Summary
Abstract
Reteplase (Retavase®) is a plasminogen activator, mimicking endogenous tissue plasminogen activator (t-PA), a serine protease, converting plasminogen to plasmin and thereby precipitating thrombolysis. It is a third-generation recombinant form of t-PA that operates in the presence of fibrin (i.e. it is fibrin specific).
Reteplase can be administered as a bolus dose (nonweight-based) rather than an infusion, which promotes rapid and safe administration. The ease of administration of this reteplase dosage regimen (two 10U bolus doses, each over 2 minutes, 30 minutes apart) is conducive to prehospital initiation of thrombolytic treatment in patients with ST-segment elevation myocardial infarction (STEMI), which reduces the time to treatment, a critical factor in improving long-term survival.
In large randomized clinical trials of patients with STEMI, reteplase was superior to alteplase for coronary artery patency (according to TIMI [thrombolysis in myocardial infarction] flow) at 60 and 90 minutes, but there was no significant difference between agents for mortality rate and incidence of intracranial bleeding. The 35-day mortality rates were equivalent for reteplase and streptokinase recipients; there was reduced incidence of some cardiac events with reteplase versus streptokinase, but a greater incidence of hemorrhagic stroke.
Reteplase has also shown thrombolytic efficacy (in nonapproved indications) as a catheter-directed intra-arterial or intravenous infusion for peripheral vessel occlusions, as 5-minute bolus doses (in 1U increments) for acute ischemic stroke, as a low-dose solution for occluded catheters or grafts, and as an intravenous double bolus for massive pulmonary embolism. Across studies in these indications, the incidence of bleeding complications associated with reteplase treatment appeared to be similar to that associated with other thrombolytic agents.
With its efficacy, and the ease of administration of the bolus doses potentially minimizing dosage errors when treatment is administered under time pressure, reteplase is a valuable option for pre- or in-hospital thrombolytic treatment in patients with STEMI, and is a useful thrombolytic for the treatment of the other thrombotic occlusive disorders described.
Pharmacoloaic Properties
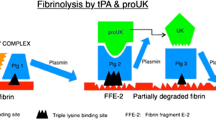
Reteplase, a single-chain, nonglycosylated peptide, is a fibrin-specific recombinant plasminogen activator that contains the kringle 2 and protease domains of native t-PA, but lacks the kringle 1, fibronectin finger, and epidermal growth factor domains. It exerts its thrombolytic action by catalyzing the conversion of the inactive proenzyme plasminogen to the active protease plasmin, which degrades the fibrin matrix of the thrombus. Reteplase has a fibrin-specific activity and, in animal models of thrombosis, is a more potent thrombolytic than alteplase, and produces reperfusion significantly faster than alteplase, streptokinase, or urokinase. In patients with acute myocardial infarction (AMI), reteplase decreased levels of fibrinogen, plasminogen, and α2-antiplasmin. In these patients, a double-bolus (10U + 10U; 30 minutes apart) dose of reteplase produced relatively greater alterations in hemostatic variables than a single bolus (10U) dose. A paradoxical activation of the coagulation system seen after reteplase treatment is blunted in a beneficial fashion when reduced-dose reteplase is combined with abciximab in AMI patients.
Pharmacokinetic studies in healthy volunteers have suggested that not all of the reteplase antigen in plasma was active. In healthy volunteers, the apparent volume of distribution of reteplase activity during the terminal elimination phase was ≈ 6L, which, like that of alteplase, approximates plasma volume. Reteplase has a longer activity half-life (12.6 minutes) than that of alteplase (<5 minutes), and is cleared via the kidneys and liver.
Therapeutic Efficacy
Patients with acute STEMI receiving reteplase, administered as two intravenous 10U bolus doses 30 minutes apart, achieved superior patency rates at 60 and 90 minutes after treatment initiation compared with alteplase recipients (in terms of TIMI [thrombolysis in myocardial infarction] grade 2 or 3, or grade 3 flow) in the RAPID II study, and similar patency rates (TIMI grade 2 or 3 flow) to those of alteplase recipients in the RAPID I trial. However, the 30-day mortality rates for these two agents were not significantly different in the GUSTO III study (7.47% vs 7.24%). The 35-day mortality rates for reteplase and streptokinase recipients in the INJECT study were considered equivalent (9.02% vs 9.53%), based on the rate with reteplase being ≤1% lower than that for streptokinase and the upper limit of the confidence interval ≤1%.
The shorter the time to reperfusion for patients with STEMI the greater the survival rate; reteplase treatment reduced the median door-to-needle time by 32 minutes in the ER-TIMI 19 study, which also led to earlier ST-segment resolution.
Including the antiplatelet agent abciximab in the reteplase regimen and halving the reteplase dose (in the GUSTO V trial of patients with STEMI) maintained efficacy relative to full-dose reteplase monotherapy but provided little benefit. There was no between-group difference in the 30-day mortality rate (5.6% vs 5.9%), thereby demonstrating the noninferiority of combination therapy versus full-dose monotherapy. There was also no difference between treatment groups for 1-year mortality. However, patients receiving combination treatment had a significantly lower combined incidence of death or nonfatal reinfarction (7.4% vs 8.8%; p = 0.0011), and a lower incidence of urgent (i.e. within 6 hours) percutaneous coronary intervention (PCI) than the monotherapy group (5.6% vs 8.6%; p < 0.0001), and they also experienced significantly fewer complications of MI up to day 7.
The combination of reteplase (half-dose) and abciximab facilitated PCI in patients with STEMI; at 30 days, there was clinical success (freedom from death, reinfarction, urgent revascularization, major bleeding, or transfusion) in 85.4% of patients who underwent early (at time of first angiography) PCI and in 70.4% of those who did not undergo early PCI.
In patients with peripheral arterial thrombotic occlusions, intra-arterial administration of catheter-directed reteplase 0.25 U/h infused for a mean ≈29 hours was associated with thrombolytic success in 84% of procedures. The benefit of adding abciximab (0.25 mg/kg bolus, then 0.125 μg/kg/min [maximum 10 μg/min] as a 12-hour infusion) to a reteplase regimen (0.1–1.0 U/h) for peripheral vessel occlusions was demonstrated in the RELAX trial by rates of complete thrombolysis of 50–80% versus 16–50% with reteplase alone, and shorter median infusion times (17–28 hours vs 22.5–42 hours). The combination of reteplase with abciximab had similar recanalization rates to those of urokinase with abciximab (each combination administered as an intra-arterial, catheter-directed pulsed spray), but the mean infusion time was longer with the reteplase combination (APART trial).
Intra-arterial reteplase administered up to 9 hours after symptom onset has demonstrated efficacy in acute ischemic stroke in small noncomparative studies, and there are preliminary investigations of the combination of reteplase and abciximab in this indication. Results of preliminary noncomparative studies also suggest efficacy, with few complications, for low-dose reteplase for the restoration of blood flow in occluded central venous catheters or hemodialysis catheters and grafts, and limited data suggest similar efficacy for reteplase (intravenous double-bolus dose) and alteplase (infusion over 2 hours) in patients with massive pulmonary embolism.
Tolerability
As With other systemic thrombolytic therapies, bleeding (intracranial bleeding, hemorrhagic stroke, other internal bleeding, and superficial bleeding from puncture/catheter or surgical sites) constitutes a serious safety issue, and is the most common adverse effect of reteplase administration. The proportions of patients with STEMI experiencing at least one bleed were similar for reteplase (10U + 10U) and comparators (15.8% vs 16.6% streptokinase recipients [INJECT study], 30.5% vs 30.8% of alteplase recipients [GUSTO III study], and 47.4% vs 47.9% of alteplase recipients [pooled results of the angiographic RAPID trials]). Overall, the puncture/ injection site was generally the most common bleeding site associated with full-dose reteplase therapy, but these bleeds were mild.
Reteplase and alteplase recipients experienced similar incidences of intracranial hemorrhage or severe or life-threatening bleeding in the large GUSTO III trial, despite a numerically and relatively lower incidence of intracranial hemorrhage with reteplase than with alteplase in the earlier smaller (RAPID) trials of vessel patency. The incidence, severity and sites of other bleeding events were similar for reteplase and alteplase in these trials.
Compared with streptokinase, reteplase was associated with a higher incidence of hemorrhagic stroke, but the incidence, severity, and site of other bleeding events was similar for both agents (INJECT study in patients with STEMI).
Also in patients with STEMI, half-dose reteplase with abciximab was associated with a similar incidence of intracranial bleeding to that of full-dose reteplase monotherapy, but a greater incidence of nonintracranial bleeding.
In patients with peripheral arterial occlusions, the incidence of major bleeding complications with reteplase monotherapy administered for thrombolysis increased with dose. The addition of abciximab to the reteplase regimen in the RELAX trial was associated with a numerically greater incidence of major bleeding and need for blood transfusion compared with reteplase alone. Major complications (including bleeding) at 30 days occurred in numerically fewer recipients of a reteplase and abciximab combination than in recipients of urokinase plus abciximab, although there were more minor complications associated with the reteplase combination.





Similar content being viewed by others
Notes
The use of trade names is for identification purposes only and does not imply endorsement.
References
Feied C, Handler JA. Thrombolytic therapy [online]. Available from URL: http://www.emedicine.com [Accessed 2006 May 18].
Deitcher SR, Jaff MR. Pharmacologic and clinical characteristics of thrombolytic agents. Rev Cardiovasc Med 2002; 3 Suppl 2: S25–33.
American Heart Association. American Stroke Association. Heart Disease and Stroke Statistics. 2006 Update, [online]. Available from URL: http://www.americanheart.org [Accessed 2006 May 2].
Millan M, Davalos A. The need for new therapies for acute ischaemic stroke. Cerebrovasc Dis 2006; 22 Suppl. 1: 3–9.
Goldhaber SZ, Bounameaux H. Thrombolytic therapy in pulmonary embolism. Semin Vasc Med 2001; 1(2): 213–20.
Goldhabër SZ, Visani L, De Rosa M. Acute pulmonary embolism: clinical outcomes in the International Cooperative Pulmonary Embolism Registry (ICOPER). Lancet 1999 Apr 24; 353(9162): 1386–9.
Protein Design Labs Inc.. Retavase®. Prescribing information. Fremont (CA): PDL Biopharma Inc., 2005 Dec.
Noble S, McTavish D. Reteplase: a review of its pharmacological properties and clinical efficacy in the management of acute myocardial infarction. Drugs 1996 Oct; 52: 589–605.
Moser M, Kohler B, Schmittner M, et al. Recombinant plasminogen activators: a comparative review of the clinical pharmacology and therapeutic use of alteplase and reteplase. Biodrugs 1998 Jun; 9: 455–63.
Martin U, Kaufmann B, Neugebauer G. Current clinical use of reteplase for thrombolysis: a pharmacokinetic-pharmacodynamic perspective. Clin Pharmacokinet 1999 Apr; 36: 265–76.
Martin U, Sponer G, Strein K. Differential fibrinolytic properties of the recombinant plasminogen activator BM 06.022 in human plasma and blood clot systems in vitro (italics). Blood Coagul Fibrinolysis 1993; 4: 235–42.
Fischer S, Kohnert U. Major mechanistic differences explain the higher clot lysis potency of reteplase over alteplase: lack of fibrin binding is an advantage for bolus application of fibrin-specific thrombolytics. Fibrinolysis Proteolysis 1997 May; 11: 129–35.
Martin U, Sponer G, Strein K. Evaluation of thrombolytic and systemic effects of the novel recombinant plasminogen activator BM 06.022 compared with alteplase, anistreplase, streptokinase and urokinase in a canine model of coronary artery thrombosis. J Am Coll Cardiol 1992; 19: 433–40.
Grunewald M, Muller M, Ellbruck D, et al. Double- versus single-bolus thrombolysis with reteplase for acute myocardial infarction: a pharmacokinetic and pharmacodynamic study. Fibrinolysis Proteolysis 1997 May; 11: 137–45.
Moser M, Nordt T, Peter K, et al. Platelet function during and after thrombolytic therapy for acute myocardial infarction with reteplase, alteplase, or streptokinase. Circulation 1999 Nov 2; 100: 1858–64.
Gurbel PA, Serebruany VL, Shustov AR, et al. Effects of reteplase and alteplase on platelet aggregation and major receptor expression during the first 24 hours of acute myocardial infarction treatment. J Am Coll Cardiol 1998 Jun; 31: 1466–73.
Coulter SA, Cannon CP, Ault KA, et al. High levels of platelet inhibition with abciximab despite heightened platelet activation and aggregation during thrombolysis for acute myocardial infarction: results from TIMI (Thrombolysis in Myocardial Infarction) 14. The TIMI 14 Platelet Substudy Investigators. Circulation 2000 Jun 13; 101: 2690–5.
Merlini PA, Repetto A, Andreoli AM, et al. Effect of abciximab on prothrombin activation and thrombin generation in patients with acute myocardial infarction also receiving reteplase. Am J Cardiol 2004 Jan 15; 93(2): 195–8.
Hoffmeister HM, Kastner C, Szabo S, et al. Fibrin specificity and procoagulant effect related to the kallikrein-contact phase system and to plasmin generation with double-bolus reteplase and front-loaded alteplase thrombolysis in acute myocardial infarction. Am J Cardiol 2000 Aug 1; 86: 263–8.
Szabo S, Etzel D, Ehlers R, et al. Combined thrombolysis with abciximab favourably influences platelet-leukocyte interactions and platelet activation in acute myocardial infarction. J Thromb Thrombolysis 2005 Dec; 20(3): 155–61.
Martin U, von Möllendorff E, Akpan W, et al. Pharmacokinetic and hemostatic properties of the recombinant plasminogen activator BM 06.022 in healthy volunteers. Thromb Haemost 1991; 66: 569–74.
Martin U, von Möllendorff E, Akpan W, et al. Dose-ranging study of the novel recombinant plasminogen activator BM 06.022 in healthy volunteers. Clin Pharmacol Ther 1991; 50: 429–36.
Genentech Inc. Activase® (alteplase, a recombinant tissue plasminogen activator). Prescribing Information. 2002.
Kuiper J, van de Bilt H, Martin U, et al. Uptake, internalization and degradation of the novel plasminogen activator reteplase (BM 06.022) in the rat. Thromb Haemost 1995; 74: 1501–10.
Centocor. Investigator’s brochure. Reteplase (Retavase®). Horsham (PA): Centocor Inc., 2004 Jul.
Smalling RW, Bode C, Kalbfleisch J. More rapid, complete, and stable coronary thrombolysis with bolus administration of reteplase compared with alteplase infusion in acute myocardial infarction. Circulation 1995; 91: 2725–32.
Global Use of Strategies to Open Occluded Coronary Arteries (GUSTO III) Investigators. A comparison of reteplase with alteplase for acute myocardial infarction. Global Use of Strategies to Open Occluded Coronary Arteries (GUSTO III) Investigators. N Engl J Med 1997 Oct 16; 337: 1118–23.
The GUSTO V Investigators. Reperfusion therapy for acute myocardial infarction with fibrinolytic therapy or combination reduced fibrinolytic therapy and platelet glycoprotein IIb/IIIa inhibition: the GUSTO V randomised trial. Lancet 2001 Jun 16; 357: 1905–1914.
Trial of abciximab with and without low-dose reteplase for acute myocardial nfarction. Strategies for Patency Enhancement in the Emergency Department (SPEED) group. Circulation 2000; 101: 2788–94.
Randomised, double-blind comparison of reteplase double-bolus administration with streptokinase in acute myocardial infarction (INJECT): trial to investigate equivalence. International Joint Efficacy Comparison of Thrombolytics [published erratum appears in Lancet 1995 Oct 7; 346 (8980): 980]. Lancet 1995; 346(8971): 329–36.
Bode C, Smalling RW, Berg G, et al. Randomized comparison of coronary thrombolysis achieved with double bolus reteplase (r-PA) and front-loaded, “accelerated” alteplase (rt-PA) in patients with acute myocardial infarction. Circulation 1996 Sep 1; 94(5): 891–8.
Antman EM, Gibson CM, de Lemos JA, et al. Combination reperfusion therapy with abciximab and reduced dose reteplase: results from TIMI 14. The TIMI 14 Investigators. Eur Heart J 2000 Dec; 21(23): 1944–53.
Morrow DA, Antman EM, Sayah A, et al. Evaluation of the time saved by prehospital initiation of reteplase for ST-elevation myocardial infarction: results of the Early Retavase-Thrombolysis In Myocardial Infarction (ER-TIMI) 19 Trial. The Early Retavase-Thrombolysis In Myocardial Infarction (ER-TIMI) 19 Investigators. J Am Coll Cardiol 2002 Jul 3; 40: 71–7.
Herrmann HC, Moliterno DJ, Ohman EM, et al. Facilitation of early percutaneous coronary intervention after reteplase with or without abciximab in acute myocardial infarction: results from the SPEED (GUSTO-4 Pilot) trial. J Am Coll Cardiol 2000 Nov 1; 36: 1489–96.
Tebbe U, von Essen R, Smolarz A, et al. Open, noncontrolled dose-finding study with a novel recombinant plasminogen activator (BM 06.022) given as a double bolus in patients with acute myocardial infarction. Am J Cardiol 1993; 72: 518–24.
Neuhaus K-L, von Essen R, Vogt A, et al. Dose finding with a novel recombinant plasminogen activator (BM 06.022) in patients with acute myocardial infarction: results of the German Recombinant Plasminogen Activator Study. J Am Coll Cardiol 1994; 24: 55–60.
Rosenberg DG, Levin E, Lausell A, et al. Feasibility and timing of prehospital administration of reteplase in patients with acute myocardial infarction. J Thromb Thrombolysis 2002 Jun; 13: 147–53.
Lamfers EJP, Schut A, Hooghoudt TEH, et al. Prehospital thrombolysis with reteplase: the Nijmegen/Rotterdam study. Am Heart J 2003 Sep; 146(3): 479–83.
Hampton JR. Mega-trials and equivalence trials: experience from the INJECT study. Eur Heart J 1996 Sep; 17 (Suppl. E): 28–34.
Wilcox RG. Clinical trials in thrombolytic therapy: what do they tell us? INJECT 6-month outcomes data. Am J Cardiol 1996 Dec 19; 78 Suppl. 12A: 20–3.
Topol EJ, Ohman EM, Armstrong PW, et al. Survival outcomes 1 year after reperfusion therapy with either alteplase or reteplase for acute myocardial infarction: results from the Global Utilization of Streptokinase and t-PA for Occluded Coronary Arteries (GUSTO) III trial. The GUSTO-III Investigators. Circulation 2000 Oct 10; 102: 1761–5.
Anderson RD, White HD, Ohman EM, et al. Predicting outcome after thrombolysis in acute myocardial infarction according to ST-segment resolution at 90 minutes: a substudy of the GUSTO-III trial. Global Use of Strategies To Open occluded coronary arteries. Am Heart J 2002 Jul; 144(1): 81–8.
White HD, Anderson RD, Weaver WD, et al. Resolution of ST-segment elevation with reteplase vs alteplase: results from the GUSTO-III ECG substudy [abstract no. 1846]. Circulation 1997 Oct 21; 96(8 Suppl.): 1–331.
Hasdai D, Holmes Jr DR, Topol EJ, et al. Frequency and clinical outcome of cardiogenic shock during acute myocardial infarction among patients receiving reteplase or alteplase: results from GUSTO-III. Eur Heart J 1999 Jan; 20: 128–35.
Antman EM, Giugliano RP, Gibson CM, et al. Abciximab facilitates the rate and extent of thrombolysis: results of the thrombolysis in myocardial infarction (TIMI) 14 trial. The TIMI 14 Investigators. Circulation 1999 Jun 1; 99(21): 2720–32.
Lincoff AM, Califf RM, Van de Werf F, et al. Mortality at 1 year with combination platelet glycoprotein IIb/IIIa inhibition and reduced-dose fibrinolytic therapy vs conventional fibrinolytic therapy for acute myocardial infarction: GUSTO V randomized trial. The GUSTO V Investigators. JAMA 2002 Nov 6; 288: 2130–5.
Thiele H, Engelmann L, Elsner K, et al. Comparison of pre-hospital combination-fibrinolysis plus conventional care with pre-hospital combination-fibrinolysis plus facilitated percutaneous coronary intervention in acute myocardial infarction. Eur Heart J 2005 Oct; 26(19): 1956–63.
Kiproff PM, Yammine K, Potts JMS, et al. Reteplase infusion in the treatment of acute lower extremity occlusions. J Thromb Thrombolysis 2002 Apr; 13: 75–9.
Kam AW, Amersur NB, Zajko AB, et al. Reteplase in the treatment of acute peripheral arterial occlusions: experience in 47 cases over 18 months [abstract no. 26]. J Vasc Interv Radiol 2002; 13: S10.
Parikh SR, Ferguson GS, Eglin TA, et al. Thrombolytic therapy in lower extremity arterial occlusions with reteplase (rPA) [abstract no. 25]. J Vasc Interv Radiol 2002; 13: S10.
Hanover TM, Kalbaugh CA, Gray BH, et al. Safety and efficacy of reteplase for the treatment of acute arterial occlusion: complexity of underlying lesion predicts outcome. Ann Vasc Surg 2005 Nov; 19(6): 817–22.
Davidian MM, Powell A, Benenati JF, et al. Initial results of reteplase in the treatment of acute lower extremity arterial occlusions. J Vasc Interv Radiol 2000 Mar; 11: 289–94.
Ouriel K, Katzen B, Mewissen M, et al. Reteplase in the treatment of peripheral arterial and venous occlusions: a pilot study. J Vasc Interv Radiol 2000; 11(7): 849–54.
Castaneda F, Swischuk JL, Li RZ, et al. Declining-dose study of reteplase treatment for lower extremity arterial occlusions. J Vasc Interv Radiol 2002 Nov; 13: 1093–8.
Ouriel K, Castaneda F, McNamara T, et al. Reteplase monotherapy and reteplase/ abciximab combination therapy in peripheral arterial occlusive disease: results from the RELAX trial. J Vasc Interv Radiol 2004 Mar; 15(3): 229–38.
Tepe G, Hopfenzitz C, Dietz K, et al. Peripheral Arteries: Treatment with Antibodies of Platelet Receptors and Reteplase for Thrombolysis — APART Trial. Radiology 2006; 239(3): 892–900.
Castaneda F, Li R, Young K, et al. Catheter-directed thrombolysis in deep venous thrombosis with use of reteplase: immediate results and complications from a pilot study. J Vasc Interv Radiol 2002 Jun; 13(6): 577–80.
Grunwald MR, Hofmann LV. Comparison of urokinase, alteplase, and reteplase for catheter-directed thrombolysis of deep venous thrombosis. J Vasc Interv Radiol 2004 Apr; 15(4): 347–52.
Drescher P, Crain MR, Rilling WS. Initial experience with the combination of reteplase and abciximab for thrombolytic therapy in peripheral arterial occlusive disease: a pilot study. J Vasc Interv Radiol 2002 Jan; 13: 37–43.
Drescher P, McGuckin J, Rilling WS, et al. Catheter-directed thrombolytic therapy in peripheral artery occlusions: combining reteplase and abciximab. Am J Roentgenol 2003 May; 180(5): 1385–91.
Barr JD, Loges R, Magdinec M. Intraarterial reteplase infusion for acute stroke intervention: inital experience [abstract no. 31]. J Vasc Interv Radiol 2000; 12(2 Pt 2): S13.
Qureshi AI, Ali Z, Suri MFK, et al. Intra-arterial third-generation recombinant tissue plasminogen activator (reteplase) for acute ischemic stroke. Neurosurgery 2001 Jul; 49: 41–48.
Qureshi AI, Siddiqui AM, Suri MF, et al. Aggressive mechanical clot disruption and low-dose intra-arterial third-generation thrombolytic agent for ischemic stroke: a prospective study. Neurosurgery 2002 Nov; 51(5): 1319–27; discussion 1327–9.
Qureshi AI, Siddiqui AM, Kim SH, et al. Reocclusion of recanalized arteries during intra-arterial thrombolysis for acute ischemic stroke. Am J Neuroradiol 2004 Feb; 25(2): 322–8.
Qureshi AI, Kirmani JF, Janjua N, et al. A prospective study to assess the safety and efficacy of intra-arterial reteplase and intravenous abciximab in patients with acute ischemic stroke. Stroke 2006 Feb 1; 37(2): 705.
Warach S, Butman J, Davis L, et al. Reopro Retavse Reperfusion of Stroke Safety Study — Imaging Evaluation (ROSIE): interim safety and efficacy results [abstract no. LB1]. International Stroke Conference; 2006 Feb 16–18; Kissimmee (FL).
Liu CY, Jain V, Shields AF, et al. Efficacy and safety of reteplase for central venous catheter occlusion in patients with cancer. J Vasc Interv Radiol 2004 Jan; 15(1 Pt 1): 39–44.
Owens L. Reteplase for clearance of occluded venous catheters. Am J Health Syst Pharm 2002 Sep 1; 59(17): 1638–40.
Castner D. The efficacy of reteplase in the treatment of thrombosed hemodialysis venous catheters. Nephrol Nurs J 2001 Aug; 28(4): 403–19 passim.
Falk A, Samson W, Uribarri J, et al. Efficacy of reteplase in poorly functioning hemodialysis catheters. Clin Nephrol 2004 Jan; 61(1): 47–53.
Hyman G, England M, Kibede S, et al. The efficacy and safety of reteplase for thrombolysis of hemodialysis catheters at a community and academic regional medical center. Nephron Clin Pract 2004; 96(2): c39–42.
Terrill KR, Lemons RS, Goldsby RE. Safety, dose, and timing of reteplase in treating occluded central venous catheters in children with cancer. J Pediatr Hematol Oncol 2003 Nov; 25(11): 864–7.
Hilleman DE, Dunlay RW, Packard KA. Reteplase for dysfunctional hemodialysis catheter clearance. Pharmacotherapy 2003 Feb; 23: 137–41.
Hilleman DE, Lanspa TJ, Lenz TL. Pulse-spray pharmacomechanical thrombolysis (PSPMT) of clotted hemodialysis grafts with reteplase (RPA) [abstract no. 321]. J Vasc Interv Radiol 2002; 13(2 Pt 2): S109.
Gibbens D, Depalma J, Albanese J, et al. Percutaneous thrombolysis of hemodialysis grafts using reteplase [abstract no. 202]. J Vasc Interv Radiol 2000; 11(2 Pt 2): 250.
Flick PA, Das M, Horton K, et al. Initial experience with reteplase using the ‘lyse and wait’ technique in thrombosed dialysis grafts [abstract no. 207]. J Vasc Interv Radiol 2000; 11(2 Pt 2): 252.
Falk A, Guller J, Nowakowski FS, et al. Reteplase in the treatment of thrombosed hemodialysis grafts. J Vasc Interv Radiol 2001 Nov; 12: 1257–62.
Tebbe U, Graf A, Kamke W, et al. Hemodynamic effects of double bolus reteplase versus alteplase infusion in massive pulmonary embolism. Am Heart J 1999 Jul; 138(1 Pt 1): 39–44.
Savonitto S, Armstrong PW, Lincoff AM, et al. Risk of intracranial haemorrhage with combined fibrinolytic and glycoprotein IIb/IIIa inhibitor therapy in acute mycocardial infarction: dichotomous response as a function of age in the GUSTO V trial. Eur Heart J 2003 Oct; 24(20): 1807–14.
McNamara TO, Dong P, Chen J, et al. Bleeding complications associated with the use of rt-PA versus r-PA for peripheral arterial and venous thromboembolic occlusions. Tech Vasc Interv Radiol 2001; 4(2): 92–8.
Antman EM, Anbe DT, Armstrong PW, et al. ACC/AHA guidelines for the management of patients with ST-elevation myocardial infarction: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Committee to Revise the 1999 Guidelines for the Management of Patients with Acute Myocardial Infarction). Circulation 2004 Aug 31; 110(9): e82–292.
Gillis JC, Wagstaff AJ, Goa KL. Alteplase: a reappraisal of its pharmacological properties and therapeutic use in acute myocardial infarction. Drugs 1995; 50(1): 102–36.
Verstraete M. Third-generation thrombolytic drugs. Am J Med 2000 Jul; 109(1): 52–8.
Khan IA, Gowda RM. Clinical perspectives and therapeutics of thrombolysis. Int J Cardiol 2003 Oct; 91(2–3): 115–27.
Cohen M, Arjomand H, Pollack Jr CV. The evolution of thrombolytic therapy and adjunctive antithrombotic regimens in acute ST-segment elevation myocardial infarction. Am J Emerg Med 2004 Jan; 22(1): 14–23.
Seyedroudbari A, Kessler ER, Mooss AN, et al. Time to treatment and cost of thrombolysis: a multicenter comparison of tPA and rPA. J Thromb Thrombolysis 2000 Apr; 9(3): 303–8.
Boersma E, Mercado N, Poldermans D, et al. Acute myocardial infarction. Lancet 2003 Mar 8; 361(9360): 847–58.
Ellis K, Brener S. New fibrinolytic agents for MI: as effective as current agents, but easier to administer. Cleve Clin J Med 2004 Jan; 71(1): 20, 23–37 passim.
Eagle KA, Goodman SG, Avezum A, et al. Practice variation and missed opportunities for reperfusion in ST-segment-elevation myocardial infarction: findings from the Global Registry of Acute Coronary Events (GRACE). The GRACE Investigators. Lancet 2002 Feb 2; 359(9304): 373–7.
Hasdai D, Behar L, Wallentin L, et al. A prospective survey of the characteristics, treatments and outcomes of patients with acute coronary syndromes in Europe and the Mediterranean basin: the Euro Heart Survey of Acute Coronary Syndromes (Euro Heart Survey ACS). Eur Heart J 2002; 23: 1190–201.
Keeley EC, Boura JA, Grines CL. Primary angioplasty versus intravenous thrombolytic therapy for acute myocardial infarction: a quantitative review of 23 randomised trials. Lancet 2003 Jan 4; 361(9351): 13–20.
Boersma E. Does time matter? A pooled analysis of randomized clinical trials comparing primary percutaneous coronary intervention and in-hospital fibrinolysis in acute myocardial infarction patients. Eur Heart J 2006 Apr; 27(7): 779–88.
Armstrong PW, Collen D, Antman E. Fibrinolysis for acute myocardial infarction: the future is here and now. Circulation 2003 May 27; 107(20): 2533–7.
Bonnefoy E, Lapostolle F, Leizorovicz A, et al. Primary angioplasty versus prehospital fibrinolysis in acute myocardial infarction: a randomised study. Lancet 2002 Sep 14; 360(9336): 825–9.
Stringer KA. TIMI grade flow, mortality, and the GUSTO-III trial. Pharmacotherapy 1998; 18(4): 699–705.
Antman EM, Cooper HA, Gibson CM, et al. Determinants of improvement in epicardial flow and myocardial perfusion for ST elevation myocardial infarction; insights from TIMI 14 and InTIME-II. The TIMI 14 Investigators. Eur Heart J 2002 Jun; 23(12): 928–33.
McNamara RL, Herrin J, Bradley EH, et al. Hospital improvement in time to reperfusion in patients with acute myocardial infarction, 1999 to 2002. J Am Coll Cardiol 2006 Jan 3; 47(1): 45–51.
Cannon CP, Sayah AJ, Walls RM. ER TIMI-19: testing the reality of prehospital thrombolysis. J Emerg Med 2000 Oct; 19(3 Suppl.): 21S–5S.
Morrison LJ, Verbeek PR, McDonald AC, et al. Mortality and prehospital thrombolysis for acute myocardial infarction: A meta-analysis. JAMA 2000; 283(20): 2686–92.
Bjorklund E, Stenestrand U, Lindback J, et al. Pre-hospital thrombolysis deiveredby paramedics is associated with reduced time delay and mortality in ambulance-transported real-life patients with ST-elevation myocardial infarction. The RIKS-HIA Investigators. Eur Heart J 2006; 27(7): 1146–52.
Dunn CJ, Goa KL. Tenecteplase: a review of its pharmacology and therapeutic efficacy in patients with acute myocardial infarction. Am J Cardiovasc Drug 2001; 1(1): 51–66.
Richards CF, Cannon CP. Reducing medication errors: potential benefits of bolus thrombolytic agents. Acad Emerg Med 2000 Nov; 7(11): 1285–9.
Hall II WL, Larkin GL, Trujillo MJ, et al. Errors in weight estimation in the emergency department: comparing performance by providers and patients. J Emerg Med 2004 Oct; 27(3): 219–24.
An international randomized trial comparing four thrombolytic strategies for acute myocardial infarction. The GUSTO Investigators. N Engl J Med 1993; 329(10): 673–82.
Single-bolus tenecteplase compared with front-loaded alteplase in acute myocardial infarction: the ASSENT-2 double-blind randomised trial. Assessment of the Safety and Efficacy of a new Thrombolytic (ASSENT-2) Investigators. Lancet 1999 Aug 28; 354(9180): 716–22.
Cannon CP, Gibson CM, McCabe CH, et al. TNK-tissue plasminogen activator compared with front-loaded alteplase in acute myocardial infarction: results of the TIMI 10B trial. Thrombolysis in Myocardial Infarction (TIMI) 10B Investigators. Circulation 1998 Dec 22-1998; 98(25): 2805–14.
Menon V, Harrington RA, Hochman JS, et al. Thrombolysis and adjunctive therapy in acute myocardial infarction: the Seventh ACCP Conference on Antithrombotic and Thrombolytic Therapy. Chest 2004 Sep; 126(3 Suppl): 549S–75S.
Cannon CP. Thrombolysis medication errors: benefits of bolus thrombolytic agents. Am J Cardiol 2000 Apr 27; 85(8A): 17C–22C.
Askari AT, Lincoff AM. GUSTO V: combination drug treatment of acute myocardial infarction. Global Use of Strategies to Open Occluded Coronary Arteries. Cleve Clin J Med 2002 Jul; 69(7): 554–60.
Perler B. Thrombolytic therapies: the current state of affairs. J Endovasc Ther 2005 Apr; 12(2): 224–32.
Grines CL, Serruys P, O’Neill WW. Fibrinolytic therapy: is it a treatment of the past? Circulation 2003 May 27; 107(20): 2538–42.
Dauerman HL, Sobel BE. Synergistic treatment of ST-segment elevation myocardial infarction with pharmacoinvasive recanalization. J Am Coll Cardiol 2003 Aug 20; 42(4): 646–51.
Stone GW, Gersh BJ. Facilitated angioplasty: paradise lost [comment]. Lancet 2006 Feb 18; 367(9510): 543–6.
Primary versus tenecteplase-facilitated percutaneous coronary intervention in patients with ST-segment elevation acute myocardial infarction (ASSENT-4 PCI): randomised trial. Assessment of the Safety and Efficacy of a New Treatment Strategy with Percutaneous Coronary Intervention (ASSENT-4 PCI) investigators. 2006 Feb 18; 367 (9510): 569–578.
Keeley EC, Boura JA, Grines CL, et al. Comparison of primary and facilitated percutaneous coronary interventions for ST-elevation myocardial infarction: quantitative review of randomised trials [published erratum appears in Lancet 2006 May 20: 367 (9523): 1656]. Lancet 2006; 367(9510): 579–88.
Ellis SG, Armstrong P, Betriu A, et al. Facilitated percutaneous coronary intervention versus primary percutaneous coronary intervention: design and rationale of the Facilitated Intervention with Enhanced Reperfusion Speed to Stop Events (FINESSE) trial. The FINESSE Investigators. Am Heart J 2004 Apr; 147(4): E16.
Gersh BJ, Antman EM. Selection of the optimal reperfusion strategy for STEMI: does time matter? Eur Heart J 2006; 27(7): 761–3.
Ellis SG, da Silva ER, Hyndrickx G, et al. Randomized comparison of rescue angioplasty with conservative management of patients with early failure of thrombolysis for acute anterior myocardial infarction. Circulation 1994; 90: 2280–4.
Sutton AG, Campbell PG, Graham R, et al. A randomized trial of rescue angioplasty versus a conservative approach for failed fibrinolysis in ST-segment elevation myocardial infarction: the Middlesbrough Early Revascularization to Limit INfarction (MERLIN) trial. J Am Coll Cardiol 2004 Jul 21; 44(2): 287–96.
Gershlick AH, Stephens-Lloyd A, Hughes S, et al. Rescue angioplasty after failed thrombolytic therapy for acute myocardial infarction. N Engl J Med 2005 Dec 29; 353(26): 2758–68.
Steg PG, Francois L, Lung B, et al. Long-term clinical outcomes after rescue angioplasty are not different from those of successful thrombolysis for acute myocardial infarction. Eur Heart J 2005; 26: 1831–7.
Miller JM, Smalling R, Ohman EM, et al. Effectiveness of early coronary angioplasty and abciximab for failed thrombolysis (reteplase or alteplase) during acute myocardial infarction (results from the GUSTO-III trial). Am J Cardiol 1999 Oct 1; 84: 779–84.
Hirsch AT, Haskal ZJ, Hertzer NR, et al. ACC/AHA guidelines for the management of patients with peripheral arterial disease (lower extremity, renal, mesenteric and abdominal aortic): executive summary. J Am Coll Cardiol 2006; 47(6): 1239–312.
Mahler F, Schneider E, Hess H. Recombinant tissue plasminogen activator versus urokinase for local thrombolysis of femoropopliteal occlusions: a prospective, randomized multicenter trial. J Endovasc Ther 2001 Dec; 8(6): 638–47.
Berridge DC, Gregson RH, Hopkinson BR, et al. Randomized trial of intra-arterial recombinant tissue plasminogen activator, intravenous recombinant tissue plasminogen activator and intra-arterial streptokinase in peripheral arterial thrombolysis. Br J Surg 1991 Aug; 78(8): 988–95.
Meyerovitz MF, Goldhaber SZ, Reagan K, et al. Recombinant tissue-type plasminogen activator versus urokinase in peripheral arterial and graft occlusions: a randomized trial. Radiology 1990 Apr; 175(1): 75–8.
Schweizer J, Altmann E, Stosslein F, et al. Comparison of tissue plasminogen activator and urokinase in the local infiltration thrombolysis of peripheral arterial occlusions. Eur J Radiol 1996 May; 22(2): 129–32.
Funaki B, Van Ha T. Catheter-directed thrombolysis in 2002: what have we learnt. New Dev Vasc Dis 2002; 3(2): 7–9.
Bravata DM. Intravenous thrombolysis in acute ischaemic stroke: optimising its use in routine clinical practice. CNS Drugs 2005; 19(4): 295–302.
Caplan LR. Treatment of acute stroke: still struggling. JAMA 2004 Oct 20; 292(15): 1883–5.
Lindsberg PJ, Soinne L, Tatlisumak T, et al. Long-term outcome after intravenous thrombolysis of basilar artery occlusion. JAMA 2004 Oct 20; 292(15): 1862–6.
Adams H, Adams R, Del Zoppo G, et al. Guidelines for the early management of patients with ischemic stroke: 2005 Guidelines Update. A scientific statement from the Stroke Council of the American Stroke Association/American Heart Association. Stroke 2005; 36: 916–23.
Wardlaw JM, Del Zoppo G, Yamaguchi T, et al. Thrombolysis for acute ischaemic stroke. The Cochrane Database of Systematic Reviews 2003; 3 Art. no.: CD00213. DOI: 10.1002/14651858.CD00213.
Sugg RM, Noser EA, Shaltoni HM, et al. Intra-arterial reteplase compared to urokinase for thrombolytic recanalization in acute ischemic stroke. Am J Neuroradiol 2006 Apr; 27(4): 769–73.
Patel SC, Mody A. Cerebral hemorrhagic complications of thrombolytic therapy. Prog Cardiovasc Dis 1999; 42(3): 217–33.
Baumann CR, Baumgartner RW, Gandjour J, et al. Good outcomes in ischemic stroke patients treated with intravenous thrombolysis despite regressing neurological symptoms. Stroke 2006 May; 37(5): 1332–3.
Author information
Authors and Affiliations
Corresponding author
Additional information
Various sections of the manuscript reviewed by: E. R. Bates, University of Michigan Medical Center, Ann Arbor, Michigan, USA; D. L. Bhatt, Department of Cardiovascular Medicine, Cleveland Clinic Foundation, Cleveland, Ohio, USA; E. Boersma, University Hospital Rotterdam, Rotterdam, The Netherlands; J. French, Department of Medicine, South Western Sydney Clinical School, University of New South Wales, Sydney, New South Wales, Australia; M. Ohman, Department of Medicine, Duke University Medical Center, Durham, North Carolina, USA; S. R. Steinhubl, Division of Cardiology, University of Kentucky, Lexington, Kentucky, USA.
Data Selection p ]Sources: Medical literature published in any language since 1980 on ‘reteplase’, identified using MEDLINE and EMBASE, supplemented by AdisBase (a proprietary database of Adis International). Additional references were identified from the reference lists of published articles. Bibliographical information, including contributory unpublished data, was also requested from the company developing the drug.
Search strategy: MEDLINE, EMBASE, and AdisBase search terms were ‘reteplase’. Searches were last updated 1 August 2006.
Selection: Studies in patients with thromboembolic disorders or central venous/hemodialysis catheter occlusion who received reteplase. Inclusion of studies was based mainly on the methods section of the trials. When available, large, well controlled trials with appropriate statistical methodology were preferred. Relevant pharmacodynamic and pharmacokinetic data are also included.
Index terms: Reteplase, plasminogen activators, acute myocardial infarction, peripheral arterial occlusion, acute ischemic stroke, central catheter occlusion, central hemodialysis catheter occlusion, pulmonary embolism, pharmacodynamics, pharmacokinetics, tolerability.
Rights and permissions
About this article
Cite this article
Simpson, D., Siddiqui, M.A.A., Scott, L.J. et al. Reteplase. Am J Cardiovasc Drugs 6, 265–285 (2006). https://doi.org/10.2165/00129784-200606040-00007
Published:
Issue Date:
DOI: https://doi.org/10.2165/00129784-200606040-00007