Abstract
Current treatment modalities available for hepatitis B virus (HB V) or hepatitis C virus (HCV) infections are not efficient. The enormous disease burden caused by these two infections makes the development of novel therapies critical. For HCV, the development of an effective vaccine is urgent in view of the escalating number of infected individuals. Molecular therapies for HBV and HCV infection can be directed at reducing viral load by interfering with the life cycle of the viruses or at generating immune response against viral epitopes. The antiviral approaches consist of the delivery or expression of antisense RNAs, ribozymes or dominant negative proteins. Viral biology can be interrupted by attacking various potential targets within the two viruses. DNA-based vaccination strategies are being explored for both prevention and treatment of these diseases. Both non-viral and recombinant viral vectors are being developed for safe, effective and long-term gene transfer to the liver. Although no ‘ideal’ vector is available at this time, the ingenuity of numerous investigators is leading to the improvement of the vector systems, promising successful application of gene therapy to the prevention and treatment of viral hepatitis in the foreseeable future.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Viral hepatitis is a major worldwide health problem. It is estimated that approximately two billion people are infected globally with the hepatitis B virus (HBV). HBV infection produces a disease spectrum that includes acute and chronic viral hepatitis, cirrhosis and hepatocellular carcinoma. While a vaccine is available for HBV and can prevent acute infection, approximately 10% of infected patients develop a chronic lifelong disease with devastating consequences. There is no curative therapy for approximately 300 million patients worldwide who are chronically infected with HBV. Interferon-α (IFNα) provides only partial protection. The need for effective novel therapies for patients infected with the hepatitis C virus (HCV) is even more urgent. HCV is a major causative agent of hepatitis acquired through transfusion or other parenteral routes, with approximately 1–2% of the world’s population being infected with this virus. In contrast to HBV, most of the acutely infected individuals develop a chronic carrier state with eventual progression in some cases to cirrhosis and hepatocellular carcinoma. Currently, no prophylactic or therapeutic vaccines are available. The importance of developing new forms of treatment for HCV is under-scored by the fact that HCV infection is at present the most common indication for liver transplantation in the United States and Europe.
Gene therapy represents a potentially effective strategy for the prevention and treatment of viral hepatitis. Two basic approaches for hepatitis gene therapy are currently being explored. First, nucleic acid-based antiviral approaches, such as antisense oligonucleotides, antisense RNA expressed from transgenes, ribozymes, and expression of dominant negative mutant core proteins in infected hepatocytes have been used to disrupt the life cycle of the viruses. Second, gene therapy approaches to effect antiviral vaccination are being pursued with the development of gene transfer vectors expressing viral antigens, adjuvant cytokines and T-cell costimulatory molecules.
1. Antiviral Strategies
The antiviral strategies are designed to make cells resistant to viral infection by blocking the key steps of the viral life cycle, such as attachment of virus to hepatocytes, internalisation and uncoating, viral gene expression and replication, virus assembly and release. Several strategies have been pursued to design nucleic acid-based antiviral drugs for the treatment of viral hepatitis.[1–3] The basic approaches include the following:
-
1.
Suppression of viral gene transcription by administration of antisense oligonucleotides, triple helix-forming nucleic acids or decoy RNAs, or expressing dominant negative proteins that interfere with viral polymerase activity.
-
2.
Interference with viral RNA by administering antisense oligonucleotides or ribozymes that specifically hybridise with viral RNA, inhibiting its translation, reducing its stability or interfering with its processing.
-
3.
Inhibition of viral function by targeting specific viral proteins through expression of dominant negative mutants or single-chain antibodies that interfere with viral proteases or polymerases, or that disrupt assembly, cell surface binding or internalisation of the virus.
To increase the lifespan of oligonucleotides in vivo, while retaining their biological activity, various modifications have been devised. These include 2′ sugar modification,[4] or generating modified oligonucleotide N3′→ P5′ phosphoramidates, containing 3′-amino instead of 3′-hydroxyl nucleosides.[5] The pharmacokinetic and toxicological issues associated with using the modified oligonucleotides have been reviewed.[6]
For expression of the dominant negative proteins, antisense RNAs or ribozymes, either viral vectors (e.g. recombinant lentivirus, adeno-associated viruses [AAV], simian virus 40 [SV40] or gene-deleted adenoviruses) could be employed. Variousnucleic acid transfer methods have been explored for delivering synthetic oligonucleotides to the liver. Of these, the approaches based on asialoglycoprotein receptor-mediated endo-cytosis appear to be the most promising at this time. The nucleic acids can be non-covalently linked to carriers, such as galactose-terminated peptides,[7] lactosylated polyethyleneimine[8] or galactocerebroside containing liposomes.[9] Following intravenous administration, these complexes are rapidly internalised by the liver and delivered to the hepatocytes.
2. Antiviral Strategies Against Hepatitis B Virus (HBV)
2.1 The HBV Life Cycle
HBV is a member of the hepadna group of DNA viruses, which cause hepatitis in many species. The individual members of the hepadna group have a narrow range of host specificity. HBV, which infects humans and chimpanzees, is a non-cytopathic, enveloped virus. The two DNA strands of its genome are incomplete and partly overlapping (figure 1). The virus replicates asymmetrically through reverse transcription of an RNA intermediate (pregenomic RNA [pRNA]).[10] Although the mechanism of viral entry into the cell is unknown, it is thought to be a receptor-mediated process that eventually leads to the uncoating of the capsid and transport of the released open circular viral genome into the nucleus. In the nucleus, DNA repair enzymes complete the viral plus and minus strands, generating a covalently closed circular (ccc) DNA molecule that serves as the template for viral transcription.
Genomic organisation of hepatitis B virus (HBV): The two strands of genomic DNA (shown in the centre) are partially single stranded, a relaxed circular structure being maintained by short cohesive overlap between the 5′ ends of the two strands. The viral polymerase fills the gaps in the DNA strands during virus replication, giving rise to covalently closed circles. The messenger RNAs (mRNAs) transcribed from the genome are shown in the outer set of circles. There are four overlapping open reading frames (ORFs). The core/precore ORF encodes the core, precore and the e protein. The S ORF encodes the three envelope proteins, S, S+preS2 and S+preS2+preS1. X mRNA encodes only the X protein. The polymerase (POL) is produced by internal translation initiation from the pregenomic RNA.
This viral genome is divided into four domains, which are transcribed into four extensively overlapping transcripts (3.5kb, 2.4kb, 2.1kb, and 0.7kb in length) that are eventually exported into the cytoplasm, where the viral proteins are translated, and viral particle assembly and genome replication occur. The 3.5kb transcript encodes the polymerase, the core, and the precore proteins, and also serves as the pRNA template. Two transcripts, 2.4kb and 2.1kb in length, encode the envelope proteins, including the hepatitis B surface antigen (HBsAg). The 0.7kb transcript encodes the X protein, which in woodchuck hepatitis virus (another member of the hepadna group) has been shown to be a requirement for initiation of infection.
The precore protein contains a leader sequence that transports it into the endoplasmic reticulum (ER), where it is processed and eventually secreted as hepatitis B e antigen (HBeAg). The envelope proteins are cotranslationally inserted into the ER membrane, where they aggregate, bud into the ER lumen, and are released either as free subviral envelope particles or as a part of infectious virions (Dane particles). The core and polymerase proteins assemble around the pRNA to form HBV RNA-containing capsids. It is inside these capsids that the first strand of viral DNA is synthesised by reverse transcription of the RNA. This first strand then serves as the template for the synthesis of the second strand of DNA.
The RNA-containing capsid, as it is maturing into a DNA-containing capsid, can potentially follow two different pathways. One pathway terminates at the ER membrane, where the capsid interacts with envelope proteins, budding into the ER lumen for eventual release as an infectious virion. The second pathway involves the transport of the capsid back to the nucleus, thereby amplifying the pool of cccDNA.[11]
2.2 HBV Antiviral Strategies
Meta-analysis of randomised placebo-controlled studies have shown a benefit of IFNα monotherapy for chronic hepatitis B infection, with the difference between treated and control groups in the proportions of patients with loss of HBeAg and HBV DNA being only 20% while that for loss of HBsAg was only 6%.[12] Nucleoside monotherapy with lamivudine yielded similar results, with a 16–32% rate of seroconversion from HBeAg to anti-HBe with undetectable HBV DNA.[13] Combination therapy with IFNα and lamivudine in three multicenter trials showed either a marginal benefit of combination therapy, or failed to show any benefit at all.[13,14] Nucleic acid-based antiviral approaches for HBV include the use of antisense oligonucleotides and RNA, ribozymes, DNA-based therapeutic vaccines and dominant negative mutant core proteins that disrupt the life cycle of HBV. Since the structural heterogeneity among HBV-DNA species is much less than that seen in RNA viruses, such as human immunodeficiency viruses, there are potential advantages of nucleic acid-based therapies.
Antisense oligonucleotides and RNA may be potentially advantageous, as viral replication involves the synthesis of a 3.5kb pRNA intermediate. Synthetic antisense therapy involving oligodeoxynucleotides (ODN) coupled to polylysine attached to asialoglycoproteins has been shown to decrease the amount of newly synthesised core-associated viral DNA, with a concomitant decrease in HBV viral RNA transcripts and HBsAg expression. In vitro models have shown that antisense RNA targeting intracellular HBV transcripts can inhibit HBV replication and antigen expression.[7,10,15] In an in vivo duck hepatitis (DHV) infection model, intravenous injection of linear polyethylenimine-complexed antisense phosphodiester ODNs, targeted to the initiation codons of the viral envelope protein, specifically suppressed hepadnaviral replication.[16] The widespread use of antisense ODN and RNA therapy, however, has been hampered by an inability to achieve required intracellular concentrations of antisense ODNs and RNAs, largely as a result of their instability in complex protein mixtures and by a lack of cell-specific delivery systems.
Another possible approach involves the use of ribozymes, which are short catalytic RNA molecules possessing endoribo-nuclease activity. The specificity of the enzyme is imparted by variable flanking sequences complementary to the RNA target substrate. Hammerhead ribozymes have been generated that cleave HBV pRNA.[3] A combinatorial hairpin ribozyme library was screened to identify hairpin ribozymes that inhibit HBV replication in transfected human hepatocellular carcinoma cells.[17] Recombinant retrovirus vectors expressing specific ribozymes targeting the pRNA, RNAs for HBsAg, HBV polymerase and X protein have been generated and tested in vitro. Expression of these modified hairpin ribozymes attenuated HBV replication by 83% in HuH7 cells.[18]
The characterisation of the HB V genome and elucidation of viral protein structure have provided an alternative to antisense and ribozyme therapy. The synthesis of dominant negative poly-peptides that interact with and/or disrupt the function of their native counterparts offers another method of inhibiting viral replication. Scaglioni et al.[19] have generated and functionally characterised dominant negative core protein variants of the HBV. Plasmids expressing a truncated core protein fused in frame with the C-terminus of HBsAg inhibited viral replication by 90–95% by disrupting viral nucleocapsid assembly and preventing encapsidation of pRNA. The dominant negative core mutants can also serve as potential intracellular immunogens. Gene therapy with recombinant retroviral and adenoviral vectors expressing these mutants partly inhibited viral replication in hepatoma cell lines constitutively expressing replicating wild type virus.[20]
3. Antiviral Strategies Against Hepatitis C Virus (HCV)
3.1 The HCV Life Cycle
The mechanism of HCV entry into the cell is still poorly understood, although low density lipoprotein (LDL) and CD81 may potentially play a role as key cellular receptors. LDL and very low density lipoprotein molecules are reported to be associated with HCV particles in the circulation of infected humans. Furthermore, the LDL receptor has been shown to transport HCV particles across the cell membrane. CD81, a ubiquitously expressed tetraspan molecule, also binds to the viral envelope protein E2, although the functional significance of this interaction is yet to be determined. After HCV binds to its cellular receptor, the lipid envelope dissociates, and the RNA genome and the structural proteins are delivered into the cytoplasm. Once inside, the HCV genome utilises the host ribosomes to translate viral RNA into viral proteins.
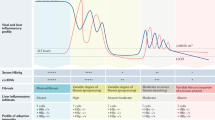
The HCV genome is a 9.5kb, single-stranded, positive-sense RNA possessing a single coding region and two flanking noncoding regions (figure 2). The coding region contains genetic information for three structural proteins (core, envelope 1, envelope 2) and six nonstructural (NS2 to 5) proteins. Both groups of proteins have been implicated in modulating the host immune response and carcinogenesis. The flanking noncoding regions (the 5′untranslated region [5′UTR] and 3′UTR) are unique RNA molecules that manipulate the host cell machinery into translating the viral genome.
Genomic organisation of hepatitis C virus (HCV): The 9.5-kb single-stranded RNA genome contains 5′and 3′untranslated regions (UTRs) and a single open reading frame. The 5′UTR contains a 341-nt internal ribosomal entry site (IRES), which is needed for translation. The 3′UTR contains a U-U/C-rich region and three highly conserved stem loop structures. The polyprotein expressed from the single open reading frame is cleaved by cellular signal peptidase (at sites indicated by open arrows) to generate the structural proteins, C, E1, E2 and probably P7. The viral proteases cleave the remainder of the polyprotein (at sites indicated by solid arrows) to generate the non-structural proteins (NS).
Translation of the genomic RNA is initiated by a highly conserved secondary structure within the 5′UTR called the internal ribosome entry site (IRES), which permits the engagement of the host ribosome. The IRES forms a binary complex with the 40S ribosomal subunit in the absence of host translation initiation factors. This complex viral RNA element is therefore a logical target for designing antiviral therapies. Translation proceeds in the 5′ to 3′ direction, producing a single viral polyprotein that is subsequently cleaved into individual viral proteins by action of the host signal peptidase, and the viral proteases, NS2-3 auto-protease and NS3-4A serine protease. Thus, the NS3 is an attractive target for antiviral therapy of HCV, and specific inhibitors of its substrate binding site are being designed.[21]
Post-translational viral replication occurs after the nonstructural protein NS5B, the viral RNA polymerase, copies the original infecting viral RNA via a negative strand intermediate. In the meantime, the NS3 protein unravels these growing RNA strands to allow their packaging with viral particles containing core and envelope (E1 and E2) proteins. The packaged virus is then exported extracellularly via poorly understood mechanisms.[22]
3.2 Interference with the HCV Life Cycle
Current treatment regimens for HCV hepatitis include the use of IFNα and ribavirin, usually in combination.[23] A randomised trial compared high-dose pegylated IFNα-2b plus ribavirin with nonpegylated IFNα-2b plus ribavirin.[24] This study showed a significantly higher sustained viral response rate of 54% for the higher-dose peginterferon group than the lower-dose and nonpegylated IFN groups. However, the rate of long-term remission of the disease after these treatments is relatively low and the sustained viral response rate is 36–41% after a 24-or 48-week course of combination therapy.[21] Newer approaches targeting specific points within the viral life cycle may lead to novel therapies. For example, the HCV IRES, which is required for translation of HCV RNA, is highly conserved across 39 different isolates and genotypes of HCV. Targeting this sequence with antisense ODN and RNA or ribozymes could have therapeutic benefits. Antisense RNA targeted against the IRES reduces reporter gene expression by 41–57%. Similarly, antisense ODN, targeted to this region, efficiently reduced HCV RNA translation.[25,26] Welch et al.[27] constructed ribozymes targeted to the 5′UTR of HCV RNA and the capsid gene regions (C). These ribozymes inhibited the expression of a cotransfected reporter gene construct, containing HCV RNA target sequences. Adenoviral vectors expressing the most effective of these ribozymes inhibited HCV core expression in a tissue culture model.[28] Hammerhead ribozymes designed to cleave at nt 136–160, 313–337, 496–520, and 373–388 of the HCV RNA, substantially and specifically inhibited viral gene expression.[29] Similarly, synthetic nuclease-resistant hammerhead ribozymes targeting various conserved sites within the 5′UTR of the HCV RNA inhibited the replication of a HCV/polio virus chimera.[30] IFNs potentiated the ribozyme effect.[31] These ribozymes, expressed from recombinant adenovirus vectors, individually or in combination, efficiently reduced or eliminated the respective plus- or minus-strand HCV RNAs in cultured cells and primary hepatocytes obtained from chronic HCV-infected patients.[32]
4. DNA Vaccines
Vaccination could potentially eradicate chronic hepatitis. Effective vaccination against viral hepatitis should induce two arms of the antiviral immune response, humoral and cell-mediated immunity. First, these vaccines should generate protective neutralising antibodies that would prevent acute viral infection. Second, an effective viral vaccine should stimulate cell-mediated immunity that would eradicate virally infected cells from chronic carriers of hepatitis. Generation of virus-specific CD8+ cytotoxic T lymphocytes (CTL) can induce apoptosis and lyse the virus-infected hepatocytes directly. They can also secrete cytokines, IFNγ and tumour necrosis factor-α, which suppress HBV gene expression and viral replication.[11,33] Protein subunit vaccines have been developed for hepatitis A and B viruses. A protein subunit vaccine for hepatitis B is used universally and has been shown to prevent new infection and decrease the incidence of hepatocellular carcinoma in Taiwanese children.[34,35] However, these vaccines are unable to stimulate anti-viral cell-mediated immunity. The immunogenicity of selected HBV envelope- or capsid-based vaccine formulations is currently under study in animal models and clinical trials for the induction or broadening of T- and B-cell responses in HBV chronic carriers.[36] Because of poor antigenicity and genetic variations in the HCV envelope proteins, effective vaccines against HCV have not yet been developed.
DNA-based vaccination might provide several important advantages over current vaccines. They are potent in inducing both humoral and major histocompatibility complex (MHC) class I-restricted CD8+ CTL responses. DNA vaccines against HBsAg and core proteins induced a strong antiviral immune response in mice, pigs and monkeys.[37] A transgenic mouse model, which is deficient for mouse MHC class I molecules (β(2)-micro-globulin(−/−) D(b−/−)) and transgenic for a chimeric human leucocyte antigen (HLA)-A*0201/D(b) molecule covalently bound to the human β(2)-microglobulin HHD(+/+), was used for DNA-based immunisation with plasmid vectors expressing the small and the middle HBsAg.[38] Genetic immunisation induced strong CTL responses to several HLA-A*0201-restricted epitopes of HBV envelope proteins. Moreover, genetic immunisation of HLA-A2 transgenic mice induced IFNγ-secreting CD8(+) T lymphocytes specific for endogenously processed peptides and with recognition specificities similar to those described during self-limited infection in humans.[38] Thus, by inducing immune responses closely related to those involved in clearing the virus from the host, DNA vaccines may represent an alternative therapeutic approach for chronic HBV infection.[39] DNA vaccines mimic the effects of live attenuated vaccines in their ability to induce cell-mediated immunity against intracellular pathogens, while avoiding additional safety concerns. DNA vaccines can even ‘override’ CTL nonresponder status in preclinical animal models. For example, after intramuscular injection of plasmid DNA encoding HBsAg, both Kb- and Db-restricted CTL reactivity to HBsAg emerged in H-2b mice, whereas priming of anti-HBsAg CTL was not detectable after injecting recombinant HBsAg or inoculating with a recombinant vaccinia virus expressing HBsAg.[40] Thus, DNA vaccination induced a class I-restricted CTL response to HBsAg in a mouse strain previously considered to be a nonresponder at the CTL level.[40] It is possible to express and immunise against a wide spectrum of antigens and epitopes of multiple antigens by DNA vaccines. A DNA encoding nine dominant HLA-A2.1- and A11-restricted epitopes from the HBV polymerase, envelope, and core protein, together with the PADRE (pan-DR epitope), universal T-helper cell epitope and an ER-translocating signal sequence, was used to immunise HLA transgenic mice. CTL induction was demonstrated against all nine CTL epitopes despite their varying MHC binding affinities.[41] Similarly, intramuscular and intradermal injections of a DNA expression vector encoding an epitope of the human immunodeficiency virus envelope fused to the surface protein of the HBV (HBsAg) induced strong humoral and cytotoxic responses to antigenic determinants of both viruses in mice and nonhuman primates.[42] To enhance the immunogenicity of the non-secreted HCV structural proteins, several chimeric HBV-HCV constructs were used for vaccination in mice. These chimeric vaccines were capable of generating CD4+ Th1 cells and CD8+ CTL activity against both HBV and HCV components of the fusion proteins.[43,44] These results indicate that it might be possible to rationally design expression vectors to induce multispecific immune responses for vaccination against various hepatitis viruses and other pathogens. DNA vaccines can be produced on a large scale and stored with relative ease compared with conventional vaccines.
Expression plasmids used for vaccination consist of the transcription (antigen expression) unit composed of the promoter/enhancer sequences and the transgene and the prokaryotic vector backbone composed of bacterial sequences necessary for plasmid amplification (origin of replication) and antibiotic resistance. Bacterial DNA contains abundant unmethylated cytidine-phosphate-guanosine (CpG) dinucleotide motifs with appropriate flanking regions that elicit an innate immune response. These motifs have been shown to induce the secretion of IFNγ and interleukin-12 by dendritic cells (DCs), which in turn activate natural killer (NK) cells[45] and bias the T-helper cells toward the Th1 pathway.[46] Thus, the bacterial DNA serves as an adjuvant in DNA vaccines and induces a Th1-CTL response against the expressed antigens. The mechanism by which the antigen encoded by the transgene is processed and presented to the immune system is intriguing because the quantity of the antigen produced in vivo is in the picogram to nanogram range.[47] It is likely that the host antigen-presenting cells (APC), rather than the predominant cell type of the tissue into which the DNA is injected (e.g. myocytes or keratinocytes), directly induce immune response after DNA vaccination.[47] The myocytes and keratinocytes may constitute a reservoir, from which professional APCs (e.g. DCs) may take up the antigens by phagocytosis of apoptotic or necrotic bodies.[47,48] This process, termed crosspriming, is confirmed by the finding that DCs could effectively present nonsecreted antigens expressed by dying, irradiated keratinocytes.[48] Although nonviral vectors are generally used for genetic immunisation studies, viral vectors, such as recombinant retrovirus,[49] varicella[50] or SV40,[51] have been used for immunisation against HBsAg. While most viral vectors are not suitable for multiple injections because of the development of neutralising antibodies, recombinant T-antigen-deleted SV40 vectors may be suitable for primary and booster immunisation, since the viral structural proteins do not evoke a neutralising antibody response even after multiple injections.[51]
4.1 HBV DNA Vaccines
The HBsAg is a well characterised molecule where the anti-genic epitopes have been mapped out. Three proteins are present in the envelope of the HBV virions, all of which contain HBsAg. These are the large (L) surface antigen (sAg, PreS1/preS2/S), the middle (M) sAg (preS2/S) and the small sAg antigen. Transfected cells secrete the middle and small sAgs, but the large sAg remains intracellularly. The S120–147 region of the small sAg contains the conformational ‘a’ epitope that is recognised by most human and murine anti-HBsAg antibodies. Intramuscular injection of plasmid DNA encoding the intracellular HBV L envelope protein induced only a weak humoral response in mice, whereas a vector expressing the secretion-competent S envelope protein evoked strong and sustained immunity.[52] The humoral response to the HBV L sAg requires the accessibility of preS antigens to B cells. The accessibility was increased by immunisation with modified small and M envelope genes that were fused to C-terminally attached epitopes, derived from the preS1 region of the L gene. The secretion of the fusion proteins induced higher titres of preS1- and preS2-specific antibodies. Thus, DNA constructs carrying preS1 determinants are promising candidates for the development of multivalent HBV vaccines.[52]
4.2 HCV DNA Vaccines
The immune response to HCV is a critical determinant of either viral clearance or establishment of the carrier state and chronic liver injury. Vaccine development against HCV is urgently needed because of the escalating burden to healthcare of chronically infected patients. The HCV RNA replication is error prone because of the lack of proofreading capacity of the RNA polymerase. This allows the virus to mutate rapidly as it adapts to the environment, leading to high sequence divergence among viral isolates from various parts of the world. The highest sequence variability occurs in the hypervariable region of the envelope glycoprotein E2, which also carries an epitope for neutralising antibodies. Strategies for HCV vaccination have been reviewed recently.[53,54] Although the types of immune response responsible for viral clearance versus persistence and chronic liver injury have not yet been defined, it is clear that generation of T-helper cells and specific cytotoxic T cells are required for HCV clearance, in addition to high-titre cross-reactive neutralising antibodies.
Major et al.[44] constructed vectors expressing the first 58 amino acids of the HCV nucleocapsid alone or as a fusion protein with the middle (pre-S2 and S) or major (S) surface antigens of HBV. Intramuscular immunisation of the chimeric plasmid DNA in BALB/c mice elicited humoral responses to antigens from both viruses within 2–6 weeks postinjection. This was the first report of the use of DNA-based immunisation for the generation of immune responses to an HCV protein and demonstrated that it was possible to elicit responses to viral epitopes from two distinct viruses via DNA immunisation with chimeric vectors. Since the envelope glycoprotein E2 binds to hepatocyte cell surface protein CD81, this protein is a potential vaccine candidate, especially to induce neutralising antibodies. Truncated E2 proteins isolated from cytosolic preparations are effective in inducing highly active and long-lasting antibody response.[55] The cellular and humoral response to the E2 protein was enhanced by electrical gene transfer into muscles of mice.[56] Although an E2 plasmid vaccine failed to induce sterilising immunity in a chimpanzee model, it appeared to prevent progression to chronicity.[57]
The core antigen is another logical target for HCV DNA vaccines because it is the most conserved HCV protein among various genotypes.[58] No mutation was detected in HCV-infected patients within the core gene, despite the presence of a strong CTL response.[59] The absence of CTL escape mutants in the core antigen makes it an attractive target for protective immunity. In Balb/c mice, plasmid constructs expressing HCV core protein generate strong CTL activity.[60] However, there are concerns about developing a DNA vaccine against core protein antigens because this protein could modulate multiple cellular processes, such as apoptosis, lipid metabolism, RNA transcription and cell transformation.[61] Thus, subunit vaccines in the nonclassical immunostimulatory complexes (ISCOM) formulation, in which the core protein was adsorbed onto (not entrapped within) the ISCOMATRIX, are being tested in rhesus macaque monkeys.[62]
DNA vaccines against the HCV nonstructural proteins, NS3, NS4, and NS5, induce CD8+ CTL activity in Balb/c mice.[63] The vaccinated mice were able to reject a syngeneic tumour expressing NS5 upon challenge. The immune response to various DNA formulations of HCV NS3 was investigated in a HLA-A2.1 transgenic mouse model.[64] Plasmids expressing NS3 as a fusion protein with murine lysosome-associated-membrane protein-1 (LAMP) showed a vigorous and long-lasting CTL response. The HLA-A2.1 transgenic mice were also used to test an oral vaccine with attenuated HCV-NS3-transformed Salmonella typhimurium.[65] This strategy induced strong cytotoxic and IFNγ-producing CD8+ T cells that persisted for at least 10 months. The immunological response to HCV expression plasmids, expressing HCV structural proteins (core, E1 and E2), was examined in HCV transgenic mice.[66] Both wild type and transgenic mice immunised with these constructs produced antibodies and exhibited T-cell proliferative response against core and envelope proteins. There was no CTL response against envelope proteins, although an anti-core CTL response was induced. Additionally, neither lymphocytic infiltrate in the liver nor hepatic inflammation was induced, despite the development of peripheral immunity. Recently, a recombinant tobacco mosaic virus expressing a consensus sequence of the hypervariable region 1 (HVR1) of the HCV envelope protein, genetically fused to the C-terminal of the B subunit of cholera toxin (CTB) was used to infect plants. Intranasal immunisation of mice with crude extracts from the infected plants containing the recombinant HVR1/CTB protein elicited both anti-CTB and anti-HVR1 antibodies that bound specifically to HCV virus particles.[67]
5. Gene Therapy Vectors
In theory, successful antiviral gene therapy should require gene transfer to a great majority of both quiescent and dividing hepatocytes. To counter viral replication, high intracellular levels of the anti-viral genetic constructs would be required to be present inside the cell for a period long enough to clear the cccHBV-DNA template, thereby eradicating chronic viral infection. Although no single vector possesses all these desirable characteristics, the available variety of gene transfer vehicles should allow application tailored to specific needs. Hepatocellular gene delivery systems can be based on non-viral or viral methods.
Non-viral methods that have produced promising results include the use of DNA-ligand or DNA-lipid complexes, both of which may be targeted to the hepatocytes, utilising specific cell surface endocytotic receptors, such as the asialoglycoprotein receptor.[15,68,69] Similarly, a linear polyethylenimine-based delivery system has been used to deliver antisense phosphodiester oligo-nucleotides directed against the initiation codons of DHV large envelope antigen. This procedure effectively blocked DHV expression in vivo.[16] However, the effect of transfection with simple DNAs is usually transient. Recently, the ‘Sleeping Beauty’ transposase, a member of the Tc1/mariner transposon family, was shown to bind the inverted repeats of salmonid transposons in a substrate-specific manner, mediating precise cut-and-paste trans-position into chromosomes of fish, mouse and human cells.[70] This system was used for random insertion of a therapeutic transgene in chromosomes of mouse hepatocytes, resulting in long-term expression of human blood coagulation factor IX.[71] Use of the transposon-transposase system may enable transfected DNA to be integrated at a high frequency within cellular genomes in vivo.
Currently, recombinant viruses are the most common vehicles used for gene delivery. Stable transduction with long-term gene expression is a major advantage for viruses that integrate in the host genome, but risk of insertional mutagenesis and/or repression of the transgene expression following integration are theoretical concerns. Vectors that integrate into the host genome include recombinant retroviruses (including leukaemia and lentiviruses), adeno-associated virus (AAV) and SV40. However, recent studies indicate that recombinant AAV may mostly persist at concatamerized episomal DNA.
Leukaemia-type retroviruses infect non-dividing cells at a low frequency, making them inefficient for gene transfer into quiescent hepatocytes. Despite these limitations, retroviral vectors have been designed to express antisense RNA to HBV surface antigen for targeted inhibition of HBV gene expression.[72] Similarly, retroviral vectors expressing dominant negative core mutants of HBV virus were used to inhibit wild-type HBV replication.[20] Recombinant lentivirus vectors can infect non-dividing cells, and HIV-based vectors, pseudotyped with vesicular stomatitis virus G (VSV-G) protein, are being developed for hepatic gene transfer.[73]
AAV-2 vectors can be grown at high titres and show promise in long-term gene transfer. AAV vectors can infect non-dividing cells, persist as episomal concatamers and express the transgene for a long time. Hepatic expression of coagulation factor IX occurred after infection with a recombinant AAV vector expressing factor IX from a thyroid hormone-binding globulin promoter/α1-microglobulin/bikunin enhancer.[74] With current techniques, approximately 5% of the hepatocytes can be transduced in vivo using recombinant AAV vectors.
A new recombinant vector, based on large T-antigen-deleted SV40, is capable of infecting both dividing and non-dividing cells, and expressing transgenes for a prolonged period.[75] The recombinant virus appears to be non-immunogenic, has high transduction efficiency (> 90% without selection), is present as both integrated and episomal forms, and can be developed at high titres.[76] Successful development of this vector may permit transduction of a majority of hepatocytes.
Episomal viral vectors include the recombinant adenoviral and the Epstein-Barr viral vectors. Adenovirus-based vectors are the most powerful gene transfer vehicles for gene transfer into the rodent or mouse liver.[77] However, the gene transfer efficiency of these vectors is much lower in primates, including humans. Although these vectors can be generated at high titres, can express transgenes in both dividing and non-dividing cells and have a broad species range, a strong humoral and cellular immune response to the vector proteins precludes repeated gene transfer with these vectors. ‘Gutless’ virus vectors, in which the genes for the viral structural proteins are deleted or mutated,[78] express transgenes for a longer duration, but remain immunogenic.[79] Recently, recombinant adenoviruses coexpressing the immuno-modulatory gene, CTLA4Ig, together with the target transgene, have been shown to be non-immunogenic, and have permitted repeated gene transfer into rodents.[80] However, since high blood levels of CTLA4Ig prevent costimulatory pathways operating between APCs and T cells, these vectors may cause temporary immune incompetence. Hybrid adenoviruses containing elements of other viruses, e.g. retroviruses[81] and AAV[82] that promote integration, are being developed. Furthermore, the tropism of these vectors is being altered to improve the infection efficiency of human hepatocytes. Another strategy for the development of hybrid vectors is to use vectors derived from the Epstein-Barr virus (EBV). EBV vectors contain an origin of replication (oriP) and a virus-encoded cofactor (EBNA-1), which together allow replication of the DNA within the nucleus in synchrony with the host chromosomal DNA.[83] The EBV-based episomal vectors can persist in the nucleus at 10 to 100 copies per cell without integrating in the host chromosome. Exploiting this system, a novel adenoviral/EBV episomal vector was designed that resulted in efficient long-term transgene expression following Cre/loxP site-specific excision of an EBV-derived episome from the hybrid vector.[84]
6. Conclusion
Despite the availability of effective vaccines for hepatitis B and incremental improvement in the drug therapy for both hepatitis B and C, both forms of viral hepatitis continue to impose a major disease burden on all nations of the world. While it is expected that universal vaccination will eventually reduce the incidence of hepatitis B, no effective prophylaxis is as yet available for hepatitis C. Novel nucleic acid-based approaches for the two types of viral hepatitis consist of DNA-based vaccination and treatments that interfere with the generation, assembly and survival of the viruses. Gene therapy methods that directly interfere with viral biology, such as antisense RNAs, ribozymes or dominant negative proteins, need to be delivered to or be expressed in the great majority of infected cells. Moreover, these therapies, as well as the expression of cytokines, are usually virostatic, but do not eradicate the virus. Thus, it is expected that a major focus of investigations will continue to be improved prophylaxis for these two disorders, particularly hepatitis C. Hurdles to the development of effective DNA-based prophylaxis include the low level of expression of antigens after intramuscular injection of DNA, inefficient antigen presentation, low immunogenicity of many of the viral proteins, and a high mutation rate of the viral epitopes. Effort is being directed at solving these problems using improved vectors, gene transfer to tissues other than skeletal muscles, administering or coexpressing cytokines that enhance the antigen-presenting cells, and expressing multiple epitopes simultaneously. It is expected that the effort of numerous innovative investigators will culminate in the availability of effective nucleic acid-based prophylaxis and therapy for these viral infections in the foreseeable future.
References
Ruiz J, Qian C, Drozdzik M, et al. Gene therapy of viral hepatitis and hepatocellular carcinoma. J Viral Hepat 1999; 6: 17–34
von Weizsacker F, Wieland S, Kock J, et al. Gene therapy for chronic viral hepatitis: ribozymes, antisense oligonucleotides, and dominant negative mutants. Hepatology 1997; 26: 251–5
Wands JR, Geissler M, Putlitz JZ, et al. Nucleic acid-based antiviral and gene therapy of chronic hepatitis B infection. J Gastroenterol Hepatol 1997; 12: S354–69
Manoharan M. 2′-carbohydrate modifications in antisense oligonucleotide therapy: importance of conformation, configuration and conjugation. Biochim Biophys Acta 1999; 1489: 117–30
Gryaznov SM. Oligonucleotide N3′→P5′ phosphoramidates as potential therapeutic agents. Biochim Biophys Acta 1999; 1489: 131–40
Levin AA. A review of the issues in the pharmacokinetics and toxicology of phos-phorothioate antisense oligonucleotides. Biochim Biophys Acta 1999; 1489: 69–84
Wu J, Gerber MA. The inhibitory effects of antisense RNA on hepatitis B virus surface antigen synthesis. J Gen Virol 1997; 78: 641–7
Kren BT, Parashar B, Bandyopadhyay P, et al. Correction of the UDP-glucuronosyltransferase gene defect in the gunn rat model of crigler-najjar syndrome type I with a chimeric oligonucleotide. Proc Natl Acad Sci U S A 1999; 96: 10349–54
Kren BT, Bandyopadhyay P, Chowdhury NR, et al. Oligonucleotide-mediated site-directed gene repair. Methods Enzymol 2002; 346: 14–35
zu Putlitz J, Wieland S, Blum HE, et al. Antisense RNA complementary to hepatitis B virus specifically inhibits viral replication. Gastroenterology 1998; 115: 702–13
Chisari FV. Rous-Whipple Award Lecture: viruses, immunity, and cancer: lessons from hepatitis B. Am J Pathol 2000; 156: 1117–32
Wong DK, Cheung AM, O’Rourke K, et al. Effect of alpha-interferon treatment in patients with hepatitis B e antigen-positive chronic hepatitis B: a meta-analysis. Ann Intern Med 1993; 119: 312–23
Yuen MF, Lai CL. Treatment of chronic hepatitis B. Lancet Infect Dis 2001; 1: 232–41
Barbaro G, Zechini F, Pellicelli AM, et al. Long-term efficacy of interferon alpha-2b and lamivudine in combination compared to lamivudine monotherapy in patients with chronic hepatitis B: an Italian multicenter, randomized trial. J Hepatol 2001; 35: 406–11
Wu GY, Wu CH. Specific inhibition of hepatitis B viral gene expression in vitro by targeted antisense oligonucleotides. J Biol Chem 1992; 267: 12436–9
Robaczewska M, Guerret S, Remy JS, et al. Inhibition of hepadnaviral replication by polyethylenimine-based intravenous delivery of antisense phosphodiester oligodeoxynucleotides to the liver. Gene Ther 2001; 8: 874–81
zu Putlitz J, Yu Q, Burke JM, et al. Combinatorial screening and intracellular antiviral activity of hairpin ribozymes directed against hepatitis B virus. J Virol 1999; 73: 5381–7
Welch PJ, Tritz R, Yei S, et al. Intracellular application of hairpin ribozyme genes against hepatitis B virus. Gene Ther 1997; 4: 736–43
Scaglioni PP, Melegari M, Wands JR. Characterization of hepatitis B virus core mutants that inhibit viral replication. Virology 1994; 205: 112–20
Scaglioni P, Melegari M, Takahashi M, et al. Use of dominant negative mutants of the hepadnaviral core protein as antiviral agents. Hepatology 1996; 24: 1010–7
Di Bisceglie AM, McHutchison J, Rice CM. New therapeutic strategies for hepatitis C. Hepatology 2002; 35: 224–31
Drazan KE. Molecular biology of hepatitis C infection. Liver Transpl 2000; 6: 396–406
McHutchison JG. Hepatitis C advances in antiviral therapy: what is accepted treatment now? J Gastroenterol Hepatol 2002; 17: 431–41
Manns MP, McHutchison JG, Gordon SC, et al. Peginterferon alfa-2b plus ribavirin compared with interferon alfa-2b plus ribavirin for initial treatment of chronic hepatitis C: a randomised trial. Lancet 2001; 358: 958–65
Wakita T, Wands JR. Specific inhibition of hepatitis C virus expression by antisense oligodeoxynucleotides: in vitro model for selection of target sequence. J Biol Chem 1994; 269: 14205–10
Wakita T, Moradpour D, Tokushihge K, et al. Antiviral effects of antisense RNA on hepatitis C virus RNA translation and expression. J Med Virol 1999; 57: 217–22
Welch PJ, Tritz R, Yei S, et al. A potential therapeutic application of hairpin ribozymes: in vitro and in vivo studies of gene therapy for hepatitis C virus infection. Gene Ther 1996; 3: 994–1001
Welch PJ, Yei S, Barber JR. Ribozyme gene therapy for hepatitis C virus infection. Clin Diagn Virol 1998; 10: 163–71
Sakamoto N, Wu CH, Wu GY. Intracellular cleavage of hepatitis C virus RNA and inhibition of viral protein translation by hammerhead ribozymes. J Clin Invest 1996; 98: 2720–8
Macejak DG, Jensen KL, Jamison SF, et al. Inhibition of hepatitis C virus (HCV)-RNA-dependent translation and replication of a chimeric HCV poliovirus using synthetic stabilized ribozymes. Hepatology 2000; 31: 769–76
Macejak DG, Jensen KL, Pavco PA, et al. Enhanced antiviral effect in cell culture of type 1 interferon and ribozymes targeting HCV RNA. J Viral Hepat 2001; 8: 400–5
Lieber A, He CY, Polyak SJ, et al. Elimination of hepatitis C virus RNA in infected human hepatocytes by adenovirus-mediated expression of ribozymes. J Virol 1996; 70: 8782–91
Guidotti LG, Ishikawa T, Hobbs MV, et al. Intracellular inactivation of the hepatitis B virus by cytotoxic T lymphocytes. Immunity 1996; 4: 25–36
Chang MH, Chen CJ, Lai MS, et al. Universal hepatitis B vaccination in Taiwan and the incidence of hepatocellular carcinoma in children. Taiwan Childhood Hepatoma Study Group. N Engl J Med 1997; 336: 1855–9
Zuckerman AJ. Prevention of primary liver cancer by immunization. N Engl J Med 1997; 336: 1906–7
Michel ML, Pol S, Brechot C, et al. Immunotherapy of chronic hepatitis B by anti HBV vaccine: from present to future. Vaccine 2001; 19: 2395–9
Fuller JT, Fuller DH, McCabe D, et al. Immune responses to hepatitis B virus surface and core antigens in mice, monkeys, and pigs after Accell particle-mediated DNA immunization. Ann N Y Acad Sci 1995; 772: 282–4
Loirat D, Lemonnier FA, Michel ML. Multiepitopic HLA-A*0201-restricted immune response against hepatitis B surface antigen after DNA-based immunization. J Immunol 2000; 165: 4748–55
Michel ML, Loirat D. DNA vaccines for prophylactic or therapeutic immunization against hepatitis B. Intervirology 2001; 44: 78–87
Schirmbeck R, Bohm W, Ando K, et al. Nucleic acid vaccination primes hepatitis B virus surface antigen-specific cytotoxic T lymphocytes in nonresponder mice. J Virol 1995; 69: 5929–34
Ishioka GY, Fikes J, Hermanson G, et al. Utilization of MHC class I transgenic mice for development of minigene DNA vaccines encoding multiple HLA-restricted CTL epitopes. J Immunol 1999; 162: 3915–25
Le Borgne S, Mancini M, Le Grand R, et al. In vivo induction of specific cytotoxic T lymphocytes in mice and rhesus macaques immunized with DNA vector encoding an HIV epitope fused with hepatitis B surface antigen. Virology 1998; 240: 304–15
Geissler M, Tokushige K, Wakita T, et al. Differential cellular and humoral immune responses to HCV core and HBV envelope proteins after genetic immunizations using chimeric constructs. Vaccine 1998; 16: 857–67
Major ME, Vitvitski L, Mink MA, et al. DNA-based immunization with chimeric vectors for the induction of immune responses against the hepatitis C virus nucleocapsid. J Virol 1995; 69: 5798–805
Ballas ZK, Rasmussen WL, Krieg AM. Induction of NK activity in murine and human cells by CpG motifs in oligodeoxynucleotides and bacterial DNA. J Immunol 1996; 157: 1840–5
Klinman DM, Yi AK, Beaucage SL, et al. CpG motifs present in bacteria DNA rapidly induce lymphocytes to secrete interleukin 6, interleukin 12, and interferon gamma. Proc Natl Acad Sci U S A 1996; 93: 2879–83
Gurunathan S, Klinman DM, Seder RA. DNA vaccines: immunology, application, and optimization. Annu Rev Immunol 2000; 18: 927–74
Akbari O, Panjwani N, Garcia S, et al. DNA vaccination: transfection and activation of dendritic cells as key events for immunity. J Exp Med 1999; 189:169–78
Sallberg M, Townsend K, Chen M, et al. Characterization of humoral and CD4+ cellular responses after genetic immunization with retroviral vectors expressing different forms of the hepatitis B virus core and e antigens. J Virol 1997; 71: 5295–303
Shiraki K, Hayakawa Y, Mori H, et al. Development of immunogenic recombinant Oka varicella vaccine expressing hepatitis B virus surface antigen. J Gen Virol 1991; 72: 1393–9
Kondo R, Feitelson MA, Strayer DS. Use of SV40 to immunize against hepatitis B surface antigen: implications for the use of SV40 for gene transduction and its use as an immunizing agent. Gene Ther 1998; 5: 575–82
Prange R, Werr M. DNA-mediated immunization to hepatitis B virus envelope proteins: preS antigen secretion enhances the humoral response. Vaccine 1999; 17: 617–23
Hsu HH, Abrignani S, Houghton M. Prospects for a hepatitis C virus vaccine. Clin Liver Dis 1999; 3: 901–15
Lechmann M, Liang TJ. Vaccine development for hepatitis C. Semin Liver Dis 2000; 20: 211–26
Heile JM, Fong YL, Rosa D, et al. Evaluation of hepatitis C virus glycoprotein E2 for vaccine design: an endoplasmic reticulum-retained recombinant protein is superior to secreted recombinant protein and DNA-based vaccine candidates. J Virol 2000; 74: 6885–92
Zucchelli S, Capone S, Fattori E, et al. Enhancing B- and T-cell immune response to a hepatitis C virus E2 DNA vaccine by intramuscular electrical gene transfer. J Virol 2000; 74: 11598–607
Forns X, Payette PJ, Ma X, et al. Vaccination of chimpanzees with plasmid DNA encoding the hepatitis C virus (HCV) envelope E2 protein modified the infection after challenge with homologous monoclonal HCV. Hepatology 2000; 32: 618–25
Bukh J, Purcell RH, Miller RH. Sequence analysis of the core gene of 14 hepatitis C virus genotypes. Proc Natl Acad Sci U S A 1994; 91: 8239–43
Christie JM, Chapel H, Chapman RW, et al. Immune selection and genetic sequence variation in core and envelope regions of hepatitis C virus. Hepatology 1999; 30: 1037–44
Tokushige K, Wakita T, Pachuk C, et al. Expression and immune response to hepatitis C virus core DNA-based vaccine constructs. Hepatology 1996; 24: 14–20
McLauchlan J. Properties of the hepatitis C virus core protein: a structural protein that modulates cellular processes. J Viral Hepat 2000; 7: 2–14
Polakos NK, Drane D, Cox J, et al. Characterization of hepatitis C virus core-specific immune responses primed in rhesus macaques by a nonclassical ISCOM vaccine. J Immunol 2001; 166: 3589–98
Encke J, zu Putlitz J, Geissler M, et al. Genetic immunization generates cellular and humoral immune responses against the nonstructural proteins of the hepatitis C virus in a murine model. J Immunol 1998; 161: 4917–23
Brinster C, Muguet S, Lone YC, et al. Different hepatitis C virus nonstructural protein 3 (Ns3)-DNA-expressing vaccines induce in HLA-A2.1 transgenic mice stable cytotoxic T lymphocytes that target one major epitope. Hepatology 2001; 34: 1206–17
Wedemeyer H, Gagneten S, Davis A, et al. Oral immunization with HCV-NS3-transformed Salmonella: induction of HCV-specific CTL in a transgenic mouse model. Gastroenterology 2001; 121: 1158–66
Satoi J, Murata K, Lechmann M, et al. Genetic immunization of wild-type and hepatitis C virus transgenic mice reveals a hierarchy of cellular immune response and tolerance induction against hepatitis C virus structural proteins. J Virol 2001; 75: 12121–7
Nemchinov LG, Liang TJ, Rifaat MM, et al. Development of a plant-derived subunit vaccine candidate against hepatitis C virus. Arch Virol 2000; 145: 2557–73
Bartholomew RM, Carmichael EP, Findeis MA, et al. Targeted delivery of anti-sense DNA in woodchuck hepatitis virus-infected woodchucks. J Viral Hepat 1995; 2: 273–8
Smith RM, Wu GY. Hepatocyte-directed gene delivery by receptor-mediated endocytosis. Semin Liver Dis 1999; 19: 83–92
Ivics Z, Hackett PB, Plasterk RH, et al. Molecular reconstruction of Sleeping Beauty, a Tc1-like transposon from fish, and its transposition in human cells. Cell 1997; 91: 501–10
Yant SR, Meuse L, Chiu W, et al. Somatic integration and long-term transgene expression in normal and haemophilic mice using a DNA transposon system. Nat Genet 2000; 25: 35–41
Tung FYT, Bowen SW. Targeted inhibition of hepatitis B virus gene expression: a gene therapy approach. Front Biosci 1998; 3: a11–5
Kalpana GV. Retroviral vectors for liver-directed gene therapy. Semin Liver Dis 1999; 19: 27–37
Wang L, Takabe K, Bidlingmaier SM, et al. Sustained correction of bleeding disorder in hemophilia B mice by gene therapy. Proc Natl Acad Sci U S A 1999; 96: 3906–10
Strayer DS. SV40-based gene therapy vectors: turning an adversary into a friend. Curr Opin Mol Ther 2000; 2: 570–8
Strayer DS, Zern MA. Gene delivery to the liver using simian virus 40-derived vectors. Semin Liver Dis 1999; 19: 71–81
Ilan Y, Saito H, Thummala NR, et al. Adenovirus-mediated gene therapy of liver diseases. Semin Liver Dis 1999; 19: 49–59
Chirmule N, Hughes JV, Gao GP, et al. Role of E4 in eliciting CD4 T-cell and B-cell responses to adenovirus vectors delivered to murine and nonhuman primate lungs. J Virol 1998; 72: 6138–45
Kafri T, Morgan D, Krahl T, et al. Cellular immune response to adenoviral vector infected cells does not require de novo viral gene expression: implications for gene therapy. Proc Natl Acad Sci U S A 1998; 95: 11377–82
Thummala NR, Ghosh SS, Lee SW, et al. A non-immunogenic adenoviral vector, coexpressing CTLA4Ig and bilirubin-uridine-diphosphoglucuronateglucuro-nosyltransferase permits long-term, repeatable transgene expression in the Gunn rat model of Crigler-Najjar syndrome. Gene Ther 2002; 9: 981–90
Feng M, Jackson Jr WH, Goldman CK, et al. Stable in vivo gene transduction via a novel adenoviral/retroviral chimeric vector. Nat Biotechnol 1997; 15: 866–70
Recchia A, Parks RJ, Lamartina S, et al. Site-specific integration mediated by a hybrid adenovirus/adeno-associated virus vector. Proc Natl Acad Sci U S A 1999; 96: 2615–20
Calos MP. The potential of extrachromosomal replicating vectors for gene therapy. Trends Genet 1996; 12: 463–6
Leblois L, Roche C, Di Falco ND, et al. Stable transduction of actively dividing cells via a novel adenoviral/episomal vector. Mol Ther 2000; 1: 314–22
Acknowledgements
This work was supported in part by the following National Institutes of Health grants: DK 39137 (to Namita Roy-Chowdhury), DK 46057 (to Jayanta Roy-Chowdhury), 1 RO1 A1 42295 (to Marshall S. Horwitz), the Liver Research Core Center (P30-DK 41296) and the Gene Therapy Core of the Seaver Institute of Human Genetics.
The authors acknowledge the contribution of many investigators who have made important contributions to this field, but whose work could not be cited in this limited review. The authors have no conflicts of interest directly relevant to the contents of this review.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Guha, C., Shah, S.J., Ghosh, S.S. et al. Molecular Therapies for Viral Hepatitis. BioDrugs 17, 81–91 (2003). https://doi.org/10.2165/00063030-200317020-00001
Published:
Issue Date:
DOI: https://doi.org/10.2165/00063030-200317020-00001