Abstract
The objective of this review was to assess models of cost effectiveness for Parkinson’s disease (PD) published after July 2002 and to derive recommendations for future modelling.
A systematic literature search was performed in the databases PubMed, Current Contents, EMBASE, EconLit, the Cochrane Database of Systematic Reviews, and DARE (Database of Abstracts of Reviews of Effectiveness), NHS EED (Economic Evaluation Database) and HTA (Health Technology Assessment) of the UK NHS Centre for Review and Dissemination (July 2002 to March 2010). Only fully published studies using decision trees, Markov models, individual simulation models or sets of mathematical equations were included.
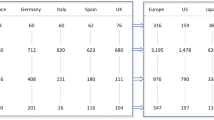
Most of the 11 studies identified used Markov models (n = 9) and two employed were based on decision trees. Based on the Hoehn & Yahr (HY) scale, authors evaluated the cost effectiveness of drug treatments (n = 6), surgical approaches such as deep brain stimulation (n = 1) or striatal cell grafting (n = 1), and diagnostic procedures such as single photon emission computed tomography (SPECT) testing (n = 3) over a time horizon of 1 year to lifetime. Costs were adapted to address a societal and/or healthcare provider/ third-party payer perspective. All but one of the interventions investigated were considered cost effective or cost saving.
Cost-effectiveness modelling in PD between 2003 and 2010 showed only minor improvement when compared with our earlier review of models published from 1998 up to 2003. Cost-effectiveness modelling recommendations were complied with to only a limited extent, leaving room for quality improvement. More advanced modelling approaches may, so far, be underrepresented, but may be used in the future, driven by the research question. Adverse events of treatment, co-morbidities or disease complications are not yet sufficiently included in the models to adequately represent clinical reality.



Similar content being viewed by others
Notes
Cabergoline, along with other ergoline dopamine agonists, was removed for the treatment of PD from the market in 2007 due to cardiac adverse effects.[66]
The disease is considered to be in an ‘on’ stage when the symptoms respond well to treatment. The disease is considered to be in an ‘off’ stage when it is either not or not adequately responding to treatment and the patient is experiencing significant symptoms.
References
Hoehn MM. The natural history of Parkinson’s disease in the pre-levodopa and post-levodopa eras. Neurol Clin 1992; 10 (2): 331–9
Mutch WJ, Dingwall-Fordyce I, Downie AW, et al. Parkinson’s disease in a Scottish city. BMJ 1986; 292 (6519): 534–6
Rajput AH, Offord KP, Beard CM, et al. Epidemiology of parkinsonism: incidence, classification, and mortality. Ann Neurol 1984; 16 (3): 278–82
Sutcliffe RL, Meara JR. Parkinson’s disease epidemiology in the Northampton District, England, 1992. Acta Neurol Scand 1995; 92: 443–50
Twelves D, Perkins KS, Counsell C. Systematic review of incidence studies of Parkinson’s disease. Mov Disord 2003; 18 (1): 19–31
Schrag A, Jahanshahi M, Quinn N. What contributes to quality of life in patients with Parkinson’s disease? J Neurol Neurosurg Psychiatry 2000; 69 (3): 308–12
Oertel WH, Quinn NP. Parkinsonism. In: Brandt T, Diener HC, Caplan LR, et al., editors. Neurological disorders: course and treatment. San Diego (CA): Academic Press, 2003
Olanow CW, Watts RL, Koller WC. An algorithm (decision tree) for the management of Parkinson’s disease (2001): treatment guidelines. Neurology 2001; 56 (11 Suppl.5): S1–88
Rascol O, Goetz C, Koller W, et al. Treatment interventions for Parkinson’s disease: an evidence based assessment. Lancet 2002; 359 (9317): 1589–98
Bronstein JM, Tagliati M, Alterman RL, et al. Deep brain stimulation for Parkinson disease: an expert consensus and review of key issues. Arch Neurol 2011; 68: 165
Kluger BM, Klepitskaya O, Okun MS. Surgical treatment of movement disorders. Neurol Clin 2009; 27: 633–77
Puig-Junoy J, Puig Peiro R. Review of the economic evidence on the use of deep brain stimulation in late stage Parkinson’s disease. Neurologia 2009; 24 (4): 220–9
Eggert KM, Reese JP, Oertel WH, et al. Cost effectiveness of pharmacotherapies in early Parkinson’s disease. CNS Drugs 2008; 22 (10): 841–60
Siebert U, Bornschein B, Walbert T, et al. Systematic assessment of decision models in Parkinson’s disease. Value Health 2004; 7 (5): 610–26
Weinstein MC, O’Brien B, Hornberger J, et al. Principles of good practice for decision analytic modeling in health-care evaluation: report of the ISPOR Task Force on Good Research Practices–Modeling Studies. Value Health 2003; 6 (1): 9–17
Nuijten MJ. Incorporation of statistical uncertainty in health economic modelling studies using second-order Monte Carlo simulations. Pharmacoeconomics 2004; 22 (12): 759–69
Nuijten MJ, Kosa J, Engelfriet P. Modeling the costeffectiveness and budgetary impact for subpopulations. Eur J Health Econ 2003; 4 (2): 70–8
Nuijten MJ, Rutten F. Combining a budgetary-impact analysis and a cost-effectiveness analysis using decisionanalytic modelling techniques. Pharmacoeconomics 2002; 20 (12): 855–67
Nuijten MJ, Rutten F. The incorporation of potential confounding variables in Markov models. Pharmacoeconomics 2003; 21 (13): 941–50
van den Hout A, Matthews FE. Estimating dementia-free life expectancy for Parkinson’s patients using Bayesian inference and microsimulation. Biostatistics 2009; 10 (4): 729–43
Drummond MF, O’Brien B, Stoddard GL, et al. Methods for the economic evaluation of health care programs. New York: Oxford University Press, 1997
Gold MR, Siegel JE, Russell LB, et al. Cost-effectiveness in health and medicine. New York: Oxford University Press, 1996
Siebert U, Behrend C, Mühlberger N, et al. Entwicklung eines Kriterienkataloges zur Beschreibung und Bewertung ökonomischer Evaluationsstudien in Deutschland. In: Leidel R, Graf von der Schulenburg JM, Wasem J, editors. Approaches and methods of economic evaluation in health care: an international perspective [in German]. Baden-Baden: Nomos Verlagsgesellschaft, 1999: 156–70
Lindgren P, Jonsson B, Duchane J. The cost-effectiveness of early cabergoline treatment compared to levodopa in Sweden. Eur J Health Econ 2003; 4 (1): 37–42
Rinne UK, Bracco F, Chouza C, et al. Early treatment of Parkinson’s disease with cabergoline delays the onset of motor complications: results of a double-blind levodopa controlled trial. The PKDS009 Study Group. Drugs 1998; 55 Suppl.1: 23–30
Hagell P, Nordling S, Reimer J, et al. Resource use and costs in a Swedish cohort of patients with Parkinson’s disease. Mov Disord 2002 Nov; 17 (6): 1213–20
Dodel RC, Singer M, Kohne-Volland R, et al. The economic impact of Parkinson’s disease: an estimation based on a 3-month prospective analysis. Pharmacoeconomics 1998; 14 (3): 299–312
LePen C, Wait S, Moutard-Martin F, et al. Cost of illness and disease severity in a cohort of French patients with Parkinson’s disease. Pharmacoeconomics 1999; 16 (1): 59–69
Smala AM, Spottke EA, Machat O, et al. Cabergoline versus levodopa monotherapy: a decision analysis. Mov Disord 2003; 18 (8): 898–905
Di Rocco A, Molinari SP, Kollmeier B, et al. Parkinson’s disease: progression and mortality in the L-DOPAera. Adv Neurol 1996; 69: 3–11
Spottke AE, Reuter M, Machat O, et al. Cost of illness and its predictors for Parkinson’s disease in Germany. Pharmacoeconomics 2005; 23: 817–36
Hudry J, Rinne JO, Keranen T, et al. Cost-utility model of rasagiline in the treatment of advanced Parkinson’s disease in Finland. Ann Pharmacother 2006; 40 (4): 651–7
Rascol O, Brooks DJ, Melamed E, et al. Rasagiline as an adjunct to levodopa in patients with Parkinson’s disease and motor fluctuations (LARGO, Lasting effect in Adjunct therapy with Rasagiline Given Once daily, study): a randomised, double-blind, parallel-group trial. Lancet 2005; 365 (9463): 947–54
Palmer CS, Schmier JK, Snyder E, et al. Patient preferences and utilities for ‘off-time’ outcomes in the treatment of Parkinson’s disease. Qual Life Res 2000; 9 (7): 819–27
Keranen T, Kaakkola S, Sotaniemi K, et al. Economic burden and quality of life impairment increase with severity of PD. Parkinsonism Relat Disord 2003; 9 (3): 163–8
Haycox A, Armand C, Murteira S, et al. Cost effectiveness of rasagiline and pramipexole as treatment strategies in early Parkinson’s disease in the UK setting: an economicMarkov model evaluation. Drugs Aging 2009; 26 (9): 791–801
Parkinson Study Group. A controlled trial of rasagiline in early Parkinson disease: the TEMPO Study. Arch Neurol 2002; 59 (12): 1937–43
Parkinson Study Group. A controlled, randomized, delayed- start study of rasagiline in early Parkinson disease. Arch Neurol 2004; 61 (4): 561–6
Holloway RG, Shoulson I, Fahn S, et al. Pramipexole vs levodopa as initial treatment for Parkinson disease: a 4-year randomized controlled trial. Arch Neurol 2004; 61 (7): 1044–53
Parkinson Study Group. Entacapone improves motor fluctuations in levodopa-treated Parkinson’s disease patients. Ann Neurol 1997; 42: 747–55
Rascol O, Brooks DJ, Korczyn AD, et al. A five-year study of the incidence of dyskinesia in patients with early Parkinson’s disease who were treated with ropinirole or levodopa. 056 Study Group. N Engl J Med 2000; 342 (20): 1484–91
Findley L, Aujla M, Bain PG, et al. Direct economic impact of Parkinson’s disease: a research survey in the United Kingdom. Mov Disord 2003; 18 (10): 1139–45
Findley LJ, Lees A, Apajasalo M, et al. Cost-effectiveness of levodopa/carbidopa/entacapone (Stalevo) compared to standard care in UK Parkinson’s disease patients with wearing-off. Curr Med Res Opin 2005; 21 (7): 1005–14
Schrag A, Jahanshahi M, Quinn N. How does Parkinson’s disease affect quality of life? A comparison with quality of life in the general population. Mov Disord 2000; 15 (6): 1112–8
Rinne UK, Larsen JP, Siden A, et al. Entacapone enhances the response to levodopa in parkinsonian patients with motor fluctuations. NOMECOMT Study Group. Neurology 1998; 51 (5): 1309–14
UK Office for National Statistics. Mortality rates [online]. Available from URL: http://www.statistics.gov.uk [Accessed 2010 Mar 1]
Kristiansen IS, Bingefors K, Nyholm D, et al. Short-term cost and health consequences of duodenal levodopa infusion in advanced Parkinson’s disease in Sweden: an exploratory study. Appl Health Econ Health Policy 2009; 7 (3): 167–80
Nyholm D, Nilsson Remahl AI, Dizdar N, et al. Duodenal levodopa infusion monotherapy vs oral polypharmacy in advanced Parkinson disease. Neurology 2005; 64 (2): 216–23
Goulionis JE, Vozikis A. Medical decision making for patients with Parkinson disease under average cost criterion. Aust New Zealand Health Policy 2009; 6: 15
Hjelmgren J, Ghatnekar O, Reimer J, et al. Estimating the value of novel interventions for Parkinson’s disease: an early decision-making model with application to dopamine cell replacement. Parkinsonism Relat Disord 2006; 12 (7): 443–52
Hely MA, Morris JG, Traficante R, et al. The Sydney multicentre study of Parkinson’s disease: progression and mortality at 10 years. J Neurol Neurosurg Psychiatry 1999; 67 (3): 300–7
Schrag A, Selai C, Jahanshahi M, et al. The EQ-5D–a generic quality of life measure–is a useful instrument to measure quality of life in patients with Parkinson’s disease. J Neurol Neurosurg Psychiatry 2000; 69 (1): 67–73
Lindvall OF, Hagell P. Status of neural repair clinical trials in brain diseases. In: Selzer ME, Clarke S, Cohen LG, et al., editors. Textbook of neural repair and rehabilitation: neural repair and plasticity. Vol. 1. Cambridge: Cambridge University Press, 2006: 615–31
Hagell P, Piccini P, Bjorklund A, et al. Dyskinesias following neural transplantation in Parkinson’s disease. Nat Neurosci 2002; 5 (7): 627–8
Antonini A, Berto P, Lopatriello S, et al. Cost-effectiveness of 123I-FP-CIT SPECT in the differential diagnosis of essential tremor and Parkinson’s disease in Italy. Mov Disord 2008; 23 (15): 2202–9
Benamer TS, Patterson J, Grosset DG, et al. Accurate differentiation of parkinsonism and essential tremor using visual assessment of [123I]-FP-CIT SPECT imaging: the [123I]-FPCIT study group. Mov Disord 2000; 15 (3): 503–10
Meara J, Bhowmick BK, Hobson P. Accuracy of diagnosis in patients with presumed Parkinson’s disease. Age Ageing 1999; 28: 99–102
Van Laere K, Everaert L, Annemans L, et al. The cost effectiveness of 123I-FP-CIT SPECT imaging in patients with an uncertain clinical diagnosis of parkinsonism. Eur J Nucl Med Mol Imaging 2008; 35 (7): 1367–76
Hughes AJ, Daniel SE, Kilford L, et al. The accuracy of clinical diagnosis of idiopathic Parkinson’s disease: a clinicopathological study of 100 cases. J Neurol Neurosurg Psychiatry 1992; 55: 181–4
Jankovic J. Essential tremor: clinical characteristics. Neurology 2000; 54 (11 Suppl.4): S21–5
Rajput AH, Rozdilsky B, Rajput A. Accuracy of clinical diagnosis in parkinsonism: a prospective study. Can J Neurol Sci 1991; 18: 275–8
Dodel RC, Höffken H, Möller JC, et al. Dopamine transporter imaging and SPECT in diagnostic work-up of Parkinson’s disease: a decision-analytic approach. Mov Disord 2003; 18 Suppl.7: S52–62
Hughes AJ, Ben-Shlomo Y, Daniel SE, et al. What features improve the accuracy of clinical diagnosis in Parkinson’s disease: a clinicopathologic study. 1992. Neurology 2001; 57 (10 Suppl.3): S34–8
Hughes AJ, Daniel SE, Ben-Shlomo Y, et al. The accuracy of diagnosis of Parkinsonian syndromes in a specialist movement disorder service. Brain 2002; 125: 861–70
Hughes AJ, Daniel SE, Lees AJ. Improved accuracy of clinical diagnosis of Lewy body Parkinson’s disease. Neurology 2001; 57 (8): 1497–9
Schade R, Andersohn F, Suissa S, et al. Dopamine agonists and the risk of cardiac-valve regurgitation. N Engl J Med 2007; 356 (1): 29–38
Nuijten MJ, van Iperen P, Palmer C, et al. Cost-effectiveness analysis of entacapone in Parkinson’s disease: a Markov process analysis. Value Health 2001; 4 (4): 316–28
Palmer CS, Nuijten MJ, Schmier JK, et al. Cost effectiveness of treatment of Parkinson’s disease with entacapone in the United States. Pharmacoeconomics 2002; 20 (9): 617–28
Herlofson K, Lie SA, Arsland D, et al. Mortality and Parkinson disease: a community based study. Neurology 2004; 62 (6): 937–42
Parkinson Study Group. Pramipexole vs levodopa as initial treatment for Parkinson disease: a randomized controlled trial. Parkinson Study Group. JAMA 2000; 284 (15): 1931–8
Linna M, Taimela E, Apajasalo M, et al. Probabilistic sensitivity analysis for evaluating cost-utility of entacapone for Parkinson’s disease. Expert Rev Pharmacoecon Outcomes Res 2002; 2 (2): 91–7
Brooks DJ, Sagar H, UK-Irish Entacapone Study Group. Entacapone is beneficial in both fluctuating and nonfluctuating patients with Parkinson’s disease: a randomised, placebo controlled, double blind, six month study. J Neurol Neurosurg Psychiatry 2003; 74 (8): 1071–9
Nilsson D, Nyholm D, Aquilonius SM. Duodenal levodopa infusion in Parkinson’s disease: long-term experience. Acta Neurol Scand 2001; 104 (6): 343–8
Ministry of Health. Prestazioni di assistenza specialistica ambulatoriale erogabili nell’ambito del SSN e relative tariffe GU n 216 of 14/11/1996: DM 22/07/1996
Winter Y, von Campenhausen S, Arend M, et al. Healthrelated quality of life and its determinants in Parkinson’s disease: results of an Italian cohort study. Parkinsonism Relat Disord; 17 (4): 265–9
Baker CB, Johnsrud MT, Crismon ML, et al. Quantitative analysis of sponsorship bias in economic studies of antidepressants. Br J Psychiatry 2003; 183: 498–506
Bell CM, Urbach DR, Ray JG, et al. Bias in published cost effectiveness studies: systematic review. BMJ 2006; 332 (7543): 699–703
Briggs A, Claxton K, Sculpher M. Decision modelling for health economic evaluation. Oxford: Oxford University Press, 2006
Institute for Quality and Efficiency in Health Care. Working Paper on Modelling in health economic evaluations. Cologne: IQWiG, 2009 [online]. Available from URL: http://www.iqwig.de/download/Working_Paper_Modelling.pdf [Accessed 2010 Jun 21]
Acknowledgements
The authors have no conflicts of interest that are directly relevant to the content of this study. Full financial disclosure for Professor Dr R. Dodel is available as SDC 2, http://links.adisonline.com/PCZ/A122.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Dams, J., Bornschein, B., Reese, J.P. et al. Modelling the Cost Effectiveness of Treatments for Parkinson’s Disease. Pharmacoeconomics 29, 1025–1049 (2011). https://doi.org/10.2165/11587110-000000000-00000
Published:
Issue Date:
DOI: https://doi.org/10.2165/11587110-000000000-00000