 0.52%), followed by dizziness (19 events, 0.42%), hypotension (15 events, 0.33%), and headache and light-headed feeling (nine events each, 0.20%). Four patients had five ADRs that were judged to be serious by their physicians – one event each of consciousness loss, cardiac failure, blood pressure decreased, status asthmaticus, and erection decreased (all are preferred terms).
Adverse Drug Reactions by Demographic Factors
Table III presents ADRs stratified by selected demographic factors. A significant difference in the incidence rate of ADRs between strata was found for age, severity (WHO classification), presence/absence of complications (renal disease), previous use of antihypertensive medications before the initiation of carvedilol, total number of days of carvedilol treatment, and concomitant use of other antihypertensive medications, as summarized here.
Age
The incidence rate in elderly patients (≥65 years) was 5.18% (91 of 1757 patients), which was significantly higher than 3.76% in non-elderly patients (106 of 2816 patients; p = 0.025). This subgroup had a significantly higher incidence of ‘general cardiovascular disorders’ (p < 0.001) and reported four or more events of the following ADRs (preferred terms): bradycardia (14 events), hypotension (12 events), dizziness (ten events), light-headed feeling (five events), weakness (four events), headache (four events), and cardiothoracic ratio increased (four events).
Severity (WHO Classification)
When stratified by severity (WHO classification), the incidence rate was 3.83% (104 of 2713 patients) for grade I, 3.95% (41 of 1037 patients) for grade II, and 7.68% (45 of 586 patients) for grade III, with a significantly higher incidence rate for grade III (p < 0.001). Patients with grade III had significantly more ‘body as a whole, general disorders’ and ‘general cardiovascular disorders’ (p = 0.010 and p = 0.004, respectively). In this subgroup, three or more events of the following ADRs (preferred terms) were reported: bradycardia (six events), hypotension (five events), dizziness (five events), light-headed feeling (three events), queasy (three events), and cardiothoracic ratio increased (three events).
Complications (Renal Disease)
For patients with complications, the incidence of ADRs was significantly higher than in those without complications (5.29% [137 of 2591] vs 2.88% [54 of 1876]; p < 0.001). When ADRs were stratified by the presence/absence of renal disease complications, a significant difference was seen between patients with renal disease complications (7.61% [22 of 289]) and those without (4.10% [174 of 4244]).[p = 0.010], although no significant difference was observed when stratified by the presence/absence of hepatic disease, cardiac disease, or diabetes. Patients with renal disease complications had significantly higher incidence rates of ADRs – body as a whole, general disorders, central and peripheral nervous system disorders, general cardiovascular disorders, and respiratory system disorders (p = 0.026, p = 0.041, p = 0.006, and p = 0.024, respectively). In this subgroup, ADRs (preferred terms) that occurred at two events or more were light-headed feeling (three events), headache dull (two events), dizziness (two events), hypotension (two events), and cardiothoracic ratio increased (two events).
Previous Use of Antihypertensive Medications
The incidence of ADRs in patients who had used antihypertensive medications before the initiation of carvedilol was 5.38% (133 of 2471 patients), which was significantly higher than the 3.07% (56 of 1822 patients) in patients who had not previously used any antihypertensive medications (p < 0.001). Central and peripheral nervous system disorders and gastrointestinal system disorders were reported significantly more often by patients who had used antihypertensive medications (p = 0.013 and p = 0.049, respectively). There was no significant difference in the incidence rate of general cardiovascular disorders (p = 0.241). Five or more events of the following ADRs (preferred terms) were reported in this subgroup: bradycardia (15 events), dizziness (14 events), hypotension (11 events), headache (eight events), queasy (seven events), headache dull (five events), and light-headed feeling (five events).
Total Number of Days of Carvedilol Treatment
The incidence rate of ADRs in the stratum of ‘<1 month’ for total number of days of carvedilol treatment was 32.68% (83 of 254 patients), significantly higher than 2.64% (114 of 4316 patients) in the stratum of ‘≥1 month’ (p < 0.001). There were significantly more body as a whole, general disorders (p < 0.001); skin and appendages disorders (p = 0.011); central and peripheral nervous system disorders (p < 0.001); psychiatric disorders (p = 0.017); gastrointestinal system disorders (p < 0.001); general cardiovascular disorders (p < 0.001); heart rate and rhythm disorders (p < 0.001); and respiratory system disorders (p < 0.001) in the stratum of ‘<1 month’. ADRs (preferred terms) that were observed at five or more events in this stratum were dizziness (ten events), hypotension (ten events), bradycardia (nine events), queasy (six events), and light-headed feeling (five events).
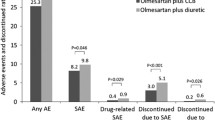
Concomitant Use of Other Antihypertensive Medications
For patients that concomitantly used other antihypertensive medications, the incidence of ADRs was 4.93% (113 of 2293 patients), significantly higher than that reported in the cohort that did not concomitantly use other antihypertensive agents (3.68% [84 of 2280 patients]).[p = 0.041]. The incidence of heart rate and rhythm disorders was significantly higher in patients with concomitant use (p = 0.019), who reported five or more events of the following ADRs: bradycardia (13 events), dizziness (12 events), hypotension (11 events), queasy (six events), light-headed feeling (five events), and GPT increased (five events).[all are preferred terms].
Changes in Laboratory Parameters
Table IV shows the mean changes from baseline in hematologic and blood chemical parameters in patients who underwent laboratory tests before and after the initiation of carvedilol treatment. Mean changes from baseline were small for all the laboratory parameters, including glucose and lipid metabolic-related parameters, without inducing clinically relevant problems.
Efficacy
Changes in Blood Pressure and Pulse Rate
Figure 2 shows changes in BP and pulse rate from baseline to week 12 for those patients among the efficacy population of 4422 for whom these measurements were taken. BP and pulse rate were significantly reduced from baseline at week 2 and continued to gradually reduce until week 12 (p < 0.001 for both).
Changes in BP and pulse rate from baseline are summarized in table V for patients who (i) had these measurements taken before and after the initiation of carvedilol treatment (all patients); (ii) had not previously used antihypertensive medications at the time of initiation of carvedilol treatment (carvedilol alone); and (iii) had previously used antihypertensive medications (concomitant use of CCBs, concomitant use of ACEIs, concomitant use of diuretics, concomitant use of α-blockers) at initiation of carvedilol treatment.
Respective mean SBP and DBP for the total efficacy population were 168.2 ± 18.6 mmHg and 95.7 ± 11.3 mmHg at baseline; these were reduced to 144.3 ± 17.3 mmHg and 83.4 ± 10.8 mmHg at week 12. Mean change value from baseline to week 12 (the value at week 12 subtracted by the baseline value) was −23.9 ± 20.3 mmHg for SBP and −12.3 ± 12.4 mmHg for DBP, indicating a significant reduction (p < 0.001 for both). Mean pulse rate in all patients was 76.2 ± 12.6 beats per minute (beats/min) at baseline and 69.7 ± 8.8 beats/min at week 12. The mean change value was −6.6 ± 11.2 beats/min, indicating a significant decrease from baseline to week 12 (p < 0.001). Respective mean change values from baseline to week 12 for SBP and DBP were −22.7 ± 18.8 mmHg and −12.2 ± 12.2 mmHg in patients treated with carvedilol alone; −26.1 ± 22.4 mmHg and −12.7 ± 13.1 mmHg in patients who received concomitant CCBs; −25.4 ± 23.3 mmHg and −11.9 ± 13.0 mmHg in those who received ACEIs; −26.3 ± 22.0 mmHg and −13.0 ± 13.3 mmHg in the patients who received diuretics; and −24.4 ± 21.0 mmHg and −11.5 ± 11.1 mmHg in patients who received α-blockers, demonstrating a significant difference in SBP/DBP between baseline and week 12 in all strata (p < 0.001 for all). No significant difference in the change value for SBP or DBP was seen for the cohort that had previously used antihypertensive drugs (p = 0.836 for SBP; p = 0.515 for DBP). Therefore, carvedilol had similar clinical efficacy when used alone or in combination with other antihypertensive medications.
Assessment of Efficacy
The results of the physicians’ assessment of efficacy (based on an antihypertensive effect of carvedilol) are presented in table VI. Among the 4422 patients in the efficacy population, 58.1% (2571 of 4422 patients) were judged as ‘decreased’ and 84.8% (3748 of 4422 patients) as ‘decreased’ or ‘tended to be decreased’.
Achievement Rate of Target Blood Pressure
Figure 3 illustrates achievement of target BP at week 12. For the target BP of 140/90 mmHg, the achievement rate at week 12 after the initiation of carvedilol was 31.3% for all patients, 29.5% for those treated with carvedilol alone, 34.8% for those with concomitant CCBs, 31.3% with ACEIs, 31.8% with diuretics, and 32.4% for those with α-blockers. For comparison, the achievement rate in the efficacy population before the initiation of carvedilol had been 3.0%. There was no significant difference in the achievement rate between the antihypertensive medications previously used (p = 0.475). For the intermediate target BP (150/90 mmHg) at the start of the survey, the achievement rate at week 12 was 53.0% for all patients, 52.2% for those with carvedilol alone, 55.9% for those with CCBs, 46.3% for those with ACEIs, 55.8% for those with diuretics, and 44.1% for those with α-blockers.
Review of Elderly Patients, those with Diabetes Mellitus or Renal Disease
Changes in Blood Pressure and Pulse Rate
Table VII shows changes in BP and pulse rate from baseline to week 12 in elderly patients (aged ≥65 years), and those with diabetes complications or renal disease complications among the efficacy population. The respective values of SBP and DBP were reduced from 171.5 ± 19.1 mmHg and 92.1 ± 11.4 mmHg at baseline to 145.5 ± 18.5 mmHg and 80.2 ± 10.7 mmHg at week 12 in the elderly group; from 171.0 ± 18.7 mmHg and 93.7 ± 12.4 mmHg at baseline to 147.4 ± 20.0 mmHg and 82.8 ± 11.1 mmHg at week 12 in those with diabetes complications; and from 173.7 ± 22.5 mmHg and 93.9 ± 13.0 mmHg at baseline to 146.5 ± 20.0 mmHg and 82.6 ± 11.3 mmHg at week 12 in those with renal disease complications. There was a significant reduction in all the subgroups (p < 0.001 for all).
Changes in Fasting Blood Glucose in Patients withDiabetes and in Creatinine in Those with RenalDisease
Figure 4 illustrates changes from baseline to week 12 in fasting blood glucose in patients with diabetes complications and in creatinine levels in those with renal disease complications in the 4574 patients in the safety population. The fasting blood glucose level in patients with diabetes complications was 163.4 ± 64.7 mg/dL at baseline and this was reduced to 148.5 ± 54.1 mg/dL at week 12. The creatinine level in those with renal disease complications was 3.28 ± 3.83 mg/dL at baseline, which was changed to 3.54 ± 4.24 mg/dL at week 12.
Discussion
The mechanism of antihypertensive action of β-blockers has not been established. The possible main mechanisms may be linked to a decrease in cardiac output, a reduction in the production/release of renin in the kidney, and a reduction in the release of sympathomimetic substances from the CNS. A reduction in the release of sympathomimetic substances by β-blockers has been demonstrated to play a role in the primary and secondary prevention of cardiovascular events through several mechanisms,[23,24] especially for hypertension complicated with ischemic heart disease. In Japan, over 20 types of β-blockers have been used in clinical practice. It has been suggested that β-blockers could have different effects on the long-term prognosis of hypertensive patients depending on their lipophilicity (water solubility), intrinsic sympathomimetic action, membrane-stabilizing action, vasodilation, and any additional actions (e.g. antioxidant), as well as their selectivity at β1 receptors. Hence, it is reasonable to suggest that it would be difficult to categorize these drugs into one group, despite the fact that they are classified as one drug class (i.e. β-blockers). In addition, since β-blockers are contraindicated in some patient groups and are not recommended for elderly patients or those with diabetes, it may be possible that potential target patient populations are excluded from receiving this treatment.
Carvedilol is a nonselective β-blocking cardiac agent. In addition to its potent antioxidant action, it was developed to have an additional α1 antagonist action (a blocking ratio of α : β = 1 : 8) to reduce some of the risks associated with other β-blockers such as increased peripheral vascular resistance, excessively impaired cardiac functions, and adverse effects on glucose/lipid metabolism.[25–28] As expected, in large-scale international clinical studies, the clinical efficacy of carvedilol was demonstrated to be different from that of conventional β-blockers.[14,19] An observational drug use survey in a large number of patients would be of certain significance to interpret whether data from such large-scale clinical studies are applicable in daily medical practice. Therefore, we conducted a prospective surveillance study on the use of carvedilol to confirm its safety and efficacy and gather information about its actual use in Japanese hypertensive patients in daily clinical practice.
We collected data on 4961 patients from 561 medical institutions nationwide; 4574 patients were evaluable for safety and 4422 were for efficacy. The overall incidence rate of ADRs was 4.31% in the survey. The most commonly reported ADRs were 24 events of bradycardia, 19 events of dizziness, 15 events of hypotension, and nine events each of headache and light-headed feeling; all could be linked to the pharmacologic action of carvedilol. The incidence and types of ADRs reported in our survey were similar to those observed in clinical studies conducted prior to approval.
A review of ADRs stratified by selected demographic factors showed a significant difference in the incidence rate of ADRs between strata for age, severity (WHO classification), presence/absence of complications (renal disease), previous use of antihypertensive medications before initiation of carvedilol, total number of days of carvedilol treatment, and concomitant use of other antihypertensive medications.
According to stratification by age, the incidence of ADRs was higher in elderly patients (aged ≥65 years) in whom there was a significantly higher incidence of general cardiovascular disorders (p < 0.001). Organ function generally tends to decline with age, therefore, in elderly patients, carvedilol should be initiated at lower doses because the drug is likely to excessively exhibit its pharmacologic actions when hepatic metabolic capacity is decreased, and because an excessive or rapid decrease in BP can cause ischemic events in important organs such as the heart, kidney, and brain.
A significantly higher incidence of ADRs was seen in the stratum of grade III as stratified by severity (WHO classification) and in that of patients with renal disease complications as stratified by presence/absence of complications (renal disease). Both strata had similar patterns of ADRs, as evidenced by the fact that the incidence rate of whole-body general disorders; general cardiovascular disorders; central and peripheral nervous system disorders; and respiratory system disorders were higher in both strata. The subgroup of patients with renal disease complications included a relatively high proportion of patients with WHO grade III. This could explain the higher incidence of ADRs in patients with WHO grade III; that is, the higher incidence rate in this subgroup could be affected by complications of renal disease. Carvedilol is metabolized in the liver and excreted in feces, but does not seem to be significantly affected by renal function. In patients with severe renal impairment, however, blood drug concentrations are likely to be increased.[29] Hence, carvedilol should be administered with caution to patients with renal disease. In patients with renal disease complications, no ADRs related to renal function (urinary system disorders), such as decreased renal function or albuminuria, were reported during the survey.
Stratification by previous use of antihypertensive medications showed a higher incidence of ADRs in patients with previous use. These patients could be characterized by having a long duration of the disease and multiple organ dysfunction due to their complications. When analyzed by disease duration, the incidence of ADRs tended to be increased with longer duration. Therefore, it would be likely that the higher incidence rate in patients with previous use would be due to the longer duration of the disease.
When analyzed by the total number of days of carvedilol treatment, patients who had received carvedilol for <1 month were found to have a higher incidence rate of ADRs. This may be because they tended to have ADRs during the early period of treatment and discontinued the drug at that time.
When analyzed by concomitant use of other antihypertensive medications, patients who had concomitantly used other antihypertensive medications had a higher incidence of ADRs; the incidence of general cardiovascular disorders was significantly higher (p = 0.019). Among patients who concomitantly used other antihypertensive medications, those who used CCBs accounted for the majority (74.1% [1698 of 2293 patients]). It would be likely that concomitant use of carvedilol with CCBs, especially with CCBs, which have an inhibitory effect on cardiac conduction and can decrease cardiac contractility and heart rate, would enhance each others actions. Carvedilol is cautioned for use with CCBs as indicated in the “Drug Interactions (Precautions for Coadministration)” section in the current package insert (Daiichi Sankyo Co., Ltd., Tokyo, Japan, 2007).
In the efficacy population, mean baseline SBP and DBP values, which were 168.2 ± 18.6 mmHg and 95.7 ± 11.3 mmHg, respectively, were significantly decreased to 144.3 ± 17.3 mmHg and 83.4 ± 10.8 mmHg at week 12. BP was significantly reduced at week 2 and was gradually reduced thereafter until week 12. In patients who received carvedilol alone who had not received any other antihypertensive drugs, respective mean change values for SBP and DBP from baseline to 12 weeks after treatment were −22.7 mmHg and −12.2 mmHg, while for the cohorts that had previously used antihypertensive drugs at initiation of carvedilol treatment, respective mean change values for SBP and DBP ranged from −24.4 to −26.3 mmHg and from −11.5 to −13.0 mmHg; there was no significant difference between patients that received carvedilol alone and those that previously and concomitantly used other antihypertensive agents. Hence, carvedilol was found to exhibit a stable antihypertensive effect when used alone and in combination with other antihypertensive drugs. For the target BP goal (140/90 mmHg) specified in JSH 2004,[1] the achievement rate ranged from 31.3% to 34.8% in the subgroups classified as previous users of antihypertensive agents, and there was no significant difference between the antihypertensive medications previously used. Therefore, carvedilol in any of the combinations achieved the target BP goal in a similar manner, suggesting that the efficacy of this drug is favorable in combination with any other antihypertensive drug. Carvedilol could also be described as being very useful with proven clinical efficacy not only when used as a first-choice treatment for patients who have not received any previous antihypertensive drugs, but also when used as an additional treatment for those who have been receiving another antihypertensive drug. However, this survey was completed before ARBs, which are widely-used antihypertensive drugs, were launched in Japan; hence, further surveys are necessary to investigate the combined effect of carvedilol and ARBs.
In this survey, 31.3% of all patients achieved the BP goal (140/90 mmHg) specified in the JSH 2004.[1] This achievement rate differed from the proportion (58.1%) of patients judged as decreased by their physicians. In contrast, 53.0% of all patients had achieved the tentative goal (150/90 mmHg) around the time of starting the survey; this rate was similar to the proportion of patients who were judged decreased. Therefore, it can be presumed that the physicians attending the survey were satisfied with the antihypertensive effect of carvedilol to some extent.
It is known that in elderly patients, reduced activity of the renin-angiotensin system is seen as one of the age-dependent humoral factors related to BP control and that renin activity is generally low. One of the mechanisms of the antihypertensive action of β-blockers is thought to be blockade of β-receptors in the juxtaglomerular cells, which results in a decrease in release of renin from the kidney. It has been reported that the antihypertensive effect of β-blockers can be reduced in hypertensive patients with low renin activity.[30–33] Therefore, it might be possible that the antihypertensive effect would be reduced in elderly hypertensive patients with low renin activity. In this survey, however, the respective SBP and DBP values in the elderly patients were 171.5 ± 19.1 mmHg and 92.1 ± 11.4 mmHg at baseline, and 145.5 ± 18.5 mmHg and 80.2 ± 10.7 mmHg at the end of treatment; these changes were similar to those seen in the whole study population, which included a high percentage of non-elderly patients (60%). A decrease in the antihypertensive effect of carvedilol was not observed in elderly patients in this survey. Thus, carvedilol was demonstrated to be effective and also of use in elderly hypertensive patients.
In Japanese and overseas guidelines,[1–4] the importance of good BP control has been emphasized especially for hypertensive patients with diabetes and those with renal disease, and a more strict BP goal has been set for such patients. For those with diabetes, blood glucose, as well as BP, has to be strictly controlled and antihypertensive drugs that have no negative impact on glucose metabolism are recommended. Many β-blockers can negatively affect glucose metabolism and it is generally said that caution should be exercised when these drugs are used by patients with diabetes. In the 2007 Guidelines for the Management of Arterial Hypertension (ESH/ESC 2007).[4] the combination of β-blockers with thiazide diuretics is not recommended for patients with a high risk of metabolic syndrome or diabetes. Carvedilol, a vasodilating β-blocker, is more likely to have a small negative effect on glucose metabolism and decrease the initial onset of diabetes as compared with other β-blockers.[34] From the results of the GEMINI (Glycemic Effects in Diabetes Mellitus: Carvedilol-Metoprolol Comparison in Hypertensives) trial, Bakris et al.[14] reported that carvedilol improves insulin sensitivity without any effect on glycated hemoglobin, while controlling BP well. Our survey included 500 patients with diabetes complications in whom the drug was found to have good antihypertensive effect without a significant difference in the incidence rate of ADRs compared with those without diabetes complications. Among reported metabolic and nutritional disorders, the ADRs related to glucose metabolism were only one event each of hyperglycemia, sugar blood level increased,Footnote 1 hypoglycemia, and sugar in the urine1 from three patients. All of these ADRs were observed in patients with diabetes complications, but none were considered serious. Fasting blood glucose levels in patients with diabetes were 163.4 ± 64.7 mg/dL at baseline and 148.5 ± 54.1 mg/dL at the end of treatment, without an adverse change from baseline. Among the 500 patients with diabetes complications, 16 started or additionally took antidiabetic medications during the course of carvedilol treatment, and seven received antidiabetic medications at the initiation of carvedilol treatment but discontinued these medications during carvedilol treatment. Even considering the addition or discontinuation of antidiabetic medications in these 23 patients, carvedilol is not believed to have a negative impact on glucose metabolism. Hence, in this survey, as reported previously, the safety of carvedilol was demonstrated with no adverse effects on glucose metabolism, even in patients with diabetes complications.
For patients with renal disease complications, as for patients with diabetes complications, strict BP control is necessary and first-choice drugs are ACEIs, which have a renal-protective effect, and renin-angiotensin system inhibitors, such as ARBs. If the BP goal is not achieved with these drugs, multidrug therapy will be needed. In this case, β-blockers would be a second or third choice when used in combination, in order to maintain good BP control. In this survey, the respective SBP and DBP values in the patients with renal disease complications were 173.7 ± 22.5 mmHg and 93.9 ± 13.0 mmHg at baseline and were decreased to 146.5 ± 20.0 mmHg and 82.6 ± 11.3 mmHg at week 12, suggesting a good antihypertensive effect of carvedilol, even in this patient subgroup. The creatinine level in patients with renal disease was 3.28 ± 3.83 mg/dL at baseline and 3.54 ± 4.24 mg/dL at the end of treatment. As indicated by the level at baseline, this subgroup of patients had severe renal dysfunction and was being treated in daily clinical practice; thus, the change in creatinine levels seen in this subgroup is not thought to be clinically relevant. Therefore, carvedilol also demonstrated to have a favorable antihypertensive effect in patients with renal disease complications, while not aggravating their renal function.
In conclusion, carvedilol was confirmed to be safe and effective when used in patients with hypertension in daily clinical practice, and was also safely used with a good antihypertensive effect in elderly patients and in those with diabetes or renal disease complications.
Conclusions
We conducted a drug use survey of Artist® tablets (carvedilol) in Japanese patients with hypertension during a period from October 1993 to September 1996. We collected data on 4961 patients from 561 medical institutions nationwide. The drug was investigated for safety in 4574 patients and for efficacy in 4422 patients. The results are summarized in the following five points:
-
1.
The overall incidence rate of ADRs was 4.31% (197 of 4574 patients). The most common ADR was bradycardia, for which 24 events were reported, followed by 19 events of dizziness, 15 events of hypotension, and nine events each of headache and light-headed feeling. These ADRs were linked to the pharmacologic action of the drug. The kinds and patterns of ADRs reported in the survey were similar to those observed in clinical trials that had been performed until the time of approval.
-
2.
As stratified by the selected demographic factors, a significantly higher incidence of ADRs was observed in the following strata: elderly patients (aged ≥65 years), patients with grade III (WHO classification) hypertension, patients with renal disease complications, patients who previously used antihypertensive medications, and patients who concomitantly used other antihypertensive medications.
-
3.
The respective SBP and DBP values were 168.2 ± 18.6 mmHg and 95.7 ± 11.3 mmHg at baseline. These values were significantly reduced at week 2 and were gradually reduced thereafter to 144.3 ± 17.3 mmHg and 83.4 ± 10.8 mmHg, respectively, at week 12.
-
4.
The change value for BP from before to after treatment in patients who received carvedilol alone and in those who had previously used antihypertensive drugs ranged from −22.7 mmHg to −26.3 mmHg for SBP and from −11.5 mmHg to −13.0 mmHg for DBP. In these subgroups, achievement of BP goal (< 140/90 mmHg) ranged from 29.5% to 34.8%. There was no significant difference in BP goal achievement rates (31.3–34.8%) between the concomitantly used antihypertensive drugs.
-
5.
The change values for SBP and DBP between before and after treatment were -26.0 mmHg and -11.9 mmHg in elderly patients (aged ≥65 years), −23.6 mmHg and −10.9 mmHg in those with diabetes complications, and -27.2 mmHg and −11.3 mmHg in those with renal disease complications, demonstrating a good antihypertensive effect of carvedilol in these populations. Carvedilol did not adversely affect glucose metabolism in patients with diabetes complications, or renal function in those with renal disease complications.
The results of this prospective surveillance study on the use of carvedilol in patients with hypertension closely reflect data that have been collected for the approval of the drug. It can be concluded that carvedilol can be safely and effectively used for the treatment of hypertension.
Notes
Observed in the same patient.
References
The Japanese Society of Hypertension & Guidelines Subcommittee of Japanese Society of Hypertension. 2004 guidelines for the management of hypertension [in Japanese]. Life Science Publishing Co., Ltd., Tokyo, Japan, 2004
World Health Organization, International Society of Hypertension Writing Group. 2003 World Health Organization (WHO)/International Society of Hypertension (ISH) statement on management of hypertension. J Hypertens 2003; 21: 1983–92
Chobanian AV, Bakris GL, Black HR, et al. Seventh report of the joint national committee on prevention, detection, evaluation, and treatment of high blood pressure. Hypertension 2003; 42: 1206–52
European Society of Hypertension (ESH) and of the European Society of Cardiology (ESC). Guidelines Committee. 2007 Guidelines for the management of arterial hypertension. J Hypertens 2007; 25: 1105–87
Tomlinson B, Bompart F, Graham BR, et al. Vasodilating mechanism and response to physiological pressor stimuli of acute doses of carvedilol compared with labetalol, propranolol and hydralazine. Drugs 1988; 36: 37–47
Yoshinaga K, Ishii T, Ikeda M, et al. Effect of DQ-2466 (carvedilol) once daily on circadian rhythm of blood pressure in patients with essential hypertension [in Japanese]. Jpn J Clin Exp Med 1989; 66: 3684–92
Seguchi H, Nakamura H, Aosaki N, et al. Effects of carvedilol on serum lipids in hypertensive and normotensive subjects. Eur J Clin Pharmacol 1990; 38 (Suppl. 2): S139–42
Goto Y, Tamachi H, Fusegawa Y, et al. Effect of carvedilol on serum lipid in patients with essential hyptertension [in Japanese]. Geriat Med 1989; 27: 1691–704
Kumahara Y, Ogihara T, Goto Y, et al. Clinical efficacy of carvedilol (DQ-2466) alone in patients with essential hypertension: a multicenter open study [in Japanese]. Jpn J Clin Exp Med 1989; 66: 3968–82
Yasujima M, Ikeda M, Kumahara Y, et al. Clinical efficacy of a combination of carvedilol (DQ-2466) and thiazide diuretics in patients with essential hypertension: a multicenter open study [in Japanese]. Jpn J Clin Exp Med 1990; 67: 658–74
Takahata T, Ohta H, Yamamoto Y, et al. Combination therapy of a b-blocker carvedilol (DQ-2466) with a calcium channel blocker nicardipine in patients with essential hypertension [in Japanese]. Jpn J Clin Exp Med 1990; 67: 1263–8
Takeda T, Kohno M, Ishii T, et al. Clinical efficacy of DQ-2466 (carvedilol) in the treatment of renal parenchymal hypertension: a multicenter open study [in Japanese]. Jpn J Clin Exp Med 1990; 67: 312–24
Yoshinaga K, Ogihara T, Goto Y, et al. Clinical efficacy of carvedilol (DQ-2466) in patients with essential hypertension: a double-blind comparative study with nadolol [in Japanese]. Jpn J Clin Exp Med 1992; 69: 2593–617
Bakris GL, Fonseca V, Katholi RE, et al. Metabolic effects of carvedilol vs. metoprolol in patients with type 2 diabetes mellitus and hypertension: a randomized controlled trial. JAMA 2004; 292: 2227–36
Packer M, Bristow MR, Cohn JN, et al. The effect of carvedilol on morbidity and mortality in patients with chronic heart failure. U.S. Carvedilol Heart Failure Study Group. N Engl J Med 1996; 334: 1349–55
The CAPRICORN Investigators. Effect of carvedilol on outcome after myocardial infarction in patients with left-ventricular dysfunction: the CAPRICORN randomised trial. Lancet 2001; 357: 1385–90
Packer M, Coats AJ, Fowler MB, et al. Effect of carvedilol on survival in severe chronic heart failure. N Engl J Med 2001; 344: 1651–8
Hori M, Sasayama S, Kitabatake A, et al. Low-dose carvedilol improves left ventricular function and reduces cardiovascular hospitalization in Japanese patients with chronic heart failure: the Multicenter Carvedilol Heart Failure Dose Assessment (MUCHA) trial. Am Heart J 2004; 147: 324–30
Poole-Wilson PA, Swedberg K, Cleland JG, et al. Comparison of carvedilol and metoprolol on clinical outcomes in patients with chronic heart failure in the Carvedilol Or Metoprolol European Trial (COMET): randomised controlled trial. Lancet 2003; 362: 7–13
Japanese Circulation Society. Guidelines for treatment of chronic heart failure (JCS 2005) [in Japanese]. Omura Printing Co., Ltd.: Yamaguchi, 2005
Hunt SA, Abraham WT, Chin MH, et al. ACC/AHA 2005 guideline update for the diagnosis and management of chronic heart failure in the adult. Circulation 2005; 112: 154–235
Good Post-Marketing Surveillance Practice [in Japanese; online]. Available from URL: http://www.hourei.mhlw.go.jp/cgi-bin/t_docframe2.cgi?MODE=hourei&DMODE=SEARCH&SMODE=NORMAL&KEYWORD=%90%bb%91%a2%94%cc%94%84%8c%e3%92%b2%8d%b8&EFSNO=597&FILE=FIRST&POS=0&HITSU=83 [Accessed 2011 May 17]
Wikstrand J, Warnold I, Toumilehto J, et al. Metoprolol versus thiazide diuretics in hypertension: morbidity results from the MAPHY study. Hypertension 1991; 17: 579–88
Yusuf S, Peto R, Lewis J, et al. Beta blockade during and after myocardial infarction: an overview of the randomized trials. Prog cardiovasc Dis 1985; 27: 335–42
Nakamura K, Kusano K, Nakamura Y, et al. Carvedilol decreases elevated oxidative stress in human failing myocardium. Circulation 2002; 105: 2867–71
Tsutamoto T, Wada A, Matsumoto T, et al. Relationship between tumor necrosis factor-alpha production and oxidative stress in the failing hearts of patients with dilated caridiomyopathy. J Am Coll Cardiol 2001; 37: 2086–92
Rossig L, Haendeler J, Mallat Z, et al. Congestive heart failure induces endothelial cell apoptosis: protective role of carvedilol. J Am Coll Cardiol 2000; 36: 2081–9
Matsuda Y, Akita H, Terashima M, et al. Carvedilol improves endothelium-dependent dilation in patients with coronary artery disease. Am Heart J 2000; 140: 753–9
Interview form of Artist® Tablets. Apr 2007 (ver. 7) [in Japanese]. Daiichi Sankyo Co., Ltd., Tokyo, 2007
Buhler FR, Laragh JH, Baer L, et al. Propranolol inhibition of rennin secretion: a specific approach to diagnosis and treatment of renin-dependent hypertensive diseases. N Engl J Med 1972; 287: 1209–14
Hollifield JW, Sherman K, Zwagg RV, et al. Proposed mechanisms of propranolol’s antihypertensive effect in essential hypertension. N Engl J Med 1976; 295: 68–73
Stumpe KO, Kolloch R, Vetter H, et al. Acute and longterm studies of the mechanisms of action of beta-blocking drugs in lowering blood pressure. Am J Med 1976; 60: 853–65
Buhler FR, Laragh JH, Sealey JE, et al. Plasma aldosteronerenin interrelationships in various forms of essential hypertension. Studies using a rapid assay of plasma aldosterone. Am J Cardiol 1973; 32: 554–61
Torp-Pederson C, Metra M, Charlesworth A, et al. Effect of metoprolol and carvedilol on preexisting and new onset diabetes in patients with chronic heart failure: data from the Carvedilol Or Metoprolol European Trial (COMET). Heart 2007; 93: 968–73
Acknowledgements
The authors would like to thank the physicians for their support for the drug use survey of Artist® tablets and for providing valuable data. We also thank Nila Bhana, MSc, of inScience Communications, a Wolters Kluwer business, who provided medical writing support funded by Daiichi Sankyo Co., Ltd., Tokyo, Japan.
This study was supported for funding, data collection, and statistical analysis by Daiichi Sankyo Co., Ltd., Tokyo, Japan. Daiichi Sankyo Co., Ltd. was involved in design and conduct of the study; collection, management, analysis, and interpretation of the data; and preparation, review, and approval of the article. In particular, Yasuhiro Nishikawa, MD, provided intellectual advice for the study concept, scientific interpretation of the results, and approval of the article. The authors have no conflicts of interest to declare.
Yasuhiro Nishikawa is currently employed by Global Project Management Department, Daiichi Sankyo Co., Ltd., Tokyo, Japan; Tomoko Iizuka is currently employed by Pharmacovigilance Department, Daiichi Sankyo Co., Ltd., Tokyo, Japan; and Masahiro Komiya is currently employed by Daiichi Sankyo Healthcare Co., Ltd., Tokyo, Japan.
This study was originally published in Japanese in the Journal of Clinical Therapeutics & Medicines [2007; 23 (12): 1051-72]. The study has been reproduced here in English with kind permission of the publisher, Rinsho Iyaku Inc.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 2.0 International License (https://creativecommons.org/licenses/by/2.0), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
About this article
Cite this article
Mori, Y., Nishikawa, Y., Iizuka, T. et al. Artist® Tablets (Carvedilol) for Hypertensive Patients in Japan. Drugs R D 11, 171–190 (2011). https://doi.org/10.2165/11592450-000000000-00000
Published:
Issue Date:
DOI: https://doi.org/10.2165/11592450-000000000-00000