Abstract
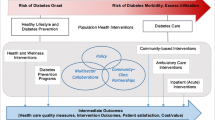
In this article, we provide a practical and systematic framework to evaluate the cost effectiveness of health plans’ investments towards improvements in diabetes care. Through a literature search of PubMed and our own review, we identified research studies providing evidence on the cost effectiveness of diabetes management. Published and unpublished studies that address these issues are reviewed and synthesized in this paper, with the goal of assisting resource allocation decision makers in selecting the most appropriate and effective diabetes care improvement strategies available to meet the needs of specific care delivery systems and patient populations. We summarize this evidence as it relates to four areas: (i) healthcare provider characteristics, the provider-patient relationship, and systems of care; (ii) clinical care decisions including the management of blood glucose, blood pressure, and cholesterol; (iii) models for improved delivery of care; and (iv) the health plan perspective regarding returns on investment.
Research data indicate that cost effectiveness varies by clinical domain. Blood pressure control, use of aspirin, and influenza and pneumococcal immunizations are cost saving in adults with diabetes across a wide range of ages and types of patients. Lipid control is most cost effective between the ages of 45–85 years, while the cost effectiveness of intensified glycemic control declines with age. Cost-effective diabetes management may be organized by primary care clinicians or by case managers working closely with either primary care or subspecialty physicians. Each delivery model has unique advantages and limitations, and there are insufficient data to compare the cost effectiveness of diabetes care across these organizational settings. Improving or enhancing a current model may require substantial investment. However, the resulting changes in the delivery of care may extend the benefits of improved management to other chronic diseases and to preventive care.
There is evidence that patient activation, physician behavior change, and care system improvements may improve care, but the cost effectiveness of these strategies is incompletely understood at present. Selection of clinical goals for improvement is likely to have a major impact on cost effectiveness, with maximal return on investment for blood pressure control, aspirin use, immunizations, and smoking cessation. Effective diabetes care can be delivered across a wide range of care settings, including primary care clinics. The organizational characteristics of clinics and use of tools such as patient registries, guidelines, visit planning and active outreach to patients improve care, but returns on investment with regards to these specific strategies awaits further research.

Similar content being viewed by others
References
Hogan P, Dall T, Nikolov P. Economic costs of diabetes in the US in 2002. Diabetes Care 2003 Mar; 26(3): 917–32.
Diabetes Control and Complications Trial Research Group. Resource utilization and costs of care in the diabetes control and complications trial: The Diabetes Control and Complications Trial Research Group. Diabetes Care 1995; 18(11): 1468–78.
UK Prospective Diabetes Study Group. 3. Cost effectiveness analysis of improved blood pressure control in hypertensive patients with type 2 diabetes: UKPDS 40. UK Prospective Diabetes Study Group. BMJ 1998 Sep 12; 317(7160): 720–6.
Eastman RC, Javitt JC, Herman WH, et al. Model of complications of NIDDM I: model construction and assumptions. Diabetes Care 1997; 20: 725–34.
Eastman RC, Javitt JC, Herman WH, et al. Model of complications of NIDDM II: analysis of the health benefits and cost-effectiveness of treating NIDDM with the goal of normoglycemia. Diabetes Care 1997; 20(5): 735–44.
CDC Diabetes Cost-effectiveness Group. Cost-effectiveness of intensive glycemic control, intensified hypertension control, and serum cholesterol level reduction for type 2 diabetes: The CDC Diabetes Cost-effectiveness Group. JAMA 2002 May 15; 287(19): 2542–51.
Selby JV, Ray GT, Zhang D, et al. Excess costs of medical care for patients with diabetes in a managed care population. Diabetes Care 1997; 20(9): 1396–402.
Greenfield S, Nerlson EC, Zubkoff M, et al. Variations in resource utilization among medical specialties and systems of care: results from the Medical Outcomes Study. JAMA 1992; 267(12): 1624–30.
Greenfield S, Rogers W, Mangotich M, et al. Outcomes of patients with hypertension and non-insulin-dependent diabetes mellitus treated by different systems and specialists: results from the Medical Outcomes Study. JAMA 1995; 274: 1436–44.
Woolhandler S, Himmelstein DU. Costs of care and administration at for-profit and other hospitals in the United States. N Engl J Med 1997 Mar 13; 336(11): 769–74.
Griffin S. Diabetes care in general practice: meta-analysis of randomised control trials. BMJ 1998; 317(7155): 390–6.
Griffin S, Kinmonth A. Diabetes care: the effectiveness of systems for routine surveillance for people with diabetes. Cambridge: University of Cambridge: Institute of Public Health, 1999.
Hofer TP, Hayward RA, Greenfield S, et al. The unreliability of individual physician ‘report cards’ for assessing the costs and quality of care of a chronic disease. JAMA 1999; 281(22): 2098–105.
Bodenheimer T, Wagner EH, Grumbach K. Improving primary care for patients with chronic illness. JAMA 2002; Oct 9; 288(14): 1775–9.
Johnson PE, Veazie PJ, Kochevar L, et al. Understanding variation in chronic disease outcomes. Health Care Manag Sci 2002; 5: 175–89.
Gaede P, Vedel P, Larsen N, et al. Multifactorial intervention and cardiovascular disease in patients with type 2 diabetes. N Engl J Med 2003 Jan 30; 348(5): 383–93.
Hall JA, Palmer RH, Orav EJ, et al. Performance quality, gender, and professional role: a study of physicians and nonphysicians in 16 ambulatory care practices. Med Care 1990 Jun; 28(6): 489–501.
UK Prospective Diabetes Study (UKPDS) Group. 19. Intensive blood-glucose control with sulphonylureas or insulin compared with conventional treatment and risk of complications in patients with type 2 diabetes (UKPDS 33). UK Prospective Diabetes Study (UKPDS) Group. Lancet 1998 Sep 12; 352(9131): 837–53.
UK Prospective Diabetes Study (UKPDS) Group. 20. Effect of intensive bloodglucose control with metformin on complications in overweight patients with type 2 diabetes (UKPDS 34). UK Prospective Diabetes Study (UKPDS) Group. Lancet 1998 Sep 12; 352(9131): 854–65.
Curb JD, Pressel SL, Cutler JA, et al. Effect of diuretic based antihypertensive treatment on cardiovascular disease risk in older diabetic patients with isolated systolic hypertension: Systolic Hypertension in Elderly Program Cooperative Research Group. JAMA 1996; 276(23): 1886–92.
Hansson L, Zanchetti A, Carruthers SG, et al. Effects of intensive blood-pressure lowering and low-dose aspirin in patients with hypertension: principal results of the Hypertension Optimal Treatment (HOT) randomised trial. HOT Study Group. Lancet 1998 Jun 13; 351(9118): 1755–62.
Pyorala K, Pedersen TR, Kjekshus J, et al. Cholesterol lowering with simvastatin improves prognosis of diabetic patients with coronary heart disease: a subgroup analysis of the Scandinavian Simvastatin Survival Study (4S). Diabetes Care 1997 Apr; 20(4): 614–20.
Haffner SM. The Scandinavian Simvastatin Survival Study (4S) subgroup analysis of diabetic subjects: implications for the prevention of coronary heart disease. Diabetes Care 1997; 20(4): 469–71.
Phillips LS, Branch WT, Cook CB, et al. Clinical inertia. Ann Intern Med 2001 Nov 6; 135(9): 825–34.
Soumerai S, McLaughlin T, Gurwitz J, et al. Effect of local medical opinion leaders on quality of care for acute myocardial infarction: a randomized controlled trial. JAMA 1998; 279(17): 1358–63.
Soumerai S, Avorn J. Principles of education outreach (academic detailing) to improve clinical decision-making. JAMA 1990; 263(4): 549–63.
O’Connor P. Organizing diabetes care: identify, monitor, prioritize, intensify. Diabetes Care 2001; 24(9): 1515–6.
O’Connor P. Improving diabetes care: organize your office, intensify your care. J Am Board Fam Pract 2001; 14(4): 320–2.
Levetan CS, Passaro MD, Jablonski KA, et al. Effect of physician specialty on outcomes in diabetic ketoacidosis. Diabetes Care 1999 Nov; 22(11): 1790–5.
Greenfield S, Kaplan SH, Kahn R, et al. Profiling care provided by different groups of physicians: effects of patient case-mix (bias) and physician-level clustering on quality assessment results. Ann Intern Med 2002 Jan 15; 136(2): 111–21.
Grumbach K, Selby J, Schmittdiel J, et al. Quality of primary care practice in a large HMO according to physician specialty. Health Serv Res 1999; 34(2): 485–502.
Selby J, Grumbach K, Quesenberry CJ, et al. Differences in resource use and costs of primary care in a large HMO according to physician specialty. Health Serv Res 1999; 34(2): 503–18.
O’Connor PJ. Commentary: practice environment, specialty, and primary care. Health Serv Res 1999 Jun; 34(2): 519–24.
Glasgow RE, Hiss RG, Anderson RM, et al. Report of the health care delivery work group: behavioral research related to the establishment of a chronic disease model for diabetes care. Diabetes Care 2001; 24(1): 124–30.
Roter DL, Hall JA, Merisca R, et al. Effectiveness of interventions to improve patient compliance: a meta-analysis. Med Care 1998; 36(8): 1138–61.
Friedrich MJ. Enhancing diabetes care in a low-income, high-risk population. JAMA 2000 Jan 26; 283(4): 467–8.
Williams GC, Freedman ZR, Deci EL. Supporting autonomy to motivate patients with diabetes for glucose control. Diabetes Care 1998 Oct; 21(10): 1644–51.
Anderson RM, Funneil MM, Barr PA, et al. Learning to empower patients: results of professional education program for diabetes educators. Diabetes Care 1991 Jul; 14(7): 584–90.
Greenfield S, Kaplan SH, Ware JE, et al. Patients’ participation in medical care: effects on blood sugar control and quality of life in diabetes. J Gen Intern Med 1988; 3(5): 448–57.
Lorig KR, Sobel DS, Stewart AL, et al. Evidence suggesting that a chronic disease self-management program can improve health status while reducing hospitalization: a randomized trial. Med Care 1999; 37(1): 5–14.
Grol R, Mokkink H, Smits A. Work satisfaction of general practitioners and the quality of patient care. Fam Pract 1985; 2: 128–35.
Van de Ven A, Ferry D. Measuring and assessing organizations. New York: John Wiley & Sons, 1980.
Starfield B, Powe NR, Weiner JR, et al. Costs vs quality in different types of primary care settings. JAMA 1994 Dec 28; 272(24): 1903–8.
O’Connor PJ, Sperl-Hillen JM, Pronk NP, et al. Primary care clinic-based chronic disease care. Dis Manage Health Outcomes 2001; 9(12): 691–8.
Sperl-Hillen J, O’Connor PJ, Carlson RR, et al. Improving diabetes care in a large health care system: an enhanced primary care approach. Jt Comm J Qual Improv 2000 Nov; 26(11): 615–22.
Berwick DM. A primer on leading the improvement of systems. BMJ 1996; 312: 619–22.
Mosser G. Clinical process improvement: engage first, measure later. Qual Manag Health Care 1996; 4(4): 11–20.
Nyman MA, Murphy ME, Schryver PG, et al. Improving performance in diabetes care: a multicomponent intervention. Eff Clin Pract 2000; 3(5): 205–12.
Brown JB, Pedula KL, Bakst AW. The progressive cost of complications in type 2 diabetes mellitus. Arch Intern Med 1999 Sep 13; 159(16): 1873–80.
Gilmer TP, O’Connor PJ, Manning WG, et al. The cost to health plans of poor glycemic control. Diabetes Care 1997; 20(12): 1847–53.
Centers for Disease Control. Economic aspects of diabetes services and education: selected annotations. Atlanta (GA): Centers for Disease Control, 1992.
Mokdad AH, Bowman BA, Ford ES, et al. The continuing epidemics of obesity and diabetes in the United States. JAMA 2001 Sep 12; 286(10): 1195–200.
Harris MI, Flegal KM, Cowie CC, et al. Prevalence of diabetes, impaired fasting glucose, and impaired glucose tolerance in US adults. The Third National Health and Nutrition Examination Survey, 1988–1994. Diabetes Care 1998 Apr; 21(4): 518–24.
National Diabetes Data Group. Diabetes in America. National Diabetes Data Group. Washington, DC: National Institutes of Health, 1995: Publ. No. 95–1468.
Wagner EH, Sandhu N, Newton KM, et al. Effect of improved glycemic control on health care costs and utilization. JAMA 2001; 285(2): 182–9.
National Cholesterol Education Program. Report of the expert panel on population strategies for blood cholesterol reduction. Circulation 1991; 83: 2154–232.
National Cholesterol Education Program. Executive Summary of the third report of the National Cholesterol Education Program (NCEP) expert panel on detection, evaluation, and treatment of high blood cholesterol in adults (Adult Treatment Panel III). JAMA 2001 May 16; 285(19): 2486–97.
Haffner SM, Alexander CM, Cook TJ, et al. Reduced coronary events in simvastatin-treated patients with coronary heart disease and diabetes or impaired fasting glucose levels: subgroup analyses in the Scandinavian Simvastatin Survival Study. Arch Intern Med 1999; 159(22): 2661–7.
Group HPSC. MRC/BHF Heart Protection Study of cholesterol lowering with simvastatin in 20,536 high-risk individuals: a randomised placebo-controlled trial. Lancet 2002 Jul 6; 360(9326): 7–22.
Herman WH, Alexander CM, Cook JR, et al. Effect of simvastatin treatment on cardiovascular resource utilization in impaired fasting glucose and diabetes: findings from the Scandinavian Simvastatin Survival Study. Diabetes Care 1999; 22(11): 1771–8.
Kannel WB. Elevated systolic blood pressure as a cardiovascular risk factor. Am J Cardiol 2000 Jan 15; 85(2): 251–5.
UK Prospective Diabetes Study (UKPDS) Group. 62. Efficacy of atenolol and captopril in reducing risk of macrovascular and microvascular complications in type 2 diabetes: UKPDS 39. UK Prospective Diabetes Study Group. BMJ 1998 Sep 12; 317(7160): 713–20.
Schrier R, Estacio R, Jeffers B. Appropriate blood pressure control in NIDDM (ABCD Trial). Diabetologia 1996; 39(12): 646–54.
Group ACR. Major outcomes in high-risk hypertensive patients randomized to angiotensin-converting enzyme inhibitor or calcium channel blocker vs diuretic: the Antihypertensive and Lipid-Lowering Treatment to Prevent Heart Attack Trial (ALLHAT). JAMA 2002 Dec 18; 288(23): 2981–97.
MacMahon S, Peto R, Cutler J, et al. Blood pressure, stroke, and coronary heart disease: Part 1, Prolonged differences in blood pressure: prospective observational studies corrected for the regression dilution bias. Lancet 1990 Mar 31; 335(8692): 765–74.
Barrett-Connor E, Wingard DL. “Normal” blood glucose and coronary risk. BMJ 2001 Jan 6; 322(7277): 5–6.
Wannamethee SG, Shaper AG, Whincup PH, et al. Smoking cessation and the risk of stroke in middle-aged men. JAMA 1995 Jul 12; 274(2): 155–60.
Gordon T, Kannel WB, McGee D, et al. Death and coronary attacks in men after giving up cigarette smoking: a report from the Framingham study. Lancet 1974 Dec 7; 2(7893): 1345–8.
Cromwell J, Bartosch WJ, Fiore MC, et al. Cost-effectiveness of the clinical practice recommendations in the AHCPR guideline for smoking cessation: Agency for Health Care Policy and Research. JAMA 1997 Dec 3; 278(21): 1759–66.
Zhu S-H, Anderson C, Tedeschi G, et al. Evidence of real-world effectiveness of a telephone quitline for smokers. N Engl J Med 2002 Oct; 347(14): 1087–93.
Nielsen K, Fiore MC. Cost-benefit analysis of sustained-release bupropion, nicotine patch, or both for smoking cessation. Prev Med 2000 Mar; 30(3): 209–16.
ETDRS Investigators. Aspirin effects on mortality and morbidity in patients with diabetes mellitus: Early Treatment Diabetic Retinopathy Study report 14. ETDRS Investigators. JAMA 1992 Sep 9; 268(10): 1292–300.
Antiplatelet Trialists’ Collaboration. Collaborative overview of randomised trials of antiplatelet therapy: I. prevention of death, myocardial infarction, and stroke by prolonged antiplatelet therapy in various categories of patients. Antiplatelet Trialists’ Collaboration. BMJ 1994 Jan 8; 308(6921): 81–106.
Rolka DB, Fagot-Campagna A, Narayan KM. Aspirin use among adults with diabetes: estimates from the Third National Health and Nutrition Examination Survey. Diabetes Care 2001 Feb; 24(2): 197–201.
O’Connor P, Pronk N, Tan A, et al. Does professional advice influence aspirin use to prevent heart disease in an HMO population? Eff Clin Pract 1998; 1(1): 26–32.
Maciosek M, Goodman M, O’Connor PJ. Selecting diabetes improvement strategies: costs and population health impact. Diabetes 2000; 49 Suppl. 1: A345.
Nichols GA, Glauber HS, Brown JB. Type 2 diabetes: incremental medical care costs during the 8 years preceding diagnosis. Diabetes Care 2000; 23(11): 1654–9.
Nichol KL, Nordin J, Mullooly J, et al. Influenza vaccination and reduction in hospitalizations for cardiac disease and stroke among the elderly. N Engl J Med 2003; 348: 1322–32.
Yusuf S, Sleight P, Pogue J, et al. Effects of an angiotensin-converting-enzyme inhibitor, ramipril, on cardiovascular events in high-risk patients: The Heart Outcomes Prevention Evaluation Study Investigators. N Engl J Med 2000; 342(3): 145–53.
Carroll CA, Coen MM, Rymer MM. Assessment of the effect of ramipril therapy on direct healthcare costs for first and recurrent strokes in high risk cardiovascular patients using data from the Heart Outcomes Prevention Evaluation (HOPE). Clin Ther 2003; 25: 1248–61.
Tuomilehto J, Lindstrom J, Eriksson JG, et al. Prevention of type 2 diabetes mellitus by changes in lifestyle among subjects with impaired glucose tolerance. N Engl J Med 2001 May 3; 344(18): 1343–50.
Diabetes Prevention Program Research Group. Reduction in the incidence of type 2 diabetes with lifestyle intervention or metformin. N Engl J Med 2002; 346: 393–403.
Duncan GE, Perri MG, Theriaque DW, et al. Exercise training, without weight loss, increases insulin sensitivity and postheparin plasma lipase activity in previously sedentary adults. Diabetes Care 2003 Mar; 26(3): 557–62.
Pronk N, Tan A, O’Connor P, et al. Identifying the potential to increase physical activity using stages of change in HMO members [abstract]. Med Sci Sports Exerc 1998; 30(5): S309.
O’Connor PJ, Rush WA, Prochaska JO, et al. Professional advice and readiness to change behavioral risk factors among members of a managed care organization. Am J Manag Care 2001 Feb; 7(2): 125–30.
Pritchard DA, Hyndman J, Taba F. Nutritional counselling in general practice: a cost effective analysis. J Epidemiol Community Health 1999 May; 53(5): 311–6.
Pronk N, Goodman M, O’Connor P, et al. Relationship between modifiable health risks and short-term health care charges. JAMA 1999; 282(23): 2235–9.
Martinson B, Crain A, Pronk N, et al. Changes in physical activity and short-term changes in health care charges: a prospective cohort study of older adults. Prev Med. In press.
Martinson BC, O’Connor PJ, Pronk NP. Physical inactivity and short-term all-cause mortality in adults with chronic disease. Arch Intern Med 2001; 161(9): 1173–80.
Haffner SM, Letho S, Ronnemaa T, et al. Mortality from chronic heart disease in subjects with type 2 diabetes and non-diabetic subjects with and without prior myocardial infarction. N Engl J Med 1998; 339: 229–34.
O’Connor PJ, Desai J, Rush WA, et al. Is having a regular provider of diabetes care related to intensity of care and glycemic control? J Fam Pract 1998 Oct; 47(4): 290–7.
Williams TF, Martin DA, Watkins JD, et al. The clinical picture of diabetic control, studied in four settings. Am J Public Health 1967; 57: 41–51.
Peterson K. Diabetes care by primary care physicians in Minnesota and Wisconsin. J Fam Pract 1994; 38(12): 361–7.
Hiss R, Anderson RM, Hess GE, et al. Community diabetes care: a 10-year perspective. Diabetes Care 1994; 17(10): 1124–34.
Sidorov J, Gabbay R, Harris R, et al. Disease management for diabetes mellitus: impact on Hemoglobin A1c. Am J Manag Care 2000; 6(11): 1217–26.
Sutherland JE, Hoehns JD, O’Donnell B, Wiblin RT. Diabetes management quality improvement in a family practice residency program. J Am Board Fam Pract 2001 Jul–Aug; 14(4): 243–51.
Wagner EH, Austin BT, Korff MV. Organizing care for patients with chronic illness. Milbank Q 1996; 74(4): 511–44.
Casalino L, Gillies RR, Shortell SM, et al. External incentives, information technology, and organized processes to improve health care quality for patients with chronic diseases. JAMA 2003 Jan 22–29; 289(4): 434–41.
O’Connor PJ. Electronic medical records and diabetes care improvement: are we waiting for Godot? Diabetes Care 2003 Mar; 26(3): 942–3.
Meigs JB, Cagliero E, Dubey A, et al. A controlled trial of web-based diabetes disease management: the MGH diabetes primary care improvement project. Diabetes Care 2003 Mar; 26(3): 750–7.
Norris SL, Nichols PJ, Caspersen CJ, et al. Increasing diabetes self-management education in community settings: a systematic review. Am J Prev Med 2002 May; 22(4 Suppl. 1): 39–66.
Aubert RE, Herman WH, Waters J, et al. Nurse case management to improve glycemic control in diabetic patients in a health maintenance organization: a randomized, controlled trial. Ann Intern Med 1998; 129(8): 605–12.
Sadur CN, Moline N, Costa M, et al. Diabetes management in a health maintenance organization: efficacy of care management using cluster visits. Diabetes Care 1999 Dec; 22(12): 2011–7.
Peters AL, Davidson MB, Ossorio RC. Management of patients with diabetes by nurses with support of subspecialists. HMO Pract 1995; 9(1): 8–13.
Weinberger M, Murray MD, Marrero DG, et al. Effectiveness of pharmacist care for patients with reactive airways disease: a randomized controlled trial. JAMA 2002 Oct 2; 288(13): 1594–602.
Norris SL, Nichols PJ, Caspersen CJ, et al. The effectiveness of disease and case management for people with diabetes: a systematic review. Am J Prev Med 2002 May; 22(4 Suppl.): 15–38.
Norris SL, Engelgau MM, Narayan KM. Effectiveness of self-management training in type 2 diabetes: a systematic review of randomized controlled trials. Diabetes Care 2001 Mar; 24(3): 561–87.
Philis-Tsimikas A, Walker C. Improved care for diabetes in underserved populations. J Ambul Care Manage 2001 Jan; 24(1): 39–43.
Philis-Tsimikas A, Rivard L, Walker C, et al. Nurse management of diabetes mellitus in low income latino populations (Project Dulce) improves care, clinical outcomes and culture bound beliefs [abstract]. Circulation 2002; 102(18): 856.
Weinberger M, Kirkman MS, Samsa GP, et al. A nurse-coordinated intervention for primary care patients with non-insulin-dependent diabetes mellitus: impact on glycemic control and health-related quality of life. J Gen Intern Med 1995; 10(2): 59–66.
Rubin RJ, Dietrich KA, Hawk AD. Clinical and economic impact of implementing a comprehensive diabetes management program in managed care. J Clin Endocrinol Metab 1998 Aug; 83(8): 2635–42.
Ramsey S, Summers KH, Leong SA, et al. 109. Productivity and medical costs of diabetes in a large employer population. Diabetes Care 2002 Jan 25; 25(1): 23–9.
Glasgow RE, Orleans CT, Wagner EH, et al. Does the chronic care model serve also as a template for improving prevention? Milbank Q 2001; 79(4): 579–612.
Gilmer T, Kronick R, Fishman P, et al. The Medicaid Rx model: pharmacy-based risk adjustment for public programs. Med Care 2001 Nov; 39(11): 1188–202.
Acknowledgements
This work was supported in part by grant RO1-HS 09946 from the Agency for Healthcare Quality and Research. The authors have no conflicts of interest that are directly relevant to the contents of this manuscript.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Gilmer, T., O’Connor, P.J. Cost Effectiveness of Diabetes Mellitus Management Programs. Dis-Manage-Health-Outcomes 11, 439–453 (2003). https://doi.org/10.2165/00115677-200311070-00004
Published:
Issue Date:
DOI: https://doi.org/10.2165/00115677-200311070-00004