Abstract
Introduction
Ensitrelvir, a novel oral inhibitor of 3C-like protease of SARS-CoV-2, shows efficacy and safety in participants with mild to moderate COVID-19. Since urinary recovery of ensitrelvir ranged from 12.9% to 21.8% across dose groups given 20–1000 mg in a single-ascending dose study, renal excretion contributes to the elimination of ensitrelvir. Therefore, the effect of renal impairment on the pharmacokinetics and safety of ensitrelvir needed to be evaluated.
Methods
This study (NCT05363215) was a phase 1, open-label, nonrandomized, parallel-group study. The effect of renal function on the pharmacokinetics of ensitrelvir was investigated. Ensitrelvir was administered as a single dose of 375 mg to participants with normal renal function and those with mild, moderate, and severe renal impairment. The participants with normal renal function were matched to each participant with moderate renal impairment with respect to sex, age, and body mass index. The unbound fractions in plasma after administration of ensitrelvir were also evaluated. For the safety assessment, the nature, frequency, and severity of treatment-emergent adverse events were evaluated and recorded.
Results
The plasma concentrations of participants with renal impairment were higher than those of participants with normal renal function. The ratios (90% confidence intervals) of the area under the plasma concentration-time curve from 0 to infinity (AUC0–inf) in participants with mild, moderate, and severe renal impairment compared to normal renal function were 1.4374 (1.1716–1.7636), 1.4885 (1.1883–1.8646), and 1.6021 (1.2782–2.0080), respectively. The plasma protein-unbound fraction was similar regardless of the plasma ensitrelvir concentration or renal function. Ensitrelvir was well tolerated in participants with mild to severe renal impairment and normal renal function.
Conclusion
Ensitrelvir was well tolerated by participants with renal impairment. There was no clinically meaningful increase on exposure to ensitrelvir in participants with renal impairment, indicating that no dose adjustment would be required due to renal function.
Similar content being viewed by others
Why carry out this study? |
On administration of ensitrelvir, a novel oral inhibitor of 3C-like protease of SARS-CoV-2, the urinary recovery ranged from 12.9% to 21.8% after a single dose of 20 to 1000 mg. |
Impaired renal function may affect the pharmacokinetics of drugs that are eliminated by the kidney, thus requiring dose adjustment or restriction. |
What was learned from the study? |
Ensitrelvir was well tolerated by participants with renal impairment. |
No dose adjustment should be required because of renal function for ensitrelvir use because its safety was confirmed within the range of increased exposure. |
Introduction
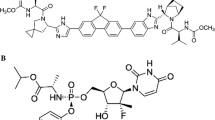
Ensitrelvir is an inhibitor of the novel 3C-like protease of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), which is essential for viral replication [1]. Ensitrelvir showed antiviral activity against a broad spectrum of SARS-CoV-2 variants including the omicron strain and coronavirus families [1] in preclinical studies. In a clinical study, ensitrelvir demonstrated favorable antiviral efficacy, potential clinical benefit and acceptable safety in the phase 2b part [2] and phase 3 part [3] of a randomized phase 2/3 study following a two-dose regimen. In the multiple-dose administration, ensitrelvir at 375 mg was given as the loading dose on Day 1 followed by 125 mg as the maintenance dose on Days 2 to 5 (375/125 mg) or at 750 mg as the loading dose on Day 1 followed by 250 mg as the maintenance dose on Days 2 to 5 (750/250 mg). Under the Emergency Regulatory Approval System, ensitrelvir was approved in Japan on November 22, 2022, for patients who are > 12 years old with mild to moderate SARS-CoV-2 infection, regardless of risk factors or vaccination status, with a dose regimen for the treatment of COVID-19 of 5-day oral administration of 375/125 mg [4].
The urinary recovery of ensitrelvir ranged from 12.9% to 21.8% after single oral administration of ensitrelvir at 20 to 1000 mg in the initial single-ascending dose study [5]. An in vitro study suggested that ensitrelvir is not a substrate for renal transporters, such as organic cation transporter (OCT) 2, multidrug and toxin extrusion (MATE) 1 and MATE-2K [6]. Ensitrelvir can be given to a wide range of patients including those with renal impairment. However, impaired renal function may affect the pharmacokinetics of drugs which are eliminated by the kidney, and some drugs require dose adjustment or restriction of use [7,8,9]. Therefore, the purpose of this study was to evaluate the effect of renal impairment on the pharmacokinetics and safety of ensitrelvir in participants with mild, moderate, and severe renal impairment.
Methods
Study Participants and Design
This study was designed in accordance with the FDA draft guidance on pharmacokinetics in participants with impaired renal function [10]. The renal function was classified based on the FDA draft guidance [10], and renal impairment participants were assigned according to their estimated glomerular filtration rate (eGFR), which was calculated by modification of diet using the renal disease (MDRD) formula [11] and the participant’s body surface area at screening (day − 28 to day − 2 relative to day 1): normal renal function (control participants eGFR ≥ 90 ml/min, n = 8), mild impairment (eGFR 60–89 ml/min, n = 8), moderate impairment (eGFR 30–59 ml/min, n = 8), and severe impairment (eGFR < 30 ml/min, n = 8). Participants with severe renal impairment were not included if they required hemodialysis. Each of the eight participants with normal renal function (control participants) was matched to a participant with moderate renal impairment with respect to sex, age (± 5 years), and BMI (± 10%).
A Phase 1, open-label, nonrandomized, parallel-group study was conducted to access the pharmacokinetics, safety, and tolerability of ensitrelvir in participants with mild, moderate, and severe renal impairment and participants with normal renal function. The participants received a single oral administration of ensitrelvir 375 mg (three 125-mg tablets). This clinical study was conducted from July 2022 to May 2023.
Ethical Compliance
This study (NCT05363215) was conducted in accordance with the study protocol approved by the Declaration of Helsinki and Council for International Organizations of Medical Sciences International Ethical Guidelines, the Institutional Review Board, the International Council for Harmonisation of Technical Requirements for Pharmaceuticals for Human Use Good Clinical Practice Guidelines, and other regulations and applicable laws. The Institutional Review Board also approved the study. All participants in this study signed a written informed consent form before participation [12,13,14].
Bioanalytical Procedure
Plasma ensitrelvir concentrations were determined by liquid chromatography with tandem mass spectrometry (LC/MS/MS). Acetonitrile was used for the protein precipitation. API4000 (Sciex, Framingham, MA) was used for the LC/MS/MS analysis. The determination method was validated over a range of 200–200,000 ng/ml, and the lower limit of quantification (LLOQ) of the method was 200 ng/ml.
Blood and Urine Collection
Pharmacokinetic blood samples were collected at 0, 0.5, 1, 1.5, 2, 2.5, 3, 4, 6, 8, 12, 16, 24, 48, 72, 96, 120, 144, 192, 240, 288, and 336 h postdose. Blood samples for protein binding were collected at 3 and 24 h postdose. Pharmacokinetic urine samples were collected at 0–24, 24–48, 48–72, 72–96, 96–120, 120–144, 144–168, 168–192, 192–216, 216–240, 240–264, 264–288, 288–312, and 312–336 h postdose.
Pharmacokinetic Assessments
The mean and standard deviations (SD) for plasma ensitrelvir concentrations were calculated by group and sampling time. In this study, the plasma ensitrelvir concentrations below the LLOQ value (200 ng/ml) were treated as zero for calculating the mean and SD for plasma ensitrelvir concentrations. Non-compartmental analysis was used to calculate the following pharmacokinetic parameters based on the plasma ensitrelvir concentrations: Cmax, time to maximum plasma concentration (Tmax), area under the plasma concentration-time curve from time zero to the time of last quantifiable concentration after dosing (AUC0–last), AUC0–inf, terminal elimination half-life (t1/2,z), terminal elimination rate constant (λz), and mean residence time (MRT). In addition, the unbound fraction in plasma (fu) was also assessed at 3 and 24 h following a single-dose administration of ensitrelvir. The cumulative amount of drug excreted unchanged in the urine (Ae), fraction of dose excreted unchanged into urine (Feu), and renal clearance of ensitrelvir (CLR) were estimated for each participant or patient with urinary excretion data. The pharmacokinetic parameters were calculated using Phoenix WinNonlin version 8.3 (Certara L.P., Princeton, NJ, USA).
Statistical Analyses
Analysis of variance (ANOVA) was conducted using SAS version 9.4 (SAS Institute Inc., Cary, NC, USA) using the Proc Mixed procedure, which included terms for renal status as a fixed effect for the ln-transformed values of the pharmacokinetic parameters. Point estimates and 90% confidence intervals (CIs) were calculated for the ratios of parameters for participants with mild, moderate, and severe renal impairment compared with participants with normal renal function.
Safety
Safety was assessed including the analysis of all treatment-emergent adverse events (TEAEs), which were categorized according to the System Organ Class and Preferred Term of MedDRA version 25.0. The nature, frequency, and severity of TEAEs were evaluated and recorded.
Results
Study Participants and Baseline Demographics
A total 34 participants were enrolled, and 32 participants completed this study. Two participants in the moderate renal impairment group were withdrawn prior to treatment because the target number of participants had already been reached for this group. The demographic and baseline characteristics of the 32 participants who completed the study are summarized in Table 1. Overall, the mean age (SD) at informed consent was 64.2 (10.15) years. The majority of participants were male (65.6%). The mean (SD) BMI was 29.0 kg/m2 (3.90). The differences in demographics between the groups for moderate renal impairment and normal renal function were included in the defined criteria for the demographically matched-control design [i.e., sex, age (± 5 years), and BMI (± 10%)].
Pharmacokinetics
Mean (SD) plasma concentration profiles following a single-dose oral administration of ensitrelvir 375 mg are shown in Fig. 1. The plasma concentrations for the participants with renal impairment tended to be higher than those in the participants with normal renal function. A summary of the PK parameters is listed in Table 2. AUC was higher in participants with poorer renal function. The geometric mean CLR values for normal, mild, moderate, and severe participants were 0.0561, 0.0327, 0.0406, and 0.0325 l/h, respectively. The comparisons of PK parameters between renal impairment groups and the normal group are presented in Table 3. As results of ANOVA, the geometric mean ratios (corresponding 90% confidence intervals [CIs]) of Cmax for participants with mild, moderate, and severe renal impairment compared to healthy control participants with normal renal function were 1.3239 (1.0409–1.6837), 1.3274 (1.0608–1.6611), and 1.1141 (0.8737–1.4206), respectively, and those of AUC0–inf for participants with mild, moderate, and severe renal impairment compared to healthy control participants with normal renal function were 1.4374 (1.1716–1.7636), 1.4885 (1.1883–1.8646), and 1.6021 (1.2782–2.0080), respectively.
Mean (standard deviation) pharmacokinetic profiles of normal renal impairment participants and participants with renal impairment following single-dose administration of ensitrelvir 375 mg. Plasma concentrations of participants with normal renal impairment, filled circles; with mild renal impairment, open circles; with moderate renal impairment, filled triangles; with severe renal impairment, open triangles. The figures are in linear (upper) and semilogarithmic (lower) scales
The results of the unbound fraction (fu) are listed in Table 4. The geometric means fu at 3 h and 24 h following a single-dose administration of ensitrelvir in the normal and the mild, moderate, and severe impairment groups were 0.0125–0.0172 and 0.0118–0.0165, respectively; they were similar regardless of renal function.
Safety and Tolerability
All treated participants (32 participants, 94.1% of the enrolled participants) were included in the safety population. All treated participants received a single oral dose of ensitrelvir (375 mg). The overall summaries of TEAEs and treatment-related AEs are shown in Tables 5 and 6, respectively. In total, TEAEs were reported for five participants (15.6%). Of these, TEAEs were reported for three (37.5%) participants with mild renal impairment and two (25.0%) participants with moderate renal impairment. No participants with severe renal impairment or normal renal function experienced TEAEs. There were no deaths and no nonfatal serious TEAEs reported during the study. Also no AESIs and no TEAEs leading to withdrawal from the study were reported. No severe TEAEs or treatment-related TEAEs were reported. All TEAEs and treatment-related TEAEs were categorized as mild or moderate. Ensitrelvir was well tolerated in participants with renal impairment. Detailed results are shown in Supplemental Table S1 and S2.
Discussion
Information about pharmacokinetics and safety for participants with renal impairment is essential for drug development and appropriate clinical utilization of drugs that are excreted by the kidney. As ensitrelvir, which is a novel oral inhibitor of 3C-like protease of SARS-CoV-2, was recovered in urine at about 20% from the phase 1 study [5], the effect of renal function on enstirelvir was evaluated in this clinical study.
The plasma ensitrelvir concentrations of participants with renal impairment were higher than those of the participants with normal renal function. This result suggested that exposure increases with decreased renal function although the plasma concentration data in one participant with normal renal function was much lower than for other participants (Supplemental Figure S1, the participant with normal renal function whose data were plotted with black circles). The Cmax and AUC0–inf for the participant were 7.24 μg/ml and 707.0 μg·h/ml, so there might have been a slight effect on the results. As for the statistical analysis, the Cmax, AUC0–inf, and t1/2,z for participants with mild impairment were increased by 1.32-, 1.44-, and 1.19-fold; those for participants with moderate impairment were increased 1.33-, 1.49-, and 1.24-fold; and those for participants with severe impairment were increased by 1.11-, 1.60-, and 1.61-fold compared to that for participants with normal renal function, respectively. These data suggested that the AUC and t1/2,z tended to increase with poorer renal function. On the other hand, considering that the phase 2/3 study demonstrated tolerability of ensitrelvir at 750 mg once followed by 250 mg once daily for 4 days (750/250 mg) [2, 3], which is double the approved dose regimen (375 mg once followed by 125 mg once daily for 4 days, 375/125 mg) [4], there seems to be little concern for safety in patients with renal impairment. Therefore, these findings suggested that the increased AUC level (< 2-fold) would not require dose adjustment in COVID-19 patients with renal impairment.
The unbound fraction was similar across groups (0.0118 to 0.0172) of participants with normal renal function and renal impairment at 3 and 24 h following a single-dose administration, suggesting that the protein binding was independent of ensitrelvir concentration over the range of concentrations evaluated in this study. In addition, the protein binding rate (= [1 − unbound fraction] × 100, i.e., 98.3–98.8%) in humans was similar to that in mice (97.6%) and hamsters (98.3%) [15]. Therefore, it is thought that there are small differences in protein binding between species.
Ensitrelvir would be eliminated from the kidney via glomerular filtration as a free form (not protein-bound form) since it is not a substrate for OCT2, MATE1, and MATE-2K [6]. The unbound fractions at 3 and 24 h after single-dose administration did not differ regardless of the level of renal function, and CLR was also decreased in participants with renal impairment compared to that in participants with normal renal function. On the other hand, Feu did not differ depending on the renal function. This result suggests that there is no difference in oral absorption, hepatic metabolism, and urinary excretion with renal impairment. Since the urinary excretion remains unchanged even if elimination is delayed because of decreased renal function, these results indicated that it is unlikely that hepatic metabolism could replace the delayed elimination due to renal impairment.
The safety of ensitrelvir was assessed with the 32 participants treated in this study. All participants were treated with a single oral dose of ensitrelvir (375 mg). Ensitrelvir was well tolerated in participants with renal impairment. The administration of ensitrelvir (375 mg) in renal impairment subjects demonstrated acceptable safety and tolerability with no new safety concerns. In total, five participants reported TEAEs. Only vessel puncture site hemorrhage was reported for > 1 participants overall (2 participants, 6.3% [1 participant from mild renal impairment and 1 participant from moderate renal impairment]). Anemia, dry mouth, a decrease in the glomerular filtration rate, and hypertriglyceridemia were each reported by one participant (3.1%). No participants with severe renal impairment or normal renal impairment experienced any TEAEs. Treatment-related TEAEs were reported for two participants (6.3%) overall, one each for the mild renal impairment and moderate renal impairment groups. Treatment-related TEAEs were reported for one participant (3.1%): dry mouth and decreased glomerular filtration rate. All TEAEs and treatment-related TEAEs were categorized as mild or moderate. All treatment-related TEAEs were resolved.
Conclusions
In conclusion, the effect of renal function on the pharmacokinetics of ensitrelvir was evaluated. The AUC of ensitrelvir tended to increase with the degree of renal impairment, but there was no clinically meaningful increase in exposure to ensitrelvir with renal impairment. Thus, no dose adjustment would be required regardless of renal function as the safety at double the dose of the approved dose regimen was confirmed. Also, a single 375-mg oral dose of ensitrelvir was well tolerated in participants with mild to severe renal impairment and in those with normal renal function. These findings provide valuable information for the clinical use of ensitrelvir in COVID-19 patients with renal impairment.
Data Availability
The datasets generated and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
Unoh Y, Uehara S, Nakahara K, et al. Discovery of S-217622, a noncovalent oral SARS-CoV-2 3CL protease inhibitor clinical candidate for treating COVID-19. J Med Chem. 2022;65(9):6499–512.
Mukae H, Yotsuyanagi H, Ohmagari N, et al. Efficacy and safety of ensitrelvir in patients With mild-to-moderate coronavirus disease 2019: the phase 2b part of a randomized, placebo-controlled, phase 2/3 study. Clin Infect Dis. 2023;76(8):1403–11. https://doi.org/10.1093/cid/ciac933.
Yotsuyanagi H, Ohmagari N, Doi Y, et al. A phase 2/3 study of S-217622 in participants with SARS-CoV-2 infection (phase 3 part). Medicine (Baltimore). 2023;102(8): e33024. https://doi.org/10.1097/MD.0000000000033024.
Xocova® (Ensitrelvir Fumaric Acid) tablets 125 mg approved in Japan for the treatment of SARS-CoV-2 infection, under the emergency regulatory approval system [press release, 22 Nov 2022. https://www.shionogi.com/global/en/news/2022/11/e20221122.html. Accessed 17 Dec 2022.
Shimizu R, Sonoyama T, Fukuhara T, Kuwata A, Matsuo Y, Kubota R. Safety, tolerability, and pharmacokinetics of the novel antiviral agent ensitrelvir fumaric acid, a SARS-CoV-2 3CL protease inhibitor, in healthy adults. Antimicrob Agents Chemother. 2022;66(10):e00632-e722. https://doi.org/10.1128/aac.00632-22.
Shimizu R, Matsuzaki T, Oka R, et al. Evaluation of drug-drug interactions of ensitrelvir, a SARS-CoV-2 3CL protease inhibitor, with transporter substrates based on in vitro and clinical studies. J Clin Pharmacol. 2023;63(8):918–27. https://doi.org/10.1002/jcph.2247. (Epub 2023 May 10).
Highlights of prescribing information for Paxlovid. https://www.accessdata.fda.gov/drugsatfda_docs/label/2023/217188s000lbl.pdf. Accessed 10 Nov 2023.
Highlights of prescribing information for Fetroja. https://www.accessdata.fda.gov/drugsatfda_docs/label/2020/209445s002lbl.pdf. Accessed 10 Nov 2023.
Highlights of prescribing information for Tricor. https://www.accessdata.fda.gov/drugsatfda_docs/label/2019/021656s029lbl.pdf. Accessed 10 Nov 2023.
FDA Guidance for Industry. Pharmacokinetics in patients with impaired renal function: study design, data analysis, and impact on dosing and labeling. September 2020. https://www.fda.gov/media/78573/download
Levey SA, Coresh J, Greene T, et al. Using standardized serum creatinine values in the modification of diet in renal disease study equation for estimating glomerular filtration rate. Ann Intern Med. 2006;145(4):247–54. https://doi.org/10.7326/0003-4819-145-4-200608150-00004.
WMA Declaration of Helsinki—ethical principles for medical research involving human subjects. https://www.wma.net/policies-post/wma-declaration-of-helsinki-ethical-principles-for-medical-research-involving-human-subjects/. Accessed 23 Sep 2022.
Council for International Organizations of Medical Sciences. International Ethical Guidelines for Health-related Research Involving Humans. https://cioms.ch/wp-content/uploads/2017/01/WEB-CIOMS-EthicalGuidelines.pdf. Accessed 23 Sep 2022.
ICH International Council for Harmonisation. Efficacy guidelines. https://www.ich.org/page/efficacy-guidelines. Accessed 23 Sep 2022.
Kuroda T, Nobori H, Fukao K, et al. Efficacy comparison of 3CL protease inhibitors ensitrelvir and nirmatrelvir against SARS-CoV-2 in vitro and in vivo. J Antimicrob Chemother. 2023;78(4):946–52.
Acknowledgements
We thank all the study participants and their families, investigators, and study teams.
Authorship.
All authors meet the International Committee of Medical Journal Editors (ICMJE) criteria for authorship for this article, take responsibility for the integrity of the work as a whole, and have given their approval for this version to be published.
Funding
This study was funded by Shionogi & Co., Ltd., including the journal’s Rapid Service Fee.
Author information
Authors and Affiliations
Contributions
All authors, Takayuki Katsube, Kezbor Safwan, Ryosuke Shimizu, and Ryuji Kubota, contributed to the conception and design of the study. Takayuki Katsube and Kezbor Safwan contributed to the acquisition and analysis of data. Takayuki Katsube, Kezbor Safwan, and Ryosuke Shimizu contributed to drafting the manuscript. All authors contributed to the interpretation of data, critically revising the manuscript for important intellectual content, and approve the manuscript for publication.
Corresponding author
Ethics declarations
Conflict of interest
Takayuki Katsube, Ryosuke Shimizu, and Ryuji Kubota are employees of Shionogi & Co., Ltd. Kezbor Safwan is an employee of Shionogi Inc.
Ethical approval
This study (NCT05363215) was conducted in accordance with the protocol. The study protocol was approved by the Declaration of Helsinki and Council for International Organizations of Medical Sciences International Ethical Guidelines, the Institutional Review Board, the International Council for Harmonisation of Technical Requirements for Pharmaceuticals for Human Use Good Clinical Practice Guidelines, and other regulations and applicable laws. The Institutional Review Board also approved the study. All participants in this study gave their written informed consent for participation [12,13,14].
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Katsube, T., Kezbor, S., Shimizu, R. et al. Effect of Renal Impairment on Pharmacokinetics and Safety of Ensitrelvir, a SARS-CoV-2 3CL Protease Inhibitor. Infect Dis Ther 13, 597–607 (2024). https://doi.org/10.1007/s40121-024-00946-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40121-024-00946-x