Abstract
Ever since tissue plasminogen activator (tPA) was approved for therapeutic fibrinolysis in 1987, it has been the fibrinolytic of choice. At the same time, it is also recognized that tPA never lived up to its clinical expectations and has more recently been replaced by percutaneous coronary intervention (PCI) as the treatment of choice for acute myocardial infarction (AMI). For other occlusive vascular diseases and for patients in remote areas, tPA remains an essential option. In view of the continued importance of fibrinolysis, it is disappointing that fibrinolysis never evolved beyond what it was when tPA replaced streptokinase (SK) 32 years ago. The endovascular procedure replacement for AMI treatment suffers from being technically demanding, time-consuming, and costly. An untested alternative fibrinolytic paradigm is that of the endogenous, physiological system, which is initiated by tPA but then is followed by the other natural plasminogen activator, urokinase plasminogen activator (uPA). In this combination, it is uPA rather than tPA that has the dominant function. This is also evident from gene knockout studies where deletion of uPA that it has the dominant effect. The fibrinolytic properties of tPA and uPA are complementary so that their combined effect is synergistic, especially when they are administered sequentially starting with tPA. Endogenous fibrinolysis functions without bleeding side effects and is ongoing. This is evidenced by the invariable presence in blood of the fibrin degradation product, D-dimer (normal concentration 110–250 ng/ml). This activator combination, consisting of a mini bolus of tPA followed by a 90-min proUK infusion, was once used to treat 101 AMI patients. Compared with the best of the tPA mega trials, this regimen resulted in an almost a doubling of the infarct artery patency rate and reduced mortality sixfold. To date, a second trial has not yet been done.


Similar content being viewed by others
References
Rijken DC, Hoylaerts M, Collen D. Fibrinolytic properties of one-chain and two-chain human extrinsic (tissue-type) plasminogen activator. J Biol Chem. 1982;257:2920–5.
GISSI-2: a factorial randomised trial of alteplase versus streptokinase and heparin versus no heparin among 12,490 patients with acute myocardial infarction. Gruppo Italiano Per Lo Studio Della Sopravvivenza Nell’Infarto Miocardico. Lancet. 1990;336:65–71.
ISIS-3: a randomized comparison of streptokinase vs tissue plasminogen activator vs anistreplase and of aspirin plus heparin vs aspirin alone among 41,299 cases of suspected acute myocardial infarction. ISIS-3 Third International Study of Infarct Survival Collaborative Group. Lancet. 1992;339:65–71.
The GUSTO Investigators. An international randomized trial comparing four thrombolytic strategies for acute myocardial infarction. N Eng J Med. 1993;329:673–82.
Brophy JM, Joseph L. Placing trials in context using Bayesian analysis. GUSTO revisited by Reverend Bayes. JAMA. 1995;273:871–5.
Pennica D, Holmes WE, Kohr WJ, Harkins RN, Vehar GA, Wad XCA, et al. Cloning and expression of human tissue-type plasminogen activator cDNA in E.coli. Nature. 1983;301:214–21.
Baglin TP, Landown R, Frasson R, Huntington JA. Discovery and characterization of an antibody directed against exosite 1 of thrombin. J Thromb Haemost. 2016;14:137–42.
Assessment of the Safety and Efficacy of a New Treatment Strategy with Percutaneous Coronary Intervention (ASSENT-4 PCI) investigators. Primary versus tenecteplase-facilitated percutaneous coronary intervention in patients with ST-segment elevation acute myocardial infarction (ASSENT-4 PCI): randomised trial. Lancet. 2006;367:569–78.
Pannell R, Black J, Gurewich V. The complementary modes of action of tissue plasminogen activator (t-PA) and pro-urokinase (proUK) by which their synergistic effect on clot lysis may be explained. J Clin Invest. 1988;81:853–9.
Husain SS, Lipinski B, Gurewich V. Rapid purification of high affinity plasminogen activator from human plasma by specific adsorption on fibrin-celite. Proc Nat Acad Sci (USA). 1981;78:4265–9.
Gurewich V, Pannell R, Louie S, Kelley P, Suddith RL, Greenlee R. Effective and fibrin-specific clot lysis by a zymogen precursor form of urokinase (pro-urokinase). A study in vitro and in two animal species. J Clin Invest. 1984;73:1731–9.
Liu J, Gurewich V. Fragment E-2 from fibrin substantially enhances pro-urokinase-induced glu-plasminogen activation. A kinetic study using a plasmin-resistant mutant pro-urokinase (Ala-158-rpro-UK). Biochemistry. 1992;31:6311–7.
Collen D. The plasminogen (fibrinolytic) system. Thromb Haemost. 1999;82:259–70.
Voskuilen M, Vermond A, Veeneman GH, van Boom JH, Klasen EA, Zegers ND, et al. Fibrinogen lysine residue Aα157 plays a crucial role in the fibrin-induced acceleration of plasminogen activation, catalyzed by tissue-type plasminogen activator. J Biol Chem. 1987;262(13):5944–6.
Hoylaerts M, Rijken DC, Lijnen HR, Collen D. Kinetics of the activation of plasminogen by human tissue plasminogen activator. Role of fibrin. J Biol Chem. 1982;257:2912–9.
Suenson E, Lützen O, Thorsen S. Initial plasmin-degradation of fibrin as the basis of a positive feed-back mechanism in fibrinolysis. Eur J Biochem. 1984;140:513–22.
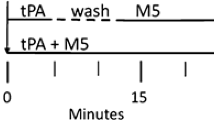
Pannell R, Li S, Gurewich V. Fibrin-specific and effective clot lysis requires both plasminogen activators and for them to be in a sequential rather than simultaneous combination. J Thromb Thrombolysis. 2017;44:210–5.
Pannell R, Li S, Gurewich V. Highly effective fibrinolysis by a sequential synergistic combination of mini-dose tPA plus low-dose mutant proUK. PLOS One. 2015;10:1–15.
Harpel PC, Chang TS, Verderber E. Tissue plasminogen activator and urokinase mediate the binding of Glu-plasminogen to plasma fibrin I. Evidence for new binding sites in plasmin-degraded fibrin I. J Biol Chem. 1985;260(7):4432–40.
Petersen LC. Kinetics of reciprocal pro-urokinase/plasminogen activation. Stimulation by a template formed by the urokinase receptor bound to poly (D-lysine). Eur J Biochem. 1997;245:316–23.
Bugge TH, Flick MJ, Danton MJS, Daugherty CC, Rømer J, Danø K, et al. Urokinase-type plasminogen activator is effective in fibrin clearance in the absence of its receptor or tissue-type plasminogen activator. Proc Natl Acad Sci USA. 1996;93:5899–904.
Singh I, Burnand KG, Collins M, Luttun A, Collen D, Boelhouwer B, et al. Failure of thrombus to resolve in urokinase-type plasminogen activator gene-knockout mice: rescue by normal bone marrow-derived cells. Circulation. 2003;107:869–75.
Gurewich V. Therapeutic fibrinolysis. How efficacy and safety can be improved. J Am Coll Cardiol. 2016;68:2099–106.
Zarich SW, Kowalchuk GJ, Weaver WD, Loscalzo J, Sassower M, Manzo K, et al. Sequential combination thrombolytic therapy for acute myocardial infarction: results of the pro-urokinase and t-PA enhancement of thrombolysis (PATENT) trial. J Am Coll Cardiol. 1995;26:374–9.
GUSTO Angiographic Investigators. The effects of tissue plasminogen activator, streptokinase, or both on coronary-artery patency, ventricular function, and survival after acute myocardial infarction. N Engl J Med. 1993;329:1615–22.
Collen D, Stassen JM, Stump DC, Verstraete M. Synergism of thrombolytic agents in vivo. Circulation. 1986;74:838–42.
Park S, Harker LA, Marzec UM, Levin EG. Demonstration of single chain urokinase-type plasminogen activator on human platelet membrane. Blood. 1989;6:1421–5.
Jiang YP, Pannell R, Liu JN. Gurewich V: evidence for a novel binding protein for urokinase-type plasminogen activator in platelet membranes. Blood. 1996;87:2775–81.
Baeten KM, Richard MC, Kanse SM, Mutch NJ, Degens JL, Booth NA. Activation of single-chain urokinase-type plasminogen activator by platelet-associated plasminogen: a mechanism for stimulation of fibrinolysis by platelets. J Thromb Haemost. 2010;8:1313–22.
Weaver WD, Hartmann JR, Anderson JL, Reddy PS, Sobolski JC, Sasahara A for the Prourokinase Study Group. New recombinant glycosylated prourokinase for treatment of patients with acute myocardial infarction. J Am Coll Cardiol. 1994;241:1242–8.
The IST-3 Collaborative Group. The benefits and harms of intravenous thrombolysis with recombinant tissue plasminogen activator within 6 h of acute ischaemic stroke (the third international stroke trial [IST-3]): a randomised controlled trial. Lancet. 2012;379:2352–63.
Montoney M, Gardell SJ, Marder VJ. Comparison of the bleeding potential of vampire bat salivary plasminogen activator versus tissue plasminogen activator in an experimental rabbit model. Circulation. 1995;91:1540–4.
Vermeer F, Bösl I, Meyer J, Bär F, Charbonnier B, Windeler J, et al. Saruplase is a safe and effective thrombolytic agent; observations in 1698 patients: results of the PASS Study. J Thromb Thrombolys. 1999;8:143–50.
Acknowledgements
The author wishes to thank Ralph Pannell, PhD, for his valuable editorial contributions
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Victor Gurewich MD is the scientific director of Thrombolytic Science International (TSI), a small company that is developing a prouPA mutant for fibrinolytic therapy. Ralph Pannell PhD has no disclosures or conflicts of interest to report.
Additional information
Key Findings
• Common pathologies like stroke and heart attack are usually caused by a thrombus.
• Optimal salvage of function and of life requires restoration of perfusion within 1–2 h, which is most readily accomplished by fibrinolysis.
• However, fibrinolysis with tPA has been inadequate and risky.
• Physiological fibrinolysis utilizes both tPA and uPA and is effective in the absence of bleeding side effects.
• Therefore, it provides a model to make fibrinolytic therapy safer.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Gurewich, V. Fibrinolysis: a Misunderstood Natural Defense Whose Therapeutic Potential Is Unknown. Cardiovasc Drugs Ther 33, 749–753 (2019). https://doi.org/10.1007/s10557-019-06923-8
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10557-019-06923-8