Abstract
Objective
To document prescribing patterns of lipid-modifying therapies in hypercholesterolemic patients, cholesterol goal attainment, and factors associated with cholesterol goal attainment in Norway.
Method
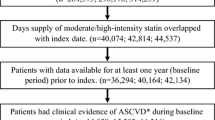
This was a retrospective, observational study using existing computerized patient records at 11 primary healthcare centers in Norway and the Norwegian Patient Register of hospital data. The study population was 3111 patients identified in the primary care database who were prescribed a lipid-modifying therapy between the dates of July 1987 and May 2003 and who were α18 years of age at the time of the first prescription. Of these patients, 1337 patients had uncontrolled lipid measures at baseline. In the analysis of goal attainment, data were available for 877 (28% of the total study population) and 1144 (37%) patients with baseline and follow-up total cholesterol (TC) and/or low-density lipoprotein-cholesterol (LDL-C) levels after 4 and 12 months’ treatment, respectively.
Outcome measures
Initial lipid-modifying therapy (drug and dosage), changes in initial lipid-modifying therapy, cholesterol goal attainment, and factors related to cholesterol goal attainment. Cholesterol treatment goals were defined as LDL-C <3.0 mmol/L and/or TC <5.0 mmol/L (as per the Second Joint Task Force of European Societies on the Prevention of Cardiovascular Disease).
Results
The initial lipid-modifying therapy was a HMG-CoA reductase inhibitor (statin) in 98% of patients, most often simvastatin (42%; mean initial dosage = 18.4 mg/day) or atorvastatin (34%; 12.7 mg/day). The median year of treatment initiation was 1999 and the mean duration of follow-up was 39 months. The initial prescription remained unchanged at year 1 for most patients (69%), whereas 17% discontinued drug treatment. Mean TC levels decreased from 7.36 mmol/L at baseline (n=1337) to 5.31 mmol/L at 12 months (n=1144; p < 0.05), whereas mean LDL-C levels decreased from 4.98 (n=847) to 3.08 mmol/L at 12 months (n=713; p < 0.05). These mean reductions occurred within 3 months of the initial prescription and did not change subsequently. A total of 32.9% of patients who were not at goal at baseline achieved cholesterol goal 12 months after initiating treatment. The factors related to cholesterol goal attainment at 12 months were: baseline TC level (odds ratio [OR] 0.64; 95% CI 0.58, 0.71), treatment with a statin (OR 8.60; 95% CI 1.13, 65.4), diagnosis of diabetes mellitus (OR 2.91; 95% CI 2.01, 4.21), and age (OR 1.02; 95% CI 1.01, 1.03).
Conclusions
Lipid-modifying therapy in Norway is dominated by statin monotherapy. In this analysis of primary-care patients, maximal reductions in cholesterol levels were seen within the first 3–4 months after therapy initiation. After 12 months of treatment, 67% of patients remained above recommended cholesterol levels. More effective and well tolerated treatment strategies are needed to improve the probability of patients achieving cholesterol treatment goals.







Similar content being viewed by others
Notes
The use of trade names is for product identification purposes only and does not imply endorsement.
References
Kannel WB, Castelli WP, Gordon T, et al. Serum cholesterol, lipoproteins, and the risk of coronary heart disease: the Framingham study. Ann Intern Med 1971 Jan; 74(1): 1–12.
Multiple Risk Factor Intervention Trial Research Group. Multiple Risk Factor Intervention Trial: risk factor changes and mortality results. JAMA 1982 Sep; 248(12): 1465–77.
Anderson KM, Castelli WP, Levy D. Cholesterol and mortality: 30 years of follow-up from the Framingham study. JAMA 1987 Apr; 257(16): 2176–80.
The Lipid Research Clinics Coronary Primary Prevention Trial results. II. The relationship of reduction in incidence of coronary heart disease to cholesterol lowering. JAMA 1984 Jan; 251(3): 365–74.
Frick MH, Elo O, Haapa K, et al. Helsinki Heart Study: primary-prevention trial with gemfibrozil in middle-aged men with dyslipidemia: safety of treatment, changes in risk factors, and incidence of coronary heart disease. N Engl J Med 1987 Nov; 317(20): 1237–45.
Randomised trial of cholesterol lowering in 4444 patients with coronary heart disease: the Scandinavian Simvastatin Survival Study (4S). Lancet 1994 Nov; 344 (8934): 1383–1389.
Shepherd J, Cobbe SM, Ford I, et al. Prevention of coronary heart disease with pravastatin in men with hypercholesterolemia: West of Scotland Coronary Prevention Study Group. N Engl J Med 1995 Nov; 333(20): 1301–7.
Sacks FM, Pfeffer MA, Moye LA, et al. The effect of pravastatin on coronary events after myocardial infarction in patients with average cholesterol levels: Cholesterol and Recurrent Events Trial investigators. N Engl J Med 1996 Oct; 335(14): 1001–9.
Downs JR, Clearfield M, Weis S, et al. Primary prevention of acute coronary events with lovastatin in men and women with average cholesterol levels: results of AFCAPS/TexCAPS. Air Force/Texas Coronary Atherosclerosis Prevention Study. JAMA 1998 May; 279(20): 1615–22.
Heart Protection Study Collaborative Group. MRC/BHF Heart Protection Study of cholesterol lowering with simvastatin in 20,536 high-risk individuals: a randomised placebo-controlled trial. Lancet 2002 Jul; 360(9326): 7–22.
Sever PS, Dahlof B, Poulter NR, et al. Prevention of coronary and stroke events with atorvastatin in hypertensive patients who have average or lower-than-average cholesterol concentrations, in the Anglo-Scandinavian Cardiac Outcomes Trial: Lipid Lowering Arm (ASCOT-LLA): a multicentre randomised controlled trial. Lancet 2003; 361: 1149–58.
Collins R, Armitage J, Parish S, et al. Effects of cholesterol-lowering with simvastatin on stroke and other major vascular events in 20536 people with cerebrovascular disease or other high-risk conditions. Lancet 2004; 363:757–67.
Cannon CP, Braunwald E, McCabe CH, et al. Intensive versus moderate lipid lowering with statins after acute coronary syndromes. N Engl J Med 2004; 350: 1495–504.
Collins R, Armitage J, Parish S, et al. MRC/BHF Heart Protection Study of cholesterol-lowering with simvastatin in 5963 people with diabetes: a randomised placebo-controlled trial. Lancet 2003 Jun; 361(9374): 2005–16.
Nissen SE, Tuzcu EM, Schoenhagen P, et al. Effect of intensive compared with moderate lipid-lowering therapy on progression of coronary atherosclerosis: a randomized controlled trial. JAMA 2004 Mar; 291(9): 1071–80.
De Backer G, Ambrosioni E, Borch-Johnsen K, et al. European guidelines on cardiovascular disease prevention in clinical practice: Third Joint Task Force of European and Other Societies on Cardiovascular Disease Prevention in Clinical Practice. Eur Heart J 2003 Sep; 24(17): 1601–10.
Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults. Executive summary of the third report of the national cholesterol education program (NCEP) expert panel on detection, evaluation, and treatment of high blood cholesterol in adults (adult treatment panel III). JAMA 2001 May; 285(19): 2486–97.
Pearson TA, Laurora I, Chu H, et al. The lipid treatment assessment project (LTAP): a multicenter survey to evaluate the percentages of dyslipidemic patients receiving lipid-lowering therapy and achieving low-density lipoprotein cholesterol goals. Arch Intern Med 2000 Feb; 160(4): 459–67.
Latts LM. Assessing the results: phase 1 hyperlipidemia outcomes in 27 health plans. Am J Med 2001 Apr; 110 Suppl. 6A: 17–23S.
McBride P, Schrott HG, Plane MB, et al. Primary care practice adherence to National Cholesterol Education Program guidelines for patients with coronary heart disease. Arch Intern Med 1998 Jun; 158(11): 1238–44.
Olson KL, Bungard TJ, Tsuyuki RT. Cholesterol risk management: a systematic examination of the gap from evidence to practice. Pharmacotherapy 2001 Jul; 21(7): 807–17.
Olson KL, Tsuyuki RT. Patients’ achievement of cholesterol targets: a cross-sectional evaluation. Am J Prev Med 2003 Nov; 25(4): 339–42.
EUROASPIRE. A European Society of Cardiology survey of secondary prevention of coronary heart disease: principal results: EUROASPIRE Study Group: European Action on Secondary Prevention through Intervention to Reduce Events. Eur Heart J 1997 Oct; 18(10): 1569–82.
EUROASPIRE II Study Group. Lifestyle and risk factor management and use of drug therapies in coronary patients from 15 countries: principal results from EUROASPIRE II Euro Heart Survey Programme. Eur Heart J 2001 Apr; 22(7): 554–72.
EUROASPIRE I and II Group: European Action on Secondary Prevention by Intervention to Reduce Events. Clinical reality of coronary prevention guidelines: a comparison of EUROASPIRE I and II in nine countries: EUROASPIRE I and II Group: European Action on Secondary Prevention by Intervention to Reduce Events. Lancet 2001 Mar; 357(9261): 995–1001.
Svilaas A, Ose L, Risberg K, et al. Treatment goals for blood lipids in high risk patients of atherosclerotic disease [in Norwegian]. Tidsskr Nor Laegeforen 2001 Mar; 121(9): 1059–63.
Svilaas A, Risberg K, Thoresen M, et al. Lipid treatment goals achieved in patients treated with statin drugs in Norwegian general practice. Am J Cardiol 2000 Dec; 86(11): 1250–3, A6.
Tonstad S, Rosvold EO, Furu K, et al. Undertreatment and overtreatment with statins: the Oslo Health Study 2000–2001. J Intern Med 2004; 255: 494–502.
Lindgren P, Borgström F, Stålhammar J, et al. Association between achieving treatment goals for lipid-lowering and cardiovascular events in real clinical practice. Eur J Cardiovasc Prev Rehabil 2005 Dec; 12(6): 530–4.
Van Ganse E, Souchet T, Laforest L. Long-term achievement of the therapeutic objectives of lipid-lowering agents in primary prevention patients and cardiovascular outcomes: an observational study. Atherosclerosis 2006 Mar; 185(1): 58–64. Epub 2005 Jul 20.
Van Ganse E, Souchet T, Laforest L, et al. Effectiveness of lipid-lowering therapy in French primary care. Br J Clin Pharmacol 2005 Apr; 59(4): 456–63.
Krobot KJ, Yin DD, Alemao E, et al. Real-world effectiveness of lipid-lowering therapy in male and female outpatients with CHD: relation to pretreatment LDL cholesterol, pretreatment CHD risk, and other factors. Eur J Cardiovasc Prev Rehabil 2005 Feb; 12(1): 37–45.
The Reality Study Group. Current lipid management and low cholesterol goal attainment in common daily practice in Spain: the Reality Study. Pharmacoeconomics 2004; 22 Suppl. 3: 1–12.
Pyorala K, De Backer G, Graham I, et al. Prevention of coronary heart disease in clinical practice: recommendations of the Task Force of the European Society of Cardiology, European Atherosclerosis Society and European Society of Hypertension. Atherosclerosis 1994 Oct; 110(2): 121–61.
Compliance and adverse event withdrawal: their impact on the West of Scotland Coronary Prevention Study. Eur Heart J 1997; 18: 1718–1724.
Larsen J, Andersen M, Kragstrup J, et al. High persistence of statin use in a Danish population: compliance study 1993–1998. Br J Clin Pharmacol 2002; 53: 375–8.
Durack-Brown I, Giral P, D’Ivernois J-F, et al. Patients’ and physicians’ perceptions and experience of hypercholesterolemia: a qualitative study. Br J Gen Pract 2003; 53: 851–7.
Hobbs FD, Erhardt L. Acceptance of guideline recommendations and perceived implementation of coronary heart disease prevention among primary care physicians in five European countries: the Reassessing European Attitudes about Cardiovascular Treatment (REACT) survey. Fam Pract 2002; 19: 596–604.
Cabana MD, Rand CS, Powe NR, et al. Why don’t physicians follow clinical practice guidelines? A framework for improvement. JAMA 1999; 282:1458–65.
Benner JS, Tierce JC, Ballantyne CM, et al. Follow-up lipid tests and physician visits are associated with improved adherence to statin therapy. Pharmacoeconomics 2004; 22 Suppl. 3: 13–23.
Acknowledgments
The study was funded by a grant form Merck/Schering Plough Limited Liability Company (Singapore). Merck/Schering Plough Limited Liability Company has developed, manufactured, and marketed lipid-modifying therapies.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Ose, L., Skjeldestad, F.E., Bakken, I.J. et al. Lipid Management and Cholesterol Goal Attainment in Norway. Am J Cardiovasc Drugs 6, 121–128 (2006). https://doi.org/10.2165/00129784-200606020-00006
Published:
Issue Date:
DOI: https://doi.org/10.2165/00129784-200606020-00006