Abstract
Outbreaks of meningococcal disease have caused devastation worldwide. Effective vaccines have not been used routinely, due to perceived limitations of the duration of effectiveness as well as immunogenicity when administered during infancy. Given the sporadic nature of outbreaks, the optimal use of these vaccines to control both short-term epidemic and endemic meningococcal disease has been the subject of much debate.
Seven economic studies on the use of polysaccharide vaccination strategies help to highlight the relevant epidemiological and economic issues surrounding the decisions for their use. Five of these studies were based in Africa, the region where annual incidence rates can be several orders of magnitude greater than the rest of the world. These studies demonstrated that vaccination against meningococcal disease during outbreak situations is suboptimal given the inability to rapidly immunise populations in a timely fashion in resource-poor areas. However, depending on the disease incidence and the ability to deliver vaccines, the polysaccharide vaccine can be cost effective for preventive strategies when given prior to the start of outbreaks, either through presumptive vaccination or through a modified routine delivery strategy.
Economic analyses of mass immunisation campaigns and modelled routine vaccination suggest that routine use of meningococcal vaccines for preventive strategies could be within the range of cost-effective public health interventions in those regions of the world where meningococcal disease is endemic. This includes the meningococcal belt of Africa, the Sahelian region.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Neisseria meningitidis is a Gram-negative polysaccharide encapsulated organism which causes meningitis, frequently with devastating neurological sequelae and a death rate often exceeding 10%, even with optimal treatment. Infections can also result in limb loss and other neurological deficits. Given its acute sporadic onset and devastating impact in young healthy individuals, mostly <30 years of age, meningococcal infections are among the most feared of the infectious diseases. Although meningococcal disease is rare in infants up to 3 months of age, the incidence gradually increases to a peak at about 1 year of age and declines thereafter. In many developed countries, there is a peak during the late teen years, an age associated with institutional crowding related to the military or higher education. During epidemics of meningococcal meningitis, the incidence increases in all age groups, however the highest incidence is still in children <2 years of age.[1,2]
Meningococcal serogroups A, B and C are responsible for 90% of cases worldwide, the remaining caused by groups W135 and Y. The only practical public health option is prevention through vaccination; however, considerable debates around ideal strategies continue to occur.[3] Studies have demonstrated the efficacy of the currently available vaccines in children,[4] and adults[5,6] for a 1- to 2-year period of follow-up; however, efficacy in infants is unclear. In Africa, the only study evaluating duration of protection showed declines in protective efficacy during a 3-year period when a single dose was given to children aged 1–4 years.[7] Thus, these vaccines clearly provide a means of preventing disease, but are currently used in light of limited available data about efficacy/effectiveness for infants and duration of protection. In general, group A polysaccharide vaccine has been recommended for protection from disease in epidemics,[8] in military training situations and in travellers to areas with high endemicity.[9] Several countries, most notably Egypt and parts of provincial China, have adopted strategies of routinely immunising children at school entry, but these strategies have not been widely adopted despite evidence of their effectiveness.[10,11]
For at least the past 90 years, group A meningococcal meningitis epidemics have ravaged the African meningitis belt, an area stretching from Senegal to Ethiopia.[12–14] In Africa, even with optimal medical treatment, case fatality rates may be as high as 30%[15] and cause a substantial proportion of survivors to have permanent neurological disability.[16,17] During 1996, the largest outbreak ever recorded occurred in this area.[18] The reported 178 450 cases, and the suboptimal implementation of emergency immunisation campaigns, led to a re-evaluation of meningococcal disease prevention strategies in this area. For example, Robbins et al.[3] called for immediate mass immunisation, followed by a routine immunisation programme of four doses of group A polysaccharide vaccine given during the first 5 years of life. Others[19] have suggested routine immunisation of school children or improvement of the current implementation strategy of emergency response with mass immunisation.
1. Meningococcal Vaccines
Most licensed meningococcal polysaccharide vaccines are formulated as monovalent group A, bivalent groups A and C, or as quadrivalent groups A, C, Y and W135. Recently, meningococcal group C conjugate vaccines that offer long-term protection have been licensed. Until recently, all major epidemics of meningitis throughout the world, including those in Africa, have been caused by group A meningococci. However, group C disease can also occur in Africa,[20] and recently W135 has been implicated in a major outbreak in that continent.[21]
The three major serogroups — A, B and C — differ in their elicitation of an immune response. While group B is thought to be less immunogenic,[22] one dose of group A or C meningococcal polysaccharide vaccine can elicit long-lived protective antibody levels in individuals older than 6 years of age.[23–25] Although infants at 3 months of age are unresponsive to vaccination, they can respond to a booster dose of group A polysaccharide to elicit protective levels until they reach 2 years of age.[24,26] A booster dose at age 2 years elicits antibodies that offer protection to age 5 years when another booster can elicit long-lived protective levels of group A antibodies.[27] In contrast, group C polysaccharide vaccine given during infancy results in suppression of the antibody response; accordingly, it is not indicated before the age of 2 years.[28] After 2 years of age, group C polysaccharide vaccine induces protective antibody levels that decline to normal levels so that another injection is required at about 5 years of age. These findings have been confirmed in African infants and children.[28–30] As a result of these and other comprehensive studies, there has been a safe, inexpensive and effective vaccine for group A meningococci since 1975 that has been licensed by the US and many other countries, and certified by the WHO.[28]
Despite the availability of vaccines, there has been considerable controversy over the optimal strategy for their use. Selection of the appropriate prevention strategy from several possible options should compare, among other things: (i) the local incidence of cases, deaths and disability; (ii) potential disease prevented; (iii) operational capabilities, including human resources; (iv) costs; and (v) practicality. Given the sporadic timing of outbreaks, the operational difficulties to deliver vaccines and the lack of agreement on the duration of protection, policy-makers have increasingly turned to modelling the cost effectiveness of various strategies. In this review, we evaluate the economic studies of alternative control strategies. The results highlight resources required and benefits gained from each of these strategies, and illustrate areas in which additional information is critical.
2. Method of Review
This review identifies and assesses published literature pertaining to the economic analyses of vaccines for the control of epidemic and endemic meningococcal meningitis. Literature searches were conducted using the following key terms: ‘meningococcal meningitis’, ‘cost’, ‘economics’, ‘vaccines’, ‘routine immunisations’, and ‘outbreaks’ through to May 2001. The literature searches resulted in a total of 28 articles, seven of which were identified as specifically addressing the economic evaluation of meningococcal meningitis immunisation.[31–37] These seven are the focus of this review. Of the remaining 21 articles, seven were evaluations of the financial and health-related outcomes of treatment strategies. The remaining 14 articles explored the epidemiology, surveillance and policy aspects concerning meningococcal meningitis[38–51] and were excluded therefore from the review as they were not principally economic analyses.
2.1 Selection of Articles
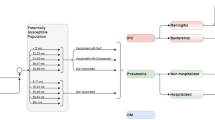
The seven economic studies reviewed were all conducted after 1991 — six since 1996. With two exceptions, the studies addressed economic aspects of meningococcal meningitis within developing countries, primarily in Africa. The types of economic analyses reviewed included cost-benefit, cost-effectiveness and cost analyses of vaccine development and vaccination strategies (table I). Comparable economic estimates between the seven studies were identified as follows: cost per vaccination, cost per case treatment, cost per prevented outcome (deaths vs treatment) and the vaccine-preventable fraction of deaths and cases (table II). The various strategies evaluated included: (i) mass immunisation campaigns where targeted populations are vaccinated in response to a declared outbreak; (ii) routine immunisations; (iii) a combination of mass and routine vaccination; and (iv) preventive immunisation, where targeted populations are vaccinated in anticipation of an outbreak. Strategies involving the vaccination of travellers to endemic areas were not reviewed nor were studies evaluating the recently licensed meningococcal group C conjugate vaccine, exclusively used in several developed countries. Each of the seven studies in which the meningococcal polysaccharide serogroup A vaccine was used are reviewed.
Results of economic studies of meningococcal vaccination strategies using meningococcal serogroup A vaccine (see also table I). All costs are in US dollars, based on year of study
3. Cost Effectiveness of Vaccine Development
An analysis undertaken by Musgrove[31] sought to justify the expenditure of funds for the development of new vaccines against meningitis, pneumonia and typhoid. The author estimated the costs and benefits to develop and disseminate vaccines by the Pan American Health Organisation (societal perspective). Vaccine development was estimated to take 10 years.
This progressive study was comprehensive in that it included the cost to develop these vaccines for the region as well as the costs of vaccine purchase and administration. Amongst the assumptions was a 20- to 30-year time frame to develop a 90% effective vaccine for at least 19.5 million persons with an incidence of meningitis of 10–50 per 100 000. Case fatality rates were assumed to be 5% and 50% with and without treatment, respectively. Case treatment was assumed to average $US3000 (year 1992 values). Discount rates between 8% and 15% were used, with 10% for the base case.
Given these parameters, the point estimate for a break-even cost for a vaccine from the societal perspective was $US0.27. This, however, did not include development costs and did not include a willingness to pay to prevent morbidity and mortality. A cost-effectiveness study would yield a higher acceptable vaccine price as it would reflect what society would be willing to pay to prevent morbidity and mortality.
3.1 Preventative Vaccination in College Populations
Jackson et al.[32] performed a cost-benefit analysis in order to examine whether students in US colleges should receive routine immunisations against meningococcal disease. The authors calculated the number of meningococcal cases that would occur over a 4-year period, both with and without implementing an immunisation programme upon college entry. The authors stated the following assumptions: (i) vaccine efficacy and vaccine coverage were assumed to be 85% and 80%, respectively; (ii) the vaccine was estimated to cost $US15 (1995 value) per dose, with an additional cost of $US15 per administration; (iii) treatment of each case of meningococcal disease or severe systemic vaccine reaction (1 per 100 000 vaccines) was estimated to cost $US8145 and $US1830, respectively; and (iv) a fatality rate of 15%. At the time, the annual rate of vaccine-preventable meningococcal disease among 18- to 22-year-olds was estimated to be 0.5/100 000. Indirect costs of the value of potential future earnings lost due to premature death were included. The authors used a 4% discount rate.
The authors estimated the cost of a routine immunisation programme against meningococcal meningitis to be $US56.2 million. At a student rate of disease of 15 times that of baseline, the savings resulting from the prevention of premature death were adequate enough to result in net savings of $US7.6 million. The authors estimated that the student rate of disease must be at least 13 times that of baseline before the cost of a routine immunisation strategy among college students would be offset by the savings from prevention.
By using varying multiples of the baseline rate of disease, the authors took into consideration the uncertainty of the specific rate of disease among college students. The authors also conducted sensitivity analyses in order to vary the probabilities for which adequate data were not available. The authors concluded that the rate of meningococcal disease among college students was not high enough to warrant the cost of the immunisation programme. However, additional costs resulting from care of survivors with long-term sequelae were not included and therefore the study underestimated all potential benefits.
3.2 Treatment Versus Outbreak Response
To assess both case management and mass vaccination strategies during a 1995 meningitis epidemic in northern Nigeria, Veeken et al.[33] conducted a cost-effectiveness/cost analysis of the non-governmental organisation Medecin sans Frontieres (MSF)-supported activities in Katsina state. The MSF support consisted primarily of the following three segments: (i) immediate treatment and medium-term case management of meningitis patients; (ii) establishment of a surveillance system; and (iii) mass vaccination for certain populations. In Katsina, MSF treated 10 117 persons (48%) out of a total of 20 927 treated meningitis cases and vaccinated 509 104 of the 930 000 people who received vaccination. To calculate the ‘impact’ of the mass vaccination campaign in Katsina, the authors estimated the number of meningitis cases prevented as a result of the vaccination efforts. Using a previously described method,[52] the number of meningitis cases that occurred was compared with a projection of the number of cases that would have occurred in the absence of a vaccination campaign. With regard to the impact of MSF-supported treatment and case management, the authors estimated the number of deaths prevented by taking the product of the number of treated cases and the difference in the case fatality rate between treated and untreated populations.
The cost per vaccination in Katsina state was $US0.64 (1996 value), and the average cost of treatment of a meningitis case was $US35, with the cost of drugs accounting for over half of the amount. Although case management and mass vaccination were noted to be efficient, there was a notable difference in the cost effectiveness of the two strategies. With the introduction of MSF-supported treatment and case management, the case fatality rate was reduced from 17% to 8%. Under the assumption of a vaccine efficacy of 85%, the authors estimated that the vaccination campaign resulted in a 3.3% reduction in the number of cases (ranging between 2% and 17%), whereas the curative activities resulted in a 36% reduction in mortality. The estimate for the number of meningitis cases prevented by vaccines was based on the absence of a herd effect-protection to non-vaccinated persons through the reduction of carriage and transmission. The authors concluded that given the rapid nature of meningitis epidemics, in conjunction with the fact that MSF-supported mass immunisation began late in the course of the epidemic, it would have been more cost effective to refrain from vaccinating the afflicted populations. Specifically, the authors calculated the cost per death prevented as $US83–$US396 for treatment and $US6000 for reactive vaccination. No long-term treatment costs or discount rate was given.
The authors noted that during meningitis epidemics there is a pressure to vaccinate, and although programmes are frequently delayed, vaccination is a precondition for gaining access to implement curative services. The study did not account for local staff time and expense to administer medication and therefore underestimated the cost of treatment. Furthermore, comparisons were made with vaccination during an outbreak, which is bound to be less efficient than preventive vaccination. The effectiveness of vaccination programmes are highly dependent on the implementation rate and timing prior to the outbreak.
3.3 Campaigns in Response to Analysis of Vaccine
In an analysis conducted by Varaine et al.,[34] mass immunisation campaigns with meningococcal A/C polysaccharide vaccines were assessed for the epidemics occurring in Niger, Burundi and Guinea in 1991, 1992 and 1993, respectively. In Niger, the target population of a vaccination campaign was the population living within a 5km radius of villages where cases were notified. In Burundi, the goal was to immunise the entire population over 1 year of age. The target population in Guinea was the population over 1 year of age in sub-districts where the weekly incidence rate exceeded 5/100 000. An estimate of prevented cases from vaccination was derived from a mathematical model. The authors also analysed the sensitivity and specificity of various epidemic alert ‘thresholds’ which initiate a response to mass vaccinate.
In Guinea, the estimated cost of the vaccination campaign was $US322 000 (1993 value). With an assumed vaccine efficacy of 85%, the vaccine-preventable fraction of cases for the population was 35–42% in urban areas and 16% in rural areas. The prevented number of cases was 1348, and the estimated cost per case prevented was $US240. The allocation of cost for the vaccination campaign was as follows: 59% vaccines, 14% injection materials, 16% logistics and 11% wages. No discount rate was provided.
In all three countries, both disposable syringes and jet injectors were used to administer vaccine. The cost of the campaign in rural areas was an estimated 50% of the total cost. The authors concluded that meningococcal A/C polysaccharide mass vaccination is an efficient method of controlling an outbreak, given that vaccination is completed within 4–6 weeks following the threshold number of cases. This type of response, however, requires adequate surveillance, preparation and infrastructure to respond.
3.4 Three Studies on Routine Vaccination Strategies Versus Outbreak Response
The study by Miller et al.[35] modelled 50 years of reported meningitis data from 16 countries to estimate the specific-country impact of various strategies including a single vaccination dose preventive, four-dose routine and outbreak response. Weekly specific incidence data for four districts from 7 years were used to model an outbreak response. Vaccine costs were assumed to be $US0.18 (1998 value) per dose with differential costs allocated for method of administration (routine or campaign) and whether the vaccine was administered with other vaccines in national programmes. A discount rate of 3% was used for costs and benefits.
For the routine vaccination strategies, the cost per death prevented ranged from $US1125 in Niger to $US71 660 in Mauritania, with 10–45% of deaths prevented depending on current coverage rates with other vaccines. These ranges were highly dependent on disease incidence. In 14 of the 16 countries studied, routine vaccination would be considered cost effective based on a year of life saved costing less than the average per capita gross domestic product. The effectiveness (and hence cost effectiveness) of the outbreak response was variable, based on: (i) various threshold incidence values to trigger a response; (ii) coverage rates; and/or (iii) the number of weeks delay between the recognition of an outbreak and the onset of a response.
The study highlighted the limitations and inadequacies of the current outbreak control strategies and explored the feasibility of routine vaccination. For the three strategies studied, an overall effective prevention beyond 42% could not be achieved because of the weak infrastructures to deliver vaccine to infants and children in the region, and the challenges in most countries to adequately respond in a timely fashion to the current threshold incidence of 15/100 000 for 2 weeks. Lowering the threshold to trigger a vaccination response would prevent more cases. Given the current high meningitis incidence levels in many countries in the regions, routine vaccination should be seriously considered in those countries with highest incidence.
Similar to Miller et al.,[35] Bovier et al.[36] modelled various vaccination strategies. Routine vaccination and a combination of routine/reactive vaccination was compared with the current WHO-recommended reactive vaccination. Relative to the current WHO strategy, routine vaccination and the combined programme would cost $US50/QALY (1999 value) and $US199/QALY, respectively. The incremental cost per averted death was $US1161 and $US2397, respectively. The analysis was sensitive to disease incidence, treatment and vaccine administrative costs and the effectiveness of mass campaign approaches. The cost to add a dose outside of the routine national vaccine programme schedule and in a campaign was estimated at $US1.03 (range of $US0.5–$US5) and $US0.83 (upper limit $US10), respectively. A 3% discount rate was used. The assumption for coverage for routine vaccination of 5-year-olds was 50%, although most countries in the meningitis belt report coverage of 25–40% at best for the combined diphtheria tetanus and pertussis (DTP) and measles vaccines. Real coverage rates are likely to be much lower, especially for vaccines given outside of current routine schedules. Given that there is no current programme for school-based vaccination at 5 years, major infrastructure improvements for vaccination would be required to achieve a minimum 50% coverage. Outbreak coverage has been documented to be 60–80%.[34]
Parent du Chatelet et al.[37] formulated a cost-effectiveness model to compare two vaccination strategies for controlling a meningococcal meningitis epidemic in Matam, Senegal: a mass preventive campaign targeting individuals 1–25 years of age and a reactive campaign targeting persons 1–30 years of age. For the preventive campaign, the cost of the A/C polysaccharide vaccination was estimated, from an actual campaign, to be $US0.38 per dose administered. For the reactive campaign, the cost of vaccination was estimated to be $US0.51–$US0.64 (2001 values) per dose administered. Vaccination coverage was estimated to be 86–92% for the preventive campaign and 74–79% for the reactive campaign. Costs and health outcomes were discounted at 3% (1–5% in the sensitivity analysis). Only direct costs were included in the analysis.
Preventive vaccination resulted in lower costs and a greater number of meningococcal disease cases prevented than a reactive campaign, as long as the following conditions were maintained (see table II): vaccination coverage in the preventive and reactive campaign was at least 71% and <94%, respectively; and the interval between the preventive campaign and the expected epidemic was <36 months. Compared with no intervention, preventive and reactive vaccination strategies resulted in a 59% and 49% reduction in cases, and a 57% and 47% reduction in deaths, respectively.[37] Further study results are included in table II.
The analysis of Parent du Chatelet et al.[37] offers notable insights into the benefits of implementing a preventive mass immunisation campaign against meningococcal disease. A recognised shortcoming of conducting reactive mass immunisation strategies in African countries is the lack of effective surveillance systems. Often, the threshold level of meningococcal meningitis cases is exceeded long before a reactive mass immunisation campaign is implemented. Thus, although the authors address the limitations of generalising results derived from a relatively small region, the decision to perform analyses of vaccine campaigns conducted in Matam — a region that lacks sufficient surveillance systems — does take into account a recurring dilemma that many African countries face. Additionally, the authors’ assumption that a reactive campaign would not begin as soon as the threshold level was passed also takes into consideration the reality of many epidemic situations in Africa.
Ultimately, the authors concluded that while the development of an effective meningococcal conjugate A/C vaccine offers the prospect of a truly effective method of control and prevention, preventive mass immunisations with the polysaccharide vaccine currently represents the most effective method for reducing morbidity and mortality.
4. Discussion
The utilisation of meningococcal polysaccharide vaccines to manage epidemics, especially for use in Africa, has been a topic of much debate. The strategy of mass vaccination has been regarded as ineffectual for several reasons. Meningococcal epidemics can accelerate rapidly to uncontrollable levels of disease and, in the past, mass vaccinations have almost always been initiated too late to be effectual.[53] Although guidelines have been established to deliver a pre-emptive strike against impending epidemics, if the early threshold warnings are to be of assistance then both the vaccine supplies and the necessary logistics must be readily available. Given the limited resources of many developing countries — particularly in Africa — it is usually difficult to meet such conditions. The abrupt manner in which a mass vaccination strategy is implemented can also be very disruptive to standard health programmes such as national routine vaccination programmes.
The great reluctance by the WHO to advocate routine vaccine use is based on the belief that meningococcal polysaccharides vaccines have a limited duration of protection against a disease that appears with an erratic periodicity. However, this needs to be balanced against the fact that outbreaks are appearing with greater frequency and the belief by others in the scientific community of the potential to achieve long-lasting immunity, albeit with more complex administration regimens.[54]
Although this is a review of the economic value of vaccination against meningococcal disease, it helps to elucidate the most critical parameters that have an impact on policy. In a number of other diseases, routine vaccination has been shown to be cost effective.[55] However, there is considerably more debate about the effectiveness of various control strategies for N. meningitidis disease, and more uncertainty of the locale-specific meningitis incidence than the economic factors that can influence policy.
Common to all the analyses reviewed in this paper are the models which measure the effectiveness of strategies. All these models require numerous assumptions related to the nature of meningococcal epidemics, their frequency, geographic expansion and appearance of new strains. Most of the analyses have attempted to weigh the merits of routine vaccination versus outbreak response based on three assumptions: polysaccharide vaccines do not give long-lasting immunity when given during infancy; polysaccharide vaccines have a limited duration of efficacy; and the infrastructure to deliver vaccines either by a campaign or routinely is weak in many parts of Africa. However, during the past 20–30 years, the nature of meningococcal epidemics has changed dramatically in Africa. The traditional meningitis belt has expanded to encompass many other countries, epidemics occur on a 1- to 2-year cycle compared with the previous 8- to 12-year cycles, and new serotypes such as W135 are emerging. In addition, there remains active debate about the duration of protection afforded, at various ages, by polysaccharide vaccine when given as a single dose by low-resourced programmes in outbreak situations.
4.1 Duration of Group A Meningococcal Polysaccharide Vaccine-Induced Immunity
As all the current strategies are dependent on the assumption that meningococcal polysaccharide vaccines have a limited duration of efficacy, it is worth exploring the evidence for this assumption further. Rheingold et al.[7] conducted a case-control study in the mid 1980s in Burkina Faso that assessed the duration of protection in subsequent outbreaks in a previously vaccinated population. A major limitation to the study was that it was a post-licensure observational study with incomplete records as to who was vaccinated with the correct number of doses, as recommended by the label insert. The measures of effectiveness and duration of protection were contrary to the efficacy that had been shown in the clinical trials.[4–6] Although effectiveness frequently indicates the impact when vaccine is used in real-life conditions, one may want to question the continued reliance on a policy based on limited data in light of other evidence for the control of meningitis in other countries such as China.[10,11]
4.2 Infrastructure Issues
There have been numerous analyses of the operational difficulties of delivering vaccines in emergency situations. The complexities of conducting surveillance and analysis of meningococcal disease rates and then implementing a response must be balanced against the complexities of routinely vaccinating with polysaccharide vaccine using a novel vaccination schedule. Either choice is complex; however, it is known that the emergency response mode has frequently failed.[56]
There are also a number of additional problems that can result from a mass vaccination strategy during meningitis epidemics. For example, consider the insufficient supply of syringes that necessitated the use of Ped-o-Jet® Footnote 1 injectors for vaccination during the 1996 Nigerian meningitis epidemic[54] and the frequent use of vaccine delivered from 50-dose vials. It may never be known how many blood-borne pathogens, including hepatitis B and C viruses and HIV, that were transmitted as a result of the need to rapidly respond without adequate supplies; these are hidden costs.[57]
Furthermore, exploitation of emergency-response situations has resulted in the disastrous use of counterfeited vaccine. During the 1995 epidemic in Niger, an MSF team working with local health authorities noticed that the vaccines from Nigeria had an unusual appearance. Once inquiries were made, it became apparent that the vaccines were counterfeit — approximately 60 000 persons were vaccinated with the fake vaccines.[58]
Any economic or decision analysis should clearly articulate the limited data and assumptions about the biomedical (i.e. characteristics of the vaccine) and operational issues.
4.3 The Current Status and Future Potential of Meningococcal Meningitis Vaccines
In Niger, N. meningitidis infections cause an approximate annual endemic rate of 30 cases per 100 000 population. While 85% of meningococcal cases are due to serogroup A meningococci, the remaining cases are due to serogroup C. In a study conducted in Niger on the safety and immunogenicity of three doses of a N. meningitidis A + C diphtheria conjugate vaccine in infants, the results supported the hypothesis that conjugate vaccines are able to induce immunological memory in young children.[59] Overall, conjugated meningococcal polysaccharide vaccines have been found to be well tolerated, adverse reactions have been mild and infrequent.[59] Further studies regarding the future potential of meningococcal conjugate vaccines must be conducted in order to determine the necessary administration schedule, the duration of protective immunity conferred by the vaccine and the strength of immunological memory to the group A component relative to the number of necessary doses.
5. Conclusion
Economic studies help to define the implicit value of alternative treatment strategies and help to quantify the importance of the uncertainty amongst numerous data assumptions, including both the biological and operational features of prevention strategies. Vaccines against meningitis have been shown to effectively control or to eliminate meningitis in regions which have utilised them routinely. The scalability of routine vaccination with existing polysaccharide vaccines in Africa faces the challenge of operational capabilities and the need to find financial resources. Although new technologies, such as conjugate vaccines, may alleviate some of those challenges, it would still be cost effective to utilise existing vaccines more strategically.
Notes
The use of trade names is for identification purposes only and does not imply endorsement.
References
Peltola H, Kataja JM, Makela PH. Shift in the age distribution of meningococcal disease as predictor of an epidemic? Lancet 1982; 11: 595–7
Spanjaard L, Bol B, deMarie S, et al. Age distribution of meningococcal disease as predictor of epidemics. Lancet 1982; II: 1039–40
Robbins J, Towne DW, Gotschlich EC, et al. [’Love’s labours lost’: failure to implement mass vaccination against group A meningococcal meningitis in sub-Saharan Africa. Lancet 1997; 350: 880–2
Peltola H, Makela PH, Kayhty H, et al. Clinical efficacy of meningococcus group A capsular polysaccharide vaccine in children three months to five years of age. N Engl J Med 1977; 297: 686–91
Gotschlich EC, Goldschneider I, Artenstein MS. Human immunity to the meningococcus: IV. Immunogenicity of the group A and group C polysaccharides in human volunteers. J Exp Med 1969; 129: 1367–84
Frasch CE. Vaccines for prevention of meningococcal disease. Clin Microbiol Rev 1989; 2 Suppl.: S134–8
Reingold AL, Broome CV, Hightower AW, et al. Age-specific differences in duration of clinical protection after vaccination with meningococcal polysaccharide A vaccine. Lancet 1985; II (8447): 114–8
World Health Organization Working Group. Control of epidemic meningococcal disease. WHO practical guidelines. 2nd ed. Geneva: World Health Organization, 1998
Centers for Disease Control. Recommendation of the Immunization Practices Advisory Committee: meningococcal vaccines. MMWR 1985; 34: 255-9
Zhiqian M. Observation on the epidemiologic efficacy for 9 years on epidemic meningococcal polysaccharide vaccine of group A by district immunization method. Zhonghua Liu Xing Bing Xue Za Zhi 1991; 12: 69–71
Win JJ. Changes in epidemic features of epidemic cerebrospinal meningitis after vaccination with purified meningococcal polysaccharide vaccine group A in Zhengzhou. Zhonghua Yu Fang Yi Xue Za Zhi 1993 May; 27 (3): 160–1
Lapeyssonnie L. La meningite cerebrospinale en Afrique. [Cerebrospinal meningitis in Africa]. Bull World Health Organ 1963; 28 Suppl.: 1–100
Greenwood BM. Epidemiology of meningitis in tropical Africa. In: Williams JD, Burnie J, editors. Bacterial meningitis. 1st ed. London: Academic Press Inc., 1987: 61–91
Greenwood BM, Blakebrough IS, Bradley AK, et al. Meningococcal disease and season in sub-Saharan Africa. Lancet 1984; 1 (8390): 1339–42
Campagne G, Schuchat A, Djibo S, et al. Epidemiology of bacterial meningitis in Niamey, Niger, 1981-96. Bull World Health Organ 1999; 77: 499–508
Merlin M, Martet G, Debonne JM, et al. Controle d’une epidemie de meningite a meningocoque en Afrique centrale. [Control of an epidemic of meningococcal meningitis in Central Africa]. Same 1996; 6: 87–95
Heyman SN, Ginosar Y, Niel L, et al. Meningococcal meningitis among Rwandan refugees: diagnosis, management, and outcome in a field hospital. Int J Infect Dis 1998; 2: 137–42
Tikhomirov E, Santamaria M, Esteves K. Meningococcal disease: public health burden and control. World Health Star Q 1997; 50: 170–7
Minutes of a WHO informal consultation on operational research on immunization prevention and control strategies for meningococcal disease; 1997 Feb 18-19; Annecy, France. Geneva: World Health Organization. WHO/EMC.97.2
Moore PS, Plikaytis BD, Bolan GA, et al. Detection of meningitis epidemics in Africa: a population-based analysis. Int J Epidemiol 1992; 21: 155–62
Taha MK, Parent Du Chatelet I, Schlumberger M, et al. Neisseria meningitidis serogroups WI 35 and A were equally prevalent among meningitis cases occurring at the end of the 2001 epidemics in Burkina Faso and Niger. J Clin Microbiol 2002 Mar; 40 (3): 1083–4
Wyle FA, Artenstein MS, Brandt BL, et al. Immunologic response of man to Group B meningococcal polysaccharide vaccines. J Infect Dis 1972; 126: 514–22
Kayhty H, Karanko V, Peltola H, et al. Serum antibodies to capsular polysaccharide vaccine of group A Neisseria meningitidis followed for three years in infants and children. J Infect Dis 1980; 142: 861–8
Mohammed I, Onyemelukwe GC, Obineche EN, et al. Control of epidemic meningococcal meningitis by mass vaccination: II. Persistence of antibody four years after vaccination. J Infect 1984; 9: 197–202
Zangwill K-M, Stout RW, Carlone GM, et al. Duration of antibody response after meningococcal polysaccharide vaccination in US Air Force personnel. J Infect Dis 1994; 169: 847–52
Gold R, Lepow ML, Goldschneider I, et al. Kinetics of antibody production to group A and group C meningococcal polysaccharide vaccines administered during the first six years of life: prospects for routine immunization of infants and children. J Infect Dis 1979; 140: 690–7
Kayhty H, Karanko V, Peltola H, et al. Serum antibodies to capsular polysaccharide vaccine of group A Neisseria meningitidis for three years in infants and children. J Infect Dis 1980; 142: 861–8
WHO Technical Report Series. Requirements for meningococcal polysaccharide vaccine. Requirements for Biological Substances No. 23. 1976; 594: 50-75
MacLennan J, Obaro S, Deeks J, et al. Immune response to revaccination with meningococcal A and C polysaccharides in Gambian children following repeated immunization during early childhood. Vaccine 1999; 17: 3086–93
Lieberman JM, Chin SS, Wong VK, et al. Safety and immunogenicity of a serogroup A/C Neisseria meningitidis oligosaccharide-protein conjugate vaccine in young children: a randomized controlled trial. JAMA 1996; 275: 1499–503
Musgrove P. Cost-benefit analysis of a regional system for vaccination against pneumonia, meningitis type B, and typhoid fever. Bull Pan Am Health Organ 1992; 26 (2): 173–91
Jackson LA, Schuchat A, Gorsky RD, et al. Should college students be vaccinated against meningococcal disease? A costbenefit analysis. Am J Public Health 1995 Jun; 85 (6): 843–5
Veeken H, Ritmeijer K, Hausman B. Priority during a meningitis epidemic: vaccination or treatment? Bull World Health Organ 1998; 76 (2): 135–41
Varaine F, Caugant DA, Rion JY, et al. Meningitis outbreaks and vaccination strategy. Trans R Soc Trop Med Hyg 1997 Jan-Feb; 91 (1): 3–7
Miller MA, Wenger J, Rosenstein N, et al. Evaluation of meningococcal meningitis vaccination strategies for the meningitis belt in Africa. Pediatr Infect Dis J 1999 Dec; 18 (12): 1051–9
Bovier PA, Wyss K, An HJ. A cost-effectiveness analysis of vaccination strategies against N. meningitidis meningitis in sub-Saharan African countries. Soc Sci Med 1999 May; 48 (9): 1205–20
Parent du Chatelet I, Gessner BD, da Silva A. Comparison of cost-effectiveness of preventive and reactive mass immunization campaigns against meningococcal meningitis in West Africa: a theoretical modeling analysis. Vaccine 2001 May 14; 19 (25-26): 3420–31
De Wals P, Dionne M, Douville-Fradet M, et al. Impact of a mass immunization campaign against serogroup C meningococcus in the Province of Quebec, Canada. Bull World Health Organ 1996; 74 (4): 407–11
Dure-Samin A, Mubina A, Azra Y. An epidemic of meningococcal disease in Karachi (Pakistan): a study of children. Acta Paediatr Jpn 1991 Jun; 33 (3): 352–6
Frasch CE. Prospects for the prevention of meningococcal disease: special reference to group B. Vaccine 1987 Mar; 5 (1): 34
Fogarty I, Cafferkey MT, Moloney AC. Meningococcal disease in the Republic of Ireland: 1995. Commun Dis Rep CDR Rev 1997 Jan 10; 7 (1): R9–13
Gordon SM. Should all college-bound freshmen receive meningococcal vaccine?. Cleve Clin J Med 2001 Jan; 68 (1): 9–10
Aboal Vinas JL, Farjas Abadia P, Zubizarreta Alberdi R, et al. Meningococcal C disease epidemic in Galicia 1996: the decision making process. Gac Sanit 1999 Jan-Feb; 13 (1): 62–9
Cochi SL, Markowitz LE, Joshi DD, et al. Control of epidemic group A meningococcal meningitis in Nepal. Int J Epidemmil 1987 Mar; 16 (1): 91–7
Greenwood BM. Treatment and prevention of meningococcal disease. Trop Doct 1984 Apr; 14 (2): 61–6
Greenwood BM, Wali SS. Control of meningococcal infection in the African meningitis belt by selective vaccination. Lancet 1980 Apr 5; 1 (8171): 729–32
Saxena SN, Rawal IJ, Tripathi KK, et al. Meningococcal vaccines in prevention and control of meningitis. Indian Pediatr 1985 Jun; 22 (6): 453–65
Binkin N, Band J. Epidemic of meningococcal meningitis in Bamako, Mali: epidemiological features and analysis of vaccine efficacy. Lancet 1982 Aug 7; II (8293): 315–8
Report of the first hemispheric meeting on meningococcal disease. Bull Pan Am Health Organ 1976; 10 (2): 163-76
Rey M, Lafaix C, Mar ID, et al. Epidemiologic aspects of purulent meningitis in tropical Africa (1052 cases observed in Dakar). Lyon Med 1972 Nov 26; 228 (18): 503–8
Spanjaard L, Bol P, Ekker W, et al. The incidence of bacterial meningitis in The Netherlands: a comparison of three registration systems, 1977-1982. J Infect 1985 Nov; 11 (3): 259–68
Pinner RW, Onyango F, Perkins BA, et al. Epidemic meningococcal disease in Nairobi, Kenya, 1989. J Infect Dis 1992; 166: 359–64
Lewis R, Nathan N, Diana L, et al. Timely detection of meningococcal meningitis in epidemics in Africa. Lancet 2001; 358: 287–93
Robbins JB, Schneerson R, Gotschlich EC. A rebuttal: epidemic and endemic meningococcal meningitis is sub-Saharan Africa can be prevented now by routine immunization with group A meningococcal capsular polysaccharide vaccine. Pediatr Infect Dis J 2000; 19 (10): 945–53
Miller MA, Hinman A. Economic analyses of vaccine policies. In: Plotkin S, Orenstein W, eds. Vaccines. 4th ed. Philadelphia (PA): WB Saunders Co, 2003: 1463–90
Mohammed I, Nasidi A, Alkali AS, et al. A severe epidemic of meningococcal meningitis in Nigeria, 1996. Trans R Soc Trop Med Hyg 2000; 94: 265–70
Miller MA, Pisani E. The cost of unsafe injections. Bull World Health Organ 1999; 77 (10): 808–11
Pecoul B, Chirac P, Trouiller P, et al. Access to essential drugs in poor countries: a lost battle? JAMA 1999 Jan 27; 281 (4): 361–7
Campagne G, Garba A, Fabre P, et al. Safety and immunogenicity of three doses of a Neisseria meningitidis A + C diphtheria conjugate vaccine in infants from Niger. Pediatr Infect Dis J 2000 Feb; 19 (2): 144–50
Acknowledgements
At the time of writing the authors were US federal employees without any declared conflicts of interest. This work was sponsored by the National Institutes of Health, Fogarty International Center, Bethesda (MD), USA.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Miller, M.A., Shahab, C.K. Review of the cost effectiveness of immunisation strategies for the control of epidemic meningococcal meningitis. Pharmacoeconomics 23, 333–343 (2005). https://doi.org/10.2165/00019053-200523040-00004
Published:
Issue Date:
DOI: https://doi.org/10.2165/00019053-200523040-00004