Abstract
Background and Objective
Vicriviroc is a small-molecule CCR5 antagonist currently in development for the treatment of HIV in patients on a regimen containing a ritonavir-boosted protease inhibitor. As renal disease and renal dysfunction are prevalent in the HIV-infected population, patients with varying degrees of renal insufficiency may receive vicriviroc, which is metabolized by cytochrome P450 (CYP) 3A4. The present study therefore examined the impact of renal insufficiency on the pharmacokinetics and safety of vicriviroc alone and in the presence of ritonavir, a strong CYP3A4 inhibitor.
Subjects and Methods
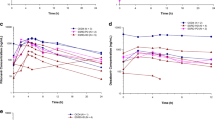
This study was an open-label, randomized, two-treatment crossover trial conducted in HIV-negative subjects with haemodialysis-dependent end-stage renal disease (ESRD) and healthy subjects with normal renal function matched by age, height, bodyweight and sex. Subjects received a single dose of vicriviroc 75 mg alone in one period, and in another period they received a single dose of vicriviroc 15 mg after 4 days of ritonavir 100 mg once daily. Ritonavir treatment was then continued for an additional 13 days. The two trial periods were separated by an interval of at least 3 weeks. The primary endpoints were the log-transformed area under the plasma concentration-time curve (AUC) and the maximum plasma concentration (Cmax), and the 90% confidence intervals (CIs) of the mean differences between subjects with ESRD and matched healthy subjects. The protocol provided the option of dose modification and further study if the vicriviroc Cmax and AUC values were at least twice as high in subjects with ESRD compared with healthy subjects, or if warranted by other safety and tolerability observations.
Results
Twelve subjects (six with ESRD, six healthy) completed the study. When vicriviroc was administered alone, the mean vicriviroc Cmax and AUC ratio estimates (90% CI) for subjects with ESRD versus healthy subjects were 74% (53, 103) and 84% (49, 145), respectively. When ritonavir was added to the regimen, the ratio estimates (90% CI) were 81% (59, 111) and 134% (105, 171), respectively. Ritonavir plasma concentrations were substantially higher in subjects with ESRD than in healthy subjects. Treatment-emergent adverse events considered possibly or probably related to treatment occurred only during the ritonavir period of the study and in one healthy subject and two subjects with ESRD; all were of mild or moderate severity. Conclusions: ESRD had no clinically relevant impact on exposure of vicriviroc when vicriviroc was administered alone or in the presence of ritonavir. In this single-dose study, vicriviroc was well tolerated both by healthy subjects and by those with ESRD. Dose adjustment of vicriviroc is therefore not necessary in renally impaired populations.







Similar content being viewed by others
References
Strizki JM, Tremblay C, Xu S, et al. Discovery and characterization of vicri-viroc (SCH 417690), a CCR5 antagonist with potent activity against human immunodeficiency virus type 1. Antimicrob Agents Chemother 2005; 49: 4911–9
Gulick RM, Su Z, Flexner C, et al. Phase 2 study of the safety and efficacy of vicriviroc, a CCR5 inhibitor, in HIV-1-infected, treatment-experienced patients: AIDS clinical trials group 5211. J Infect Dis 2007; 196: 304–12
Zingman B, Suleiman J, DeJesus E, et al. Vicriviroc in combination therapy with an optimized antiretroviral regimen for treatment-experienced subjects: the VICTOR-E1 trial [abstract no. 795]. 15th Conference on Retroviruses and Opportunistic Infections; 2008 Feb 3–6; Boston (MA)
Hsu A, Granneman GR, Bertz RJ. Ritonavir: clinical pharmacokinetics and interactions with other anti-HIV agents. Clin Pharmacokinet 1998; 35: 275–91
Granfors MT, Wang JS, Kajosaari LI, et al. Differential inhibition of cytochrome P450 3A4, 3A5, and 3A7 by five human immunodeficiency virus (HIV) protease inhibitors in vitro. Basic Clin Pharmacol Toxicol 2006; 98: 79–85
Seiberling M, Kraan M, Keung A, et al. Similar increase in SCH 417690 plasma exposure with coadministration of varying doses of ritonavir in healthy volunteers [abstract no. TuPe3.1B06]. 3rd IAS Conference on HIVPathogenesis and Treatment; 2005 Jul 24–27; Rio de Janeiro
Wyatt CM, Winston JA, Malvestutto CD, et al. Chronic kidney disease in HIV infection: an urban epidemic. AIDS 2007; 21: 2101–3
Choi AI, Rodriguez RA, Bacchetti P, et al. Low rates of antiretroviral therapy among HIV-infected patients with chronic kidney disease. Clin Infect Dis 2007; 45: 1633–9
Gilden DE, Kubisiak JM, Gilden DM. Managing Medicare’s HIV caseload in the era of suppressive therapy. Am J Public Health 2007; 97: 1053–9
Wyatt CM, Klotman PE. HIV-associated nephropathy in the era of antiretroviral therapy. Am J Med 2007; 120: 488–92
Schwartz EJ, Szczech LA, Ross MJ, et al. Highly active antiretroviral therapy and the epidemic of HIV+end-stage renal disease. J Am Soc Nephrol 2005; 16: 2412–20
Röling J, Schmid H, Fischereder M, et al. HIV-associated renal diseases and highly active antiretroviral therapy-induced nephropathy. Clin Infect Dis 2006; 42: 1488–95
Goicoechea M, Liu S, Best B, et al. Greater tenofovir-associated renal function decline with protease inhibitor-based versus nonnucleoside reverse-transcriptase inhibitor-based therapy. J Infect Dis 2008; 197: 102–8
Denissen JF, Grabowski BA, Johnson MK, et al. Metabolism and disposition of the HIV-1 protease inhibitor ritonavir (ABT-538) in rats, dogs, and humans. Drug Metab Dispos 1997; 25: 489–501
Norvir® (ritonavir capsules) soft gelatin (ritonavir oral solution): US prescribing information. North Chicago (IL): Abbott Laboratories, 2007 Jul
Ramanathan R, Ghosal A, Miller MW, et al, inventors. Piperazine derivatives useful as CCR5 antagonists. US patent application 20060105964. 2005 Oct 27
Ghosal A, Ramanathan R, Yuan Y, et al. Identification of human liver cytochrome P450 enzymes involved in biotransformation of vicriviroc, a CCR5 receptor antagonist. Drug Metab Dispos 2007; 35: 2186–95
Ramanathan R, Zhong R, Alvarez N, et al. Comparative metabolism and excretion of a novel CCR5 receptor antagonist, SCH 417690 (vicriviroc), in human, monkey, and rat. Drug Metab Rev 2005; 37: 725–6
US FDA Center for Drug Evaluation and Research [CDER]. Guidance for industry. Pharmacokinetics in patients with impaired renal function — study design, data analysis, and impact on dosing and labeling. Rockville (MD): CDER, 1998 May
Izzedine H, Launay-Vacher V, Baumelou A, et al. An appraisal of antiretroviral drugs in hemodialysis. Kidney Int 2001; 60: 821–30
Data on file, Schering Corporation, 2007
Selzentry™ (maraviroc) tablets: US prescribing information. New York: Pfizer Inc., 2007 Aug
Schering-Plough. Efficacy and safety of vicriviroc in HIV-infected treatmentnaïve subjects (study P04875AM1) [ClinicalTrials.gov identifier NCT00 551018]. US National Institutes of Health, ClinicalTrials.gov [online]. Available from URL: http://www.clinicaltrials.gov/ct2/show/NCT00551018?term=vicriviroc+AND+treatment-naive&rank=1 [Accessed 2010 Feb 1]
Acknowledgements
This trial was supported by Schering-Plough Research Institute, a part of the Schering Corporation. Assistance with manuscript preparation, funded by Schering-Plough, was provided by Sui Generis Health (New York, NY). Claudia Kasserra, Ernestina Tetteh and Edward O’Mara are employees of Schering-Plough and own Schering-Plough stock. Chi-Fung Keung (Anther), Angela Sansone-Parsons and Mahmoud Assaf were employees of Schering-Plough during the conduct and analysis of the study. Thomas Marbury has no conflicts of interest that are directly relevant to the contents of this study.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Kasserra, C., Sansone-Parsons, A., Keung, A. et al. Renal Insufficiency Has No Effect on the Pharmacokinetics of Vicriviroc in a Ritonavir-Containing Regimen. Clin Pharmacokinet 49, 397–406 (2010). https://doi.org/10.2165/11319470-000000000-00000
Published:
Issue Date:
DOI: https://doi.org/10.2165/11319470-000000000-00000